: Reading time:
What are the characteristics of a diagnosis of “schizotypal disorder”, how does it differ from schizophrenia and how is schizotypal disorder treated – says Irina Valentinovna Shcherbakova, Doctor of Medical Sciences, Professor, Psychiatrist.
Until the nineties of the last century, schizotypal disorder was known as “sluggish schizophrenia” or “slow-onset” (“pre-schizophrenia”, “mild schizophrenia”, “pseudo-neurotic schizophrenia”). It is a relatively benign, slowly progressive endogenous process that occurs in one third of all patients with schizophrenia. In the current ICD-10 classification of mental disorders, schizotypal disorder is an independent diagnosis, isolated from schizophrenia. It includes a group of functional mental disorders that occupy an intermediate position between schizophrenia and personality pathology.
In the current ICD-10 classification of mental disorders, schizotypal disorder is an independent diagnosis, isolated from schizophrenia.
Schizotypal disorder includes individuals with impairments in interpersonal functioning, cognition, emotion, and behavioral control who exhibit a genetic predisposition to schizophrenia, so-called “hidden carriers.” The latter are family members of patients with schizophrenia and are distinguished by chronic peculiarities of thinking and communication, and low social activity.
The first signs of schizotypal disorder appear in childhood or adolescence. The provocation that triggers the disease can be psychological stress. Schizotypal disorder is characterized by a gradual, usually imperceptible onset, the absence of pronounced exacerbations and defined remissions, and is chronic and continuous.
As the disease progresses, there is a gradual decline in working capacity associated with a decline in intellectual activity and initiative, impoverishment of emotions and contacts, and deepening social isolation. At the same time, about 30% of patients with schizotypal disorder continue to work, choosing lighter, home-based types of work activities that are more acceptable to them; Some patients become dependents and disabled.
Main symptoms of schizotypal personality disorder
The clinical signs of schizotypal disorder are varied, but some of them are fundamental for diagnosis:
strange beliefs, speech;
strange or magical thinking;
unusual sensations and bodily illusions;
suspiciousness or paranoid thoughts (thoughts of persecution);
inappropriate emotions or lack of emotional response (constricted affect);
strange, eccentric or peculiar behavior or appearance;
lack of close friends or confidants other than first-degree relatives;
excessive social anxiety, which does not decrease after dating and is usually associated with paranoid fears.
These signs can be combined into three groups:
- Cognitive-perceptual deficits: strange beliefs, perceptual disturbances, paranoia or suspiciousness
- interpersonal deficits: lack of close friends, social anxiety, paranoia or suspiciousness
- disorganization: unclear speech or thinking, dulled affect, strange behavior
What are personality disorders?
Your personality is your unique way of thinking, understanding, reacting and relating to people. Many people may seem like extraordinary individuals. But they are believed to have a personality disorder
, only if their identity is:
- Causes serious problems at work or school.
- Does not allow them to behave normally towards others.
- It is not something they can change or correct, even if it causes problems.
People with personality disorders usually think that there is nothing wrong with them. They may be upset by the consequences of their personality disorder, such as divorce or job loss. However, they usually believe that these problems are the fault of others rather than themselves. Other people usually have difficulty communicating with a person who has a personality disorder.
Many people with a personality disorder also have other problems, such as:
- Depression
Additional signs
Along with the main above-mentioned signs of schizotypal disorder, the clinical picture also contains other symptoms in both men and women, which are usually found in neurotic diseases, mood, behavioral or personality disorders.
Neurotic manifestations. The most common disorders in schizotypal disorder include anxiety-phobic symptoms - fears, panic attacks, obsessive-compulsive symptoms; heightened introspection, increased reflection, somatoform phenomena, asthenia. There are often cases of painful concern about one’s physical or mental health (hypochondria) or “mysterious” symptoms and diseases that have not been confirmed by specialists.
Eating disorders. Eating disorders, such as anorexia or bulimia, are quite common.
Mood disorders (affective disorders). Concomitant mood disorders are the rule rather than the exception—long-term, shallow depressions or unreasonable mood elevations (euphoria), long-term or short-term, but without psychotic symptoms.
Behavioral disorders. Aggressive, antisocial behavior, absurd actions, and desire disorders in the form of vagrancy, sexual perversions, and alcohol and psychoactive substance abuse may be observed.
Some of the described disorders become permanent or “axial”; others can replace each other or join existing ones, becoming additional, aggravating the patient’s condition.
Depending on the predominance of certain symptoms, there are several main variants of schizotypal personality disorder:
- pseudoneurotic schizophrenia (external resemblance to neurosis)
- pseudopsychopathic schizophrenia (external resemblance to psychopathy)
- schizophrenia, poor in symptoms (characterized by increasing asthenia and decreased ability to work)
- schizotypal personality disorder
- latent schizophrenia
Typical signs
First of all, what catches your eye when you see such patients and what they themselves note is deep apathy, powerlessness, and reluctance to do anything. I just want to lie there, without getting up, all day long.
As the patients themselves note, they are not in the mood. They are neither happy nor sad. It seems as if you have died, but your body is still alive. The girl noted that during especially difficult periods she was so indifferent that she would put out a cigarette on herself in order to awaken even the slightest feelings in herself.
But one feeling still remains - anxiety. She is so strong that it is difficult to control her. However, it cannot be said that it has an emotional connotation. Rather, it should be characterized as internal tension. It is manifested by tachycardia, a feeling of heat inside, dizziness, rapid breathing. To reduce its intensity, a person uses various rituals: walking or swaying from side to side, or picking up an object and starting to turn it over in a stereotypical manner. When anxiety decreases, the patient feels weak and exhausted.
Gradually all emotions begin to fade, first good and then bad. An emotional assessment of any event is given only from a logical point of view: the sun is shining - this is good, the car has an accident - this is bad. The instinct of self-preservation decreases.
As the emotional background becomes impoverished, the ability to sympathize and empathize with others is lost.
The poverty of emotions becomes visible, as they say, is obvious: the person seems detached, there is coldness and indifference in his behavior. There is practically no facial expression, the voice is quiet and monotonous.
On the other hand, emotionlessness is replaced by outbursts of aggression and rage. It is very difficult for patients to control themselves at these moments.
Given such emotional swings, patients with SR find it difficult to communicate with people and make new acquaintances. As a rule, they are reserved, uncommunicative and shy. Others may be overly suspicious and believe that they are being harmed.
The patient's appearance is sometimes quite eccentric. He involuntarily attracts attention. The person dresses strangely, eccentrically, and there are also oddities in his behavior. Thus, the guy noted that at the moment of the “heyday” of the disease he was so consumed by apathy that he walked around in dirty and torn clothes, stopped washing and brushing his teeth.
The thinking of these people is inappropriate. They express crazy ideas, their speech is pretentious and incoherent. Sometimes they lose touch with reality. They find it difficult to maintain attention, and they jump from one topic to another, are persistent in their statements and are confident that they are right.
Patients often become interested in magic and mysticism, believe in miracles and a higher power, start going to church or join sects.
Hallucinations in schizotypal disorder are not as obvious as in schizophrenia, and are rather illusory in nature. For example, a person can clearly hear a conversation in the sound of a running computer. Or a pillar is mistaken for a person.
Derealization is manifested by a feeling of unreality of the environment. Everything around becomes blurry, colors lose their brightness, sounds lose volume. This comes upon the sick suddenly. They understand the absurdity of the situation, and this depresses them even more.
This is how a teenage girl suffering from SPD describes her condition: I have no thoughts at all. In order for them to appear, I begin to tell myself something in my inner voice. As for emotions, as a person, I have a lot of them, but I rarely experience them.
Illusions manifest themselves in the fact that in the face of one person I see the features of a completely different person. Sometimes I can see objects that are not really there. Cases of derealization are always sudden and unpredictable for me. At the same time, I feel like I’m in a dream. I went to another city. And suddenly, sitting on the bench, I couldn’t understand where I was, how I got here and what I was doing. A terrible panic seized me, I began to scream and cry.
My anomalous thinking consists of very strange logical chains. If my friend and I are walking together, and she didn’t look at me when I looked at her, strange thoughts appear. It's like this: If she didn't look at me, it means she doesn't value me. Our friendship is not so strong on her part, she does not love me. Our friendship is over.
The symptoms of schizotypal disorder are varied and similar to those of schizophrenia. But they are expressed to a lesser extent, do not lead to loss of reason, and the person understands the painfulness of his condition.
Differences between schizotypal disorder and schizophrenia in psychiatry
The diagnosis of “schizotypal disorder” excludes severe psychotic disorders characteristic of schizophrenia, among them: delusional, hallucinatory, movement disorders (catatonia), clouding of consciousness.
In addition, with schizotypal disorder there are never such severe outcomes as with schizophrenia, for example, apathetic-abulic dementia.
In addition, with schizotypal disorder there are never such severe outcomes as with schizophrenia, for example, apathetic-abulic dementia.
Symptoms and manifestations
In the International Classification of Diseases (ICD), schizotypal disorder f21 is classified in the “Schizophrenia” section. Its other name is sluggish schizophrenia. The diseases are indeed similar. Is it possible to mix them up? In both cases, the patient is characterized by:
- detailed and stereotypical thinking;
- eccentric behavior;
- unexpected psycho-emotional reactions;
- delusional state and excessive suspicion;
- tendency to isolate from society.
In schizophrenia, these symptoms are more pronounced. At the same time, there is a complete break with reality. This is not typical for f21, although the individual’s behavior does not meet generally accepted norms.
| Service | Price |
| Initial consultation by phone | for free |
| Detailed consultation by phone/Skype | from 1,000 rubles |
| Consultation with a psychiatrist in the clinic | from 1,500 rubles |
| Home visit | from 5,000 rubles |
| Urgent home visit | from 8,000 rubles |
| Constant observation by a psychiatrist | from 10,000 rubles |
Causes of schizotypal disorder
Genetic reasons. The external clinical similarity of schizotypal disorder with other mental illnesses may be explained by hereditary factors. Scientists have discovered a number of common genetic abnormalities with schizophrenia, bipolar affective disorder and personality disorders (psychopathy). For example, the genetic contribution explains the exceptionally high level of characteristics characteristic of patients: strange appearance and behavior, aloofness, and lack of close friends. The genetic commonality of schizotypal disorder and schizophrenia also causes some cognitive deviations that relate to attention and memory.
Environmental factors. The causes of schizotypal disorder are associated not only with heredity, but also with factors unfavorable for the development of the fetus, psychological trauma in early childhood, and chronic stress. In particular, maternal influenza during the sixth month of pregnancy was associated with higher levels of schizotypal symptoms in the adult male population. Serious risk factors for the development of schizotypal disorder in youth may include malnutrition of the pregnant mother and child under three years of age, a history of child abuse, emotional abuse (including bullying and post-traumatic disorder), neglect, and neglect, especially with a corresponding genetic background.
The combination of various adverse effects leads to disturbances in the neurochemical balance in the brain, hormonal and immune abnormalities, which determine the clinical picture and accompany schizotypal personality disorder.
Causes
What is the main causal source of the development of the disease is not known exactly.
Psychiatrists identify the following factors that contribute to the onset of painful manifestations:
- Genetic. Presence of relatives in the family with a similar problem.
- A depressing atmosphere in the house for a child, alcoholism, drug addiction among loved ones.
- Psychotrauma.
- Difficult pregnancy and pathological birth of the mother.
- Features of character and temperament.
When parents understand that they cannot do without the help of a psychiatrist, they are faced with an acute question: is it possible to cure their children. They come to our clinic for a consultation with this problem.
Diagnosis of schizotypal disorder
The diversity and multicomponent nature of symptoms in men and women with schizotypal disorder in psychiatry creates difficulties in diagnosis. Outwardly, patients may exhibit anxiety or "neurotic conflicts" that are determined or aggravated by "hidden" magical ideas, strange beliefs, or overvalued ideas. Therefore, schizotypal patients are often initially diagnosed with attention deficit disorder, social anxiety disorder, autism, dysthymia, neuroses, bipolar disorder, depression, and psychopathy.
Only a psychiatrist can establish a diagnosis of “schizotypal disorder” and give a prognosis after appropriate clinical examinations of the patient, obtaining objective information regarding his behavior and manifestations of the disease from close relatives.
Only a psychiatrist can establish a diagnosis of “schizotypal disorder” after appropriate clinical examinations of the patient, obtaining objective information regarding his behavior and manifestations of the disease from close relatives.
Additional methods will improve the quality and reliability of diagnosis - pathopsychological, neurophysiological examinations, blood tests to identify markers of the activity and severity of a mental disorder (for example, Neurotest).
Thanks to a pathopsychological examination (conducted by a psychologist), the characteristics of cognitive processes, the emotional-volitional sphere, and personal characteristics are revealed, which form the psychological portrait of the patient along with pathological traits caused by schizotypal disorder. Neurophysiological examination gives an idea of the degree of damage or distortion of cognitive functions, the degree of reserve and compensatory capabilities of the brain.
The neurotest includes several indicators that reflect the state of the immune system involved in the formation of schizotypal disorder and other schizophrenia spectrum disorders. Certain combinations of deviations in indicators indicate a specific variant of the disease, suggest its prognosis, the degree of severity, severity of the condition and the effectiveness of the therapy.
Causes
It is impossible to identify the exact reasons for the formation of a schizoid personality type; research is still ongoing. The following risk factors are expected:
- genetic, that is, congenital, characteristics of the individual;
- the presence of any mental spectrum disorders in close relatives - the theory of hereditary predisposition;
- environmental factors - social status, local mentality, characteristics of growing up;
- the nature of the relationship of parents or guardians to the child in the process of personality formation;
- the cumulation of experiences from early childhood to the present - stress, fear, loneliness, neglect from others, any type of violence.
It is not possible to talk about a single etiology, since the topic remains poorly studied even in a professional environment. Therefore, you should not specifically look for the most “convenient” reasons that explain the characteristics of a particular person.
Each clinical case should be reviewed by a psychiatrist, who will be able to determine the individual set of prerequisites that served as the impetus for the formation of SPD.
Treatment of schizotypal disorder
Treatment of schizotypal disorder should begin as early as possible and be comprehensive. Timely diagnosis and adequately selected therapy not only reduce painful symptoms, but also reduce the risks of developing complications in the form of loss of ability to work, social isolation, loneliness, the transition of a slow-moving disease process into more severe forms of schizophrenia, the emergence of addictions, and suicidal tendencies.
Complex therapy is an effective combination of psychotropic drugs and psychotherapeutic techniques. Remember! Only a qualified psychiatrist knows how schizotypal disorder is treated.
Drug therapy. Drugs of various pharmacological groups are used - antipsychotics, antidepressants, mood stabilizers, tranquilizers. Specific regimens are selected individually, taking into account the clinical picture, duration of the disease, and state of physical health. Treatment is long-term: after relief of current symptoms, maintenance therapy is carried out.
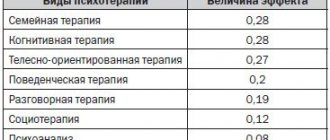
Psychotherapy. Supervision of the patient by a psychotherapist is mandatory to obtain a positive and stable result. Unlike schizophrenia, with schizotypal disorder the use of almost all known types of psychotherapeutic techniques is permitted. During sessions with a psychotherapist, the necessary skills are developed to cope with symptoms, maintain social connections, form attitudes to activate volitional and motivational impulses, and correct pathological personal characteristics. Psychotherapeutic sessions have an important psychoprophylactic value, helping to increase the stress resistance of patients and prevent self-aggressive behavior.
Unlike schizophrenia, treatment for schizotypal disorder involves the use of almost all known types of psychotherapeutic techniques.
Primary prevention of schizotypal disorder in children involves early environmental enrichment. This includes exercise, cognitive stimulation and improved nutrition between three and five years of age, which improves brain function and reduces the likelihood of developing the disease in youth.
Treatment
Completely and irrevocably eliminating all symptoms of the disorder is an impossible task. But psychotherapeutic influence is necessary. Treatment involves teaching the person with the disorder social skills. Drug therapy for SPD is a method that has not been scientifically proven, and its effectiveness is controversial.
Carriers of the disorder rarely seek psychiatric help. Most often, they find themselves in the doctor's office when psychological difficulties arise at work or in family life.
Schizoid personality disorder without psychotic symptoms does not require inpatient or medicinal treatment. However, in advanced cases aggravated by psychotic pathologies, therapy involves psychotropic drugs. Antipsychotic spectrum drugs are most often prescribed.
Pronounced symptoms of SPD can be relieved with small dosages of antipsychotic drugs (sulpiride, amisulpride, aripiprazole, etc.). When a personality disorder of the schizoid type is combined with a depressive episode, antidepressants and mood stabilizers are added to the treatment plan.
However, psychotherapy for the condition plays a key role. It resolves intrapersonal and interpersonal conflicts, unsatisfied needs (for schizoids it is often related to the sphere of self-realization). Hospitalization is relevant only if SPD is burdened by psychotrauma, suicidal intentions (often), and psychotic reactions.
The psychotherapist’s task is to gently draw the patient’s attention to the negative consequences of pronounced inappropriate behavior. Recommendations are provided on how to comply with society's norms and rules. The specialist adheres to the goal of drawing the patient’s attention to the surrounding reality. An important point is that the patient's family members are involved in the therapy process. In this case, group and family counseling is carried out.
During treatment, restorative and relaxing procedures are useful - massage sessions, physiotherapeutic methods, exercise therapy. Psychotherapeutic influence does not accomplish the task of radically changing the patient’s character - this is impossible. The goal is only to help develop adaptability to the surrounding reality and facilitate professional development.
Cognitive behavioral therapy is an excellent option for this pathology. It will alleviate the symptoms of maladjustment, recklessness, and isolation. Therapy increases self-confidence and corrects attacks of affective outbursts. Correcting the condition is a long and labor-intensive process; the disorder is not often treatable.