Psyche and immunity
The term "psychoimmunology" was coined in 1964 by George Solomon to refer to the relationship between emotions, immunity and disease. Robert Adler from the University of Rochester expanded this concept in 1975, and now doctors use the term “psychoneuroimmunology,” which more fully reveals the meaning of the mutual influence of mental state and physical health.
In recent years, this area has been developing rapidly, and even non-professionals should keep abreast of the main discoveries.
What is this immunity anyway?
Let me briefly remind you that immunity is the body’s ability to protect itself from foreign objects. The biological meaning of immunity is to preserve the genetic integrity of the body. The so-called immune system consists of a central part: the red bone marrow and thymus - and a peripheral part: the spleen and lymph nodes.
You may have noticed that when you have a boil, the nearby lymph nodes increase in size. This happens as they build up strength to protect you. It is not surprising that doctors pay so much attention to the lymph nodes, feeling them during a medical examination.
Special cells—lymphocytes—play an important role in the body’s immune response. At the cellular level, T-lymphocytes work (they mainly destroy and break down damaged cells), and the humoral response (production of antibodies in the blood) is provided by B-lymphocytes. There are many other protective cells, especially the “cool” ones are called “natural killers”; they are able to effectively attack tumor cells.
How do psychological factors affect the immune system?
Most often, this influence is exerted through the endocrine system. Increased nervous tension leads to the release of catecholamines and cortisol, which ultimately reduces the activity of the immune system.
By the way, doctors use synthetic analogues of catecholamines and cortisol to treat allergic reactions and so-called autoimmune diseases (when the immune system “goes crazy” and attacks its own cells).
And other mechanisms of influence of the human psyche on the immune system remain to be studied. For example, it is still not clear why a person who looks at wallpaper with strawberries has a severe allergic reaction, as if he had actually eaten a certain amount of these berries (we are, of course, talking about a person who has previously allergic reactions to strawberries have been reported).
Acute and chronic stress suppresses the immune system
The easiest way to study the effects of stress on the body was to study medical students, since they, like any students, experience exam stress with a certain frequency and are very responsible for medical and biological research.
Thus, the immune response was tested during three-time vaccination against hepatitis B. The production of antibodies to hepatitis B occurred only in those students who did not experience exam stress. Those who experienced even moderate levels of anxiety did not produce the necessary immune response. That is, vaccination was useless for them. And note, we are talking about completely healthy young people. And the stress was not the greatest.
The same was observed regarding the healing of superficial wounds during examinations. The process was on average 40% slower than during the summer holidays.
Not only exams, but also other seemingly ordinary things can suppress your immune system. A fairly common example of chronic stress occurs in family caregivers. God forbid you have a family member with Alzheimer's. Here your defenses will definitely be depleted, and everything that the restless students experienced during the session will manifest itself with particular force.
Can chronic stress disrupt the immune system?
17.03.2021
Chronic stress can disrupt the functioning of many body systems, including the immune system .
The immune system interacts with the nervous system , especially the brain , and the communication itself is two-way. The third “musketeer” in this dialogue is the endocrine system , that is, endocrine glands such as the pituitary gland , adrenal glands and thyroid glands, which constantly produce hormones . All these systems together ensure the maintenance of homeostasis, that is, internal balance and protection from the external environment. So it’s not difficult to guess that the state of the psyche can affect immunity . However, the question is how big its impact can be.
Psychoneuroimmunology
Recently, there has been an intensive development of work on the effect of stress on the immunity of the human body. Research is being conducted in the field of medical sciences and psychology itself. This sudden increase in interest in the above topic led to the emergence of a new scientific field - psychoneuroimmunology.
Psychoneuroimmunology is a science that studies the influence of the psyche on health. Her main interests include the relationship between stress and disease (how it influences its occurrence or exacerbation).
A breakthrough for this field of science came with the discoveries of the 1960s, when the belief that the independence of the nervous and immune systems was not true was confirmed.
The brain can influence the lymphatic organs (the places where immune system grow and mature) through the autonomic nervous system or through the well-known HPA (hypothalamus-pituitary-adrenal) axis. In turn, this axis is one of the main “regulators” of the body’s stress response. Why is it important?
It has been known for some time that substances released by cells of the nervous system lead to changes in the body's immune response. Some cells of the immune system , namely macrophages and lymphocytes, have receptors on their surface with which they can receive signals transmitted by the central nervous system , thanks to a wide range of different neurotransmitters, which, in turn, cause certain changes in the functioning of the immune system . It is also interesting that lymphoid cells themselves have the ability to produce many neuroactive substances, and they can reverse the secretion of neurotransmitters in nerve endings located in the immune system .
Indirect effects of chronic stress
immune system dysfunction due to chronic stress, there are also indirect mechanisms that can negatively affect the said system. Namely, a frequently observed phenomenon with concomitant long-term stress is the use of various types of stimulants, more or less common. It is not uncommon for people exposed to chronic stress to have trouble sleeping, which can also lead to a weakened immune system .
Bottom line
Today we can say that stress, especially chronic stress, negatively affects the functioning of the immune system . Interestingly, short-term stress can even support certain immune functions, which is clearly not the case with chronic stress. It is also known that under conditions of chronic stress, susceptibility to viral infections increases and vaccine-stimulated antibody production decreases.
Published in Immunology Premium Clinic
Stress hormones reduce immunity: how to deal with fatigue and irritability
We live in an age of speed and stress. According to a recent international study, Russia has taken first place in the list of countries where residents experience stress at work. 81% of Russians admitted this. In Germany there are 51%, in the USA - 39%, and in sunny Italy - only 23%.
“Emotions and mood have a direct impact on the immune system,” Professor Kholodova notes in the meantime. — Short-term stress increases the body's resistance to respiratory infections. But a prolonged one leads to the opposite consequences. The body sacrifices little to protect itself as a whole - it grabs viruses.
Recent studies have shown that neurotic people get ARVI 2-3 times more often than emotionally stable people and stay sick longer. And today scientists can explain this scientifically. After all, stress affects all organs and systems, stimulating the central nervous system to produce excessive amounts of the hormones cortisol and norepinephrine. With a little stress, cortisol creates protection, but if there is too much of it, it begins to destroy organs, triggering autoimmune processes, which ultimately weakens immunity. “Recently, our colleagues from Samara, under the leadership of Professor Sitnikov, conducted a study among children with ARVI. It turned out that the more severe their infection was, the higher their levels of norepinephrine and cortisol were,” continues Irina Kholodova.
These studies only confirmed the results of several scientific studies conducted abroad. Thus, German researchers have found that during the exam period, students are more likely to get viral infections due to the fact that their titer of antibodies that protect against infections drops sharply. Russian scientists conducted studies with medical students whose immune activity in the blood worsened during the session.
What are the symptoms of long-term stress? They can be very non-specific. For example, with prolonged stress, pain often appears (heads, backs, legs, etc.), nausea, tachycardia, memory problems, difficulty concentrating, anxiety and restlessness, mood swings, short temper, irritability, malnutrition or overeating (especially sweets). ) insomnia.
How to deal with stress? A VTsIOM survey showed that 46% watch TV for this purpose, 46% listen to music, 19% wash down stress with alcohol, 16% eat. Only 12% resort to sports (and rightly so, 9% to sex, and 2% to meditation and yoga. “Of course, sports are wonderful. But stress often needs to be treated. In our country, such patients are most often prescribed anxiolytics and beta blockers "Many of them cause adverse reactions and addiction. I personally prefer homeopathic drugs, which work perfectly in this regard. By the way, my colleague Academician Konovalov is now conducting research in Kazan on the treatment of stress with ultra-low doses of drugs," says Irina Kholodova.
Well, you also need to sleep at least 8 hours, spend more time in the fresh air, eat less heavy food (fatty, fried, peppered and smoked) and more vegetables and fruits, and also consume sufficient quantities of vitamin C. Then save your psyche, and you will get ARVI less often.
Oxidative stress can cause the development of cancer
Oxidative stress may not have clear symptoms and develop in various organs of the human body. It leads to the development of serious pathologies, including cardiovascular diseases and cancer - specialists from the PMI Science project spoke about this at a scientific and practical seminar in Moscow.
Oxidative stress, which is the process of cell damage as a result of oxidation by free radicals, leads to a malfunction of the cells and tissues of the body. Pathological reactions are triggered, irreversibly damaging the cell and leading to the launch of genetically programmed death - apoptosis.
“The main provoking factors in the development of oxidative stress are physical overexertion, chronic diseases, smoking, exposure to solar radiation and toxic substances, alcohol in excessive quantities, uncontrolled use of medications,” says
PMI Science scientific advisor Dmitry Belopakhov .
“More and more research suggests that understanding the mechanisms and causes of oxidative stress will help more effectively prevent diseases of various etiologies and develop preventive medicine .”
If a patient constantly feels tired, has decreased immunity, has worsened skin condition, or has severe headaches, these could all be symptoms of oxidative stress. In this case, early diagnosis and correction of risk factors is important, which will help avoid the development of acute and chronic diseases.
“Chronic systemic inflammation of low activity is a long-term activation of pro-inflammatory immune pathways associated with the risk of developing chronic non-infectious diseases, such as chronic obstructive pulmonary disease and some forms of cancer,” emphasized Dmitry Belopakhov. “In addition, oxidative stress is one of the significant mechanisms of damage to nervous tissue, the fight against which is a pressing problem in neurology.”
According to oncourologist of Sechenov University Vladimir Lekarev
And, in Russia, in the structure of mortality, oncological diseases occupy second place after diseases of the circulatory system. And one of the most provoking factors for the development of cancer is smoking.
“Tobacco smoke contains carcinogens that affect the formation of DNA adducts, as a result of which DNA damage occurs, somatic mutations accumulate and cancer develops,” said Vladimir Lekarev. — It has been proven that smokers have a 4 times higher risk of developing bladder cancer than non-smokers. Smoking also increases the risk of developing urothelial cancer, prostate cancer, and kidney cancer. In addition, the risk of postoperative and infectious-inflammatory complications is higher among carriers of this habit.”
Moreover, according to doctors, smoking is one of the most modifiable factors that enhance oxidative and inflammatory reactions. Applying harm reduction concepts and switching patients to electronic heated tobacco systems may reduce oxidative stress in patients who do not quit smoking.
A clinical case reported by cardiovascular surgeon Rasul Gadzhimuradov
, shows significant improvement in the condition of a 62-year-old patient with multifocal atherosclerosis after quitting smoking conventional cigarettes.
“The patient, in addition to atherosclerosis, has diabetes, atrial fibrillation, and suffered a heart attack. He smokes from about 14 years old, 2-3 packs a day. Several years ago, due to a blocked artery, he developed gangrene in his foot. Part of the foot had to be amputated,” said Rasul Gadzhimuradov. — The patient continued to smoke, a heart attack and arterial obstruction occurred again. The issue had to be resolved firmly; the patient himself sought advice on alternative means of obtaining nicotine, since he was unable to give up the bad habit. We advised him to switch to ESNT. There are currently no relapses of the disease."
Link to publication: medvestnik.ru
What diseases most often develop due to stress?
What diseases most often develop due to stress?
Stress is any experience that causes tension: physical, psychological or emotional. Short-term stress does not pose a threat to health, but chronic stress has a strong impact on the immune system and can ultimately lead to illness.
Short-term stress is not dangerous
A meeting with a lion that escaped from the zoo can be considered a stressful situation. At this moment, your body suspends many of the processes occurring in it (the hormone cortisol is responsible for this) and throws all its energy into flight (adrenaline helps with this). It’s even good for the body (well, unless the lion catches up with you). Once you are safe, adrenaline and cortisol levels will return to normal and all systems will resume their normal functioning.
But if you are constantly under pressure from some situation: financial problems, difficulties in relationships, at work, illnesses of loved ones, then it may seem that you are being attacked by mini-lions every day. The body perceives all these troubles as a threat. And the stress response remains turned on in the background.
Non-stop stress triggers inflammation
In 2012, scientists found that non-stop stress is associated with the fact that the body regulates the inflammatory response worse. Inflammation is partly controlled by the hormone cortisol, and prolonged stress alters its effectiveness by reducing tissue sensitivity to the hormone. The body is not able to adequately respond to infectious diseases - recovery is delayed, and more complications arise. The inflammatory background aggravates the underlying disease: diabetes, angina or any other.
A 2021 study found that stress exposure significantly increases the risk of developing autoimmune diseases such as rheumatoid arthritis, psoriasis, multiple sclerosis, and lupus. People with stress disorder were more likely to be diagnosed with autoimmune diseases, including multiple ones. Scientists also noted that people with post-traumatic stress disorder who took antidepressants were less likely to experience autoimmune diseases, unlike those who did not take medications.
How to control stress
Stressful events in life cannot be avoided, but you can learn to control their impact on your life. Helps cope with stress:
- eating a healthy diet, regular exercise and getting enough sleep;
- different relaxation methods: yoga, deep breathing practice, massage or meditation;
- favorite hobbies (surfing the Internet does not count);
- communication with friends and like-minded people;
- professional consultation with a psychologist or psychotherapist.
The conference rooms of scientific institutes are now full of a new breed of scientists: psychoneuroimmunologists. These people make their living doing research based on the incredible fact that what goes on in our heads can affect how our immune system works. It was once believed that these two areas were in no way connected with each other - the immune system destroys bacteria, produces antibodies, hunts tumors; the brain helps us dance, reinvent the wheel and watch our favorite television series. But the idea of independence of the immune and nervous systems turned out to be erroneous. The autonomic nervous system threads nerves into body tissues that form or store immune system cells. These cells then enter the blood. In addition, the tissues of the immune system turn out to be sensitive (that is, they have receptors) to all those interesting hormones that are produced by the pituitary gland at the command of the brain. Therefore, as it turns out, the brain constantly sticks its nose into the affairs of the immune system.
Evidence of the brain's influence on the immune system began to emerge at least 100 years ago, with the first demonstration that if a person with a rose allergy were to wave a fake rose in front of their nose (assuming they did not know the rose was fake), they would have an allergic reaction. . Here's a fascinating and more recent demonstration that the brain influences the immune system: consider two groups of professional actors. Let's ask the first group to rehearse a dark, depressive scene all day, and the second group to rehearse an optimistic, joyful sketch. For actors in the first group, the immune system response will weaken, while for actors in the second group it will increase. (Where do you think this study was conducted? UCLA, of course.) But the most clear-cut link between the brain and the immune system came from a study based on a paradigm called “conditional immune suppression.” Give the animal a drug that suppresses the immune system. Then conduct Pavlovian-style experiments with “conditioned stimuli,” such as giving the animal a flavored drink that it can associate with an immune-suppressing drug. A few days later, give the animal only a conditioned stimulus that causes a response, and immunity will decline. In 1982, a report was published of an experiment based on a variation of this paradigm, conducted by two pioneers in the field, Robert Ader and Nicholas Cohen of the University of Rochester. The results stunned scientists. In experiments on mice, animals suddenly began to get sick due to excessive activity of the immune system. The disease is usually controlled by giving the mice immunosuppressants. Ader and Cohen showed that using conditioning techniques, a drug can be replaced with a conditioned stimulus - and this affects the immunity of animals to such an extent that it can prolong their life.
Studies like these have convinced scientists that there is a strong connection between the nervous and immune systems. It stands to reason that if artificial rose or the taste of a flavored drink can change immune function, then stress can too. In the first part of this chapter, we will discuss the effects of stress on immunity and how it can be useful in stressful situations. In the second part of this chapter, we'll look at whether long-term stress due to chronic immune suppression can weaken the body's ability to fight infectious diseases. This is a very interesting question, and can only be answered with great caution and many caveats. There is emerging evidence that stress-induced immune suppression may actually increase the risk and severity of certain diseases. But this connection does not seem to be very pronounced and its importance is often exaggerated.
To appreciate modern advances in this complex but important area of knowledge, you need to start with the basics - with how the immune system works in general.
How the immune system works
The main job of the immune system is to protect the body from infectious agents, such as viruses, bacteria, fungi and parasites. This process is incredibly complex. On the one hand, the immune system must distinguish between normal cells and aggressor cells - in the jargon of immunologists, distinguish “ours” from “strangers”. Somehow, the immune system remembers what every cell in our body looks like and attacks any cells that do not have our individual “cellular signature” (such as bacteria). Additionally, when faced with a new invader, the immune system can even create an immunological “record” of what the infectious agent is like. This allows her to prepare for his future incursions. The principle of vaccination is based on this ability: we are injected with a small amount of a weakened infectious agent, and this prepares the immune system for a real attack.
Immune defense is activated by a complex complex of cells circulating in the blood. They are called lymphocytes and monocytes (collectively, immune cells are called leukocytes; “cytes” are “cells”). There are two classes of lymphocytes: T cells and B cells. Both are formed in the bone marrow, but T cells migrate to the thymus (thymus gland) and reach maturity there (which is why they are called “T cells”). B cells mature in the bone marrow. B cells produce primarily antibodies. There are several types of T cells (T helper cells, T suppressor cells, cytotoxic killer T cells, etc.).
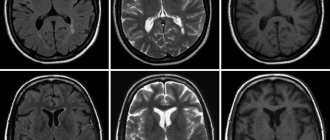
T cells and B cells attack infectious agents in different ways. T cells create cellular immunity (Fig. 25). When an infectious agent invades the body, it is recognized by a monocyte called a macrophage. It reports the foreign particle to the T-helper cell. The alarm siren turns on, and in response to the invasion of the “stranger,” T-cells begin to disperse throughout the body. This signaling system leads to the activation and rapid expansion of cytotoxic killer T cells. True to their name, they attack and destroy infectious agents. By the way, the AIDS virus kills the T cells of the immune system.
B cells act differently. They support immunity by creating antibodies (Figure 26). Once macrophages and T helper cells have begun to act, they stimulate the proliferation of B cells. The main task of B cells is to differentiate and produce antibodies - large proteins that recognize certain features of the invading infectious agent (usually its specific protein) and attach to it. Such selectivity is very important - the shape of the resulting antibody exactly “fits” the shape of one or another distinctive feature of the invader, like a key to a lock. Thus, antibodies attach to the cells of the infectious agent, block them and prepare them for destruction.
Rice. 25. Cascade of cellular immunity. (1) The infectious agent is attacked by a special type of monocyte called a macrophage. (2) The macrophage reports the infectious agent to the T helper cell (a type of white blood cell) and produces interleukin-1 (IL-1), which stimulates T helper cell activity. (3) The T helper cell then produces interleukin-2 (IL-2), which triggers the proliferation of T cells. (4) This leads to the proliferation of another type of leukocytes, cytotoxic killer T cells, and they destroy the infectious agent
Rice. 26. Immune cascade based on antibodies. (1) The infectious agent encounters a macrophage. (2) The macrophage reports the infectious agent to T helper cells, and they produce interleukin-1 (IL-1), which stimulates the activity of T helper cells. (3)T helper cells produce B cell growth factor, and this triggers the differentiation and rapid proliferation of another type of leukocyte, B cells. (4) B cells produce specific antibodies that attach to proteins of the infectious agent, preparing it for destruction by a large group of proteins circulating in the blood called complement
The immune system has another interesting aspect. For example, if different parts of the liver must coordinate a particular activity, they have a proximity advantage. But immune system cells circulate freely in the blood. To ensure that the alarming immune siren was heard in all parts of this vast system, the body created chemical messengers. )They also circulate in the blood and carry messages between different types of immune cells. For example, when macrophages first recognize an infectious agent, they produce a messenger called. It induces helper T cells to produce interleukin-2, which stimulates the growth of T cells (to further complicate this scheme, there are at least five additional interleukins with more specific functions). On the antibody front, T cells also produce B cell growth factor. Other classes of messengers, such as interferons, activate different types of lymphocytes.
The sorting process, in which the immune system distinguishes between self and non-self, is usually quite effective (although some sneaky tropical parasites, such as schistosomiasis, have learned to trick the immune system by appropriating the “signature” of the body’s own cells). The immune system is constantly busy separating “us” from “strangers”: red blood cells are mine. The eyebrows are mine. The virus is disgusting, let's attack. Muscle cells are our guys... (Fig. 27).
Rice. 27. Microphotograph of a nonspecific killer T cell attacking a tumor cell
But what if the immune sorting process goes wrong? One obvious type of error is when the immune system fails to recognize the infectious invader; of course this is very bad. It is equally dangerous if the immune system mistakenly recognizes as a harmful invader something that in fact is not one. For example, some completely harmless substance triggers an alarm reaction. It could be something edible, like peanuts or shellfish, or something airborne and harmless, like pollen. But the immune system mistakenly decided that it was not only “foreign”, but also dangerous, and began to actively fight it. In this case, an allergy occurs.
In the second type of immune system overreaction, a normal part of our own body is mistaken for the infectious agent and, as a result, it is attacked. When the immune system mistakenly attacks a normal part of the body, it can lead to a wide variety of very nasty “autoimmune” diseases. For example, in multiple sclerosis, the nervous system is attacked; in juvenile diabetes, pancreatic cells that normally produce insulin. As we will soon see, stress, surprisingly, influences the course of autoimmune diseases.
So far in this brief overview of the immune system, we have talked about acquired immunity. Suppose you are exposed for the first time to some new, dangerous pathogen, let's call it pathogen X. Acquired immunity has three features. Firstly, it allows you to “learn” to attack pathogen X with the help of specific antibodies and immune cells that can recognize this particular pathogen. This has an important advantage: we have a “marker” on which the name of pathogen X is written. Secondly, it takes time to create such immunity: when we first encounter pathogen X, we need to find out which antibodies best match it and create millions of copies of it. We can then identify and destroy pathogen X for many years, and if that specific defense is already there, repeated exposure to pathogen X will only strengthen that defense.
This acquired immunity is a very unusual invention, and it is found only in vertebrates. But we also have a simpler, more ancient mechanism of the immune system, the same as that of living beings of a completely different species - insects. It's called innate immunity. It doesn't provide defenses designed specifically for pathogen X and specific antibodies that are different from those designed for, say, pathogen Y. But when a pathogen hits us a second time, this nonspecific immune response also comes into play.
This generalized immune response most often occurs at the front line where the pathogen first establishes a foothold, such as in the skin or mucosal tissue in the mouth or nose. As soon as this happens, the antibodies contained in the saliva attack any “foreign” microbes. This is a nonspecific reaction that does not distinguish invaders from each other. Such antibodies are produced in the mucous membrane and cover it with an antiseptic layer. In addition, at the site of infection, capillaries dilate and immune cells can freely enter here from the blood, infiltrating the area of infection. Among these cells are macrophages, neutrophils and nonspecific killer cells that attack harmful microbes. The expansion of capillaries also increases the flow of fluid containing proteins that prevent aggressive microbes from entering the blood. What happens as a result? Proteins fight germs, and fluid causes swelling. This is how the innate immune system works: it causes inflammation¹. So now we have a basic understanding of how the immune system functions. It's time to look at how stress affects your immune system. Naturally, this process is much more complicated than it might seem.
________________________________________________
¹ As we just said, the innate immune response relies on proteins entering the infected area. Among the proteins that fight microbes is one we talked about in Chapter 3, C-reactive protein in the blood. I'm sure you remember that sticky particles, such as cholesterol, create atherosclerotic plaques only in places where blood vessels are damaged. Therefore, the degree of damage and the severity of inflammation of blood vessels is a good predictor of the risk of atherosclerosis. C-reactive protein, as we already know, is the most reliable indicator of such inflammation.
Previous – Women: cycle disorders and amenorrhea | Next – How does stress suppress the immune system?
How stress affects immunity
08.08.2018
Interesting
Natalia Adnoral
“Calm, just calm. Nonsense, a matter of everyday life"
This well-known Carlson “mantra” can become a reliable means of maintaining and promoting health.
It’s no longer a secret that stress directly affects the functioning of the nervous, endocrine and immune systems, and, therefore, the body as a whole. And if an “acute” stressful situation mobilizes internal reserves and helps to “jump out” of a difficult physical or psychological situation, then chronic stress, on the contrary, gradually leads to exhaustion of the body. Many mechanisms of these relationships have already been discovered by modern science: stress - activation of the immune system - increased inflammatory response - atherosclerosis, obesity, diabetes, heart attack, stroke, other severe acute and chronic diseases, including oncology.
For example, scientists from Rice University “calculated” a chain of reactions linking chronic stress and diabetes: a depressed mental state increases the formation of interleukin 6, one of the proteins of the immune system that mediates the inflammatory response. High protein levels lead to disruption of carbohydrate metabolism, which leads to increased blood sugar levels. And from here diabetes is just a stone's throw away. Moreover, other researchers (the results were published in the journal Cell Metabolism) identified another mechanism - a decrease in tissue sensitivity to insulin (one of the causes of type 2 diabetes) under the influence of an inflammatory response.
It would seem that the immune system activated by stress should better cope with its direct responsibility - protecting the body from external and internal aggressors. However, the facts indicate the opposite: the body of people under prolonged stress becomes very susceptible to various pathogens and gets sick faster. Why?
Scientists from Carnegie Mellon University in Pittsburgh found that the culprit is not the inflammatory response as such, but its inadequacy to the situation - that is, the loss of the ability of the immune system to regulate the severity of inflammatory processes.
There has already been enough similar work in the world to recognize chronic stress as an “accomplice” in the destruction of our health.
But there is also good news from science - a feeling of happiness, joy, trust, acceptance strengthens the immune system, accelerates recovery, and rejuvenates the body! Moreover, according to scientists (for example, Professor Andrew Steptoe), it is a person’s internal sense of self that is important for health, and not the quality of external events. And it is precisely this subjective assessment, unlike life circumstances, that we are free to choose! No matter what happens to us, our reaction to what happened depends on us and only on us.
It is not this event that is a misfortune, but the ability to endure it with dignity is happiness. Marcus Aurelius
Life knocks us down, but it's up to us to decide if we can get back up. Mr. Khan from the movie "The Karate Kid"
People have known about this “recipe for health” (and not only physical health) for a long time, and many have proven its effectiveness with their own lives.
Make an appointment
ABOUT THE WOUNDS OF WINNERS: HOW DOES STRESS AFFECT IMMUNITY?
Unfortunately, this law also works in the opposite direction. A person broken by life's troubles will get sick faster - and this even applies to “colds” and flu.
As the “Tension and Stress” survey conducted recently by the Levada Center showed, we are twice and sometimes three times more likely to get upper respiratory tract infections when our souls are anxious or bitter. And we recover significantly longer than the “national average.”
What is the connection between mental health and physical health? This question is answered by Professor Irina Nikolaevna Kholodova , Doctor of Medical Sciences, teacher of the Department of Pediatrics of the Russian Medical Academy of Postgraduate Education.
WHAT IS YOUR MOOD AND IS YOUR IMMUNITY?
“The results of recent research in the field of neurophysiology suggest that emotions and mood affect the immune system of the human body, reducing or increasing its resistance to acute respiratory infections,” explains Irina Nikolaevna. “At the everyday level, many note, for example, that when a person is self-confident and passionate about some goal, he is not distracted by negative factors that always surround everyone, and in this state he is less susceptible to infectious diseases.”
The wounds of winners heal faster. Modern neurophysiologists scientifically prove the ancient wisdom.
WHEN WE ARE WORRIED, WE MOBILIZE
Stress, to some extent, is a natural part of our lives. As the author of the anti-stress method of synchrogymnastics “Key”, used in the Ministry of Emergency Situations, the Ministry of Internal Affairs and among cosmonauts, Dr. Khasai Aliev , notes, stress arises when we are faced with the unknown, uncertainty. And there are very, very many such situations.
If the stress is small, it improves performance, helps to get ready... The body concentrates its energy on solving an important task. We are worried, but at the same time we are mobilizing.
with the famous Soviet goalkeeper Vladislav Tretyak before the match with Czechoslovakia. The specialist helped me completely overcome my anxiety.
“During the skate, I felt an extraordinary surge of strength: I didn’t miss a single puck. Well, I think this is a psychologist! - Vladislav Tretyak recalled. – But, apparently, at some point this self-confidence grew into self-confidence. I missed one goal and immediately fell apart. And it all ended - 3:8. After this incident, that psychologist did not appear on the team..."
Fans all over the country were in shock. The legendary goalkeeper missed eight goals! Tretiak has never played so badly.
BEYOND THE POSSIBLE
Under short-term stress, a person sometimes becomes stronger than one could imagine.
A fragile woman lifts a heavy truck (her little daughter ran out onto the roadway and could have been crushed under the wheels in a second). Patients with Parkinson's disease are the first to leave a burning hospital (two to three hours before the fire, they not only did not run, but had difficulty walking).
Stress can help you pass a difficult exam, pass an interview, win a competition, but...
WHERE DOES EMOTIONAL OVERLOAD LEAD?
When stress is severe or persistent, the biological interactions of organs in our body are disrupted. The “stress hormones” - cortisol and adrenaline - have been known for a long time. And modern diagnostic methods have helped to discover: if a person has depression, the hemispheres of the brain work and even look different. Why do they look different? When you experience negative emotions for a long time, the structure of your brain changes.
With chronic stress, when the balance of our body is already thrown off by worries and worries, biochemical processes are also disrupted. At the same time, the immune system suffers: the level of glucocorticoids in the blood rises sharply. High concentrations of these hormones suppress the immune system.
How to understand that the influence of stress on the body has crossed a dangerous line?
The following symptoms indicate that stress is beginning to destroy our health:
- constant fatigue, frequent colds, headaches, nausea, rapid heartbeat;
- problems with memory and attention, inability to concentrate, anxiety, constant tension, excitement, negative perception of reality. A person loses trust - in the world, in life, in people... Sometimes he does not trust even those who really treat him well;
- mood swings, irritability, short temper, agitation, depression, feelings of loneliness and uselessness. Literally every little thing unsettles you, and there are a lot of them at every step, even in public transport;
- undereating or overeating, self-isolation, lack of sleep, sedentary lifestyle.
All these symptoms are interconnected and often aggravate each other. When we move little, the body produces less “happiness hormones”, endorphins. And if you are plunged into depression, then your favorite activities, incl. sports and walks. Self-isolation and reluctance to communicate increase the feeling of loneliness. And vice versa.
LONG-TERM STRESS = EXHAUSTION
Anger, anxiety, depression are those feelings and states that destroy us not only in a figurative sense. Due to negative emotions, the body “wears out” faster. Even if they are not visible, and outwardly the person behaves well.
When we are in a bad mood for a long time, the functioning of the immune system is disrupted. Pathogenic microbes are present in the body even when we are healthy. But if we are healthy and look at the world with optimism, then both the number of viruses and bacteria and their activity are under strict control. But as soon as the immune system is weakened by chronic stress, pathogenic microorganisms begin to multiply intensively...
“Sometimes the “inner picture” occupies a very large, sometimes dominant place. And then it is much easier to eliminate a real microbe in the patient’s body than to “evict” an imaginary microbe from his psyche, explains Irina Nikolaevna. “Doctors know that a person who has been in this state for a long time, as a rule, does not feel exhaustion of the nervous system and cannot prevent it.”
*** Constant stress has become the norm for many of us (we can hardly influence the increase in housing and communal services tariffs, crowding in transport or bureaucracy and healthcare reform). We really don’t often feel nervous exhaustion. But sometimes the stress can be reduced by rest. It will not take away valuable time: when we are tired and work hard, the efficiency of our work is still close to zero.
Get a little better sleep, walk through a beautiful park and enjoy the golden autumn, listen to good music, watch your favorite movie and just lie on the couch when you’re tired... All this strengthens your nerves. After all, if everyday problems “unsettle” you, it means that the body is already working “to the limit.” Overwork and a healthy nervous system are mutually exclusive concepts.
Based on materials from the Ocillobus club meeting “Family health: everyone’s well-being is important”
Stress destroys the immune system, the diseases it causes and treatments
Conventionally, all people are divided into optimists and pessimists. Optimists perceive events not as stressful situations, but as set tasks (challenges) that need to be solved (overcome) in life, so they mobilize themselves (the strength of their body) in order to cope with the situation. Pessimists tend to exaggerate the importance of an event; it seems to them that they do not have enough strength and capabilities to solve the problem; Against this background, depression often develops.
There is a science - psychoneuroimmunology , which studies the relationship between the immune system and the nervous system.
It has been established that short-term and short-term stress is even beneficial to the body: small troubles, minor mistakes, emotional stress during physical activity (for example, playing a favorite sport) are a stimulating factor for the functioning of the nervous system. Adaptive mechanisms work better if they are systematically trained.
Chronic stress leads to the development of serious diseases, weakening of the body's protective immune forces, as a result of which the disease can become incurable. A proven fact is the close relationship between key systems - immune, nervous and endocrine. It is prolonged stress that causes imbalance in the optimal functioning of the body.
With prolonged stress, a complex chain of biochemical reactions occurs, which lead to changes in the quantitative and qualitative composition of the body's natural defense mechanisms. The consequence of this process is the presence of deformation phenomena in the endocrine, nervous and immune systems, and hormonal changes occur. A decrease in immunity leads to the fact that the body becomes prey for viruses and parasites, and a person begins to get sick more often.
Stress is the basis of heart disease (coronary heart disease, heart attack, stroke) and the entire cardiovascular system, hypertension, hypotension, angina pectoris, tachycardia, gastric and duodenal ulcers, eczema, impotence, bronchial asthma, atherosclerosis, diabetes mellitus type; American scientists are confident that stress plays a negative role in the development of Alzheimer’s disease,
The development of these diseases is often accompanied by insomnia, chronic fatigue, drowsiness, irritability, headaches, dizziness, memory loss and decreased concentration, neuroses, and depressive states; sometimes weight loss. A person’s nervous system is depleted, the aging process accelerates, and the quality of hair, skin, and nails deteriorates.
Stress plays a special role in the development of cancer. The vast majority of patients said that before the illness some dramatic event took place in their lives - dismissal from work, loss of housing, divorce, death in the family, strong feelings about someone close to them, about their children. And they failed to cope with the problems.
Rethinking stress is the main way to deal with it. It is necessary to find the main reasons that provoke it, and then you should learn to control it; choose your priorities. The Dalai Lama, at a meeting with leading Russian scientists at his residence in the North Indian city of Dharamsala, named a cure for depression. According to him, the root of depression in the modern world is that people build their lives around material values, and this can be changed by teaching “hygiene of emotions”: “But if I tell you about the hygiene of emotions, then even when anger approaches, you can think: “It’s approaching.” anger is a harmful emotion.” And you will try to make efforts to weaken it.”
The point is that standard methods of treating oncology (surgery, chemotherapy, radiation therapy) also have a stressor effect on the body. The results of experimental and clinical work confirm that the process of tumor metastasis intensifies after stressors: surgery, chemotherapy, radiation therapy, hypothermia, overexertion, overheating; introduction of hormones that trigger stress reactions. Stressful influences can awaken dormant cancer cells in the body.
The most promising method of treatment in a situation with oncology is a gentle effect on the body, using the truly inexhaustible possibilities of photodynamic therapy using the unique natural drug “Radachlorin” in combination with omelotherapy . This proprietary method, used at Edis Med Co LLC, allows you to effectively help the body restore its protective functions and cope not only with oncology, but also with many chronic diseases.