Symptoms
Symptoms of encephalitis include:
- headache;
- vomit;
- nausea;
- aches and pain in the joints;
- high body temperature (above 38 degrees Celsius);
- confusion;
- drowsiness;
- disorientation;
- convulsions;
- changes in personality behavior.
Not in all cases, but still, photophobia, loss of vision, neck stiffness, involuntary movements of the head, limbs, body, and insemination of body parts may also be noted. Sometimes you can experience anxiety, delusions, paranoia, and hallucinations.
Initially, the patient may seem like just a person who has the flu. But a change in his mental background already indicates that it is worth sounding the alarm and urgently calling an ambulance.
Are you experiencing symptoms of encephalitis?
Only a doctor can accurately diagnose the disease. Don't delay your consultation - call
How to get rid of viral encephalitis
After all clinical testing is completed, the treating doctor draws up a special treatment plan, which includes complex therapy. It consists of numerous techniques. Let's look at them in more detail:
- Etiotropic step - the use of drugs with antiviral effects is prescribed, as well as interferon and its like, special forms of immunoglobulin. The main task of such therapy is to correct vital options, the use of anti-edema drugs, antihypoxic and neuroprotective medications.
- Symptomatic step - aimed at taking anticonvulsants, antiemetic components, antipsychotics, tranquilizers and other psychotropic substances.
- The restorative step is carried out by a neuroprotective and vascular treatment method, various massages and exercise therapy are used, as well as physiotherapeutic techniques.
In case of mental problems, several sessions with a psychiatrist will be required. Thanks to the consultation, the patient will participate in correctional therapy, learn social adaptation and go through all stages of psychotherapy.
Causes of encephalitis
Infectious encephalitis can occur due to:
- herpes virus;
- chickenpox virus;
- for no reason.
Post-infectious encephalitis occurs due to:
- measles;
- pigs;
- flu;
- chicken pox;
- rubella;
- cytomegalovirus;
- HIV;
- Epstein-Barr virus.
This happens because the immune system begins to produce antibodies that are supposed to fight the infection. But instead, the antibodies attack the brain, where inflammation forms. Why this reaction occurs is still not clear to scientists.
Autoimmune encephalitis develops when a person’s immune system mistakenly perceives brain substances as a threat. Why this happens is also unknown, but in some cases the starting point is a tumor.
Tick-borne encephalitis virus, IgM
Antibodies of the IgM class to the tick-borne encephalitis virus are specific antiviral immunoglobulin proteins produced by the immune system in response to infection with the tick-borne encephalitis virus and indicating a current infection.
The result of the study is qualitative.
Synonyms Russian
Antibodies of the IgM class to the tick-borne encephalitis virus, class M immunoglobulins to the tick-borne encephalitis virus.
English synonyms
Anti-arboviral Encephalitis IgM, Encephalitis Virus Antibodies, IgM, Tick-borne encephalitis virus IgM (TBE virus IgM).
Research method
Enzyme-linked immunosorbent assay (ELISA).
What biomaterial can be used for research?
Venous blood.
How to properly prepare for research?
Do not smoke for 30 minutes before donating blood.
General information about the study
Tick-borne encephalitis is a seasonal (spring-summer) viral disease, transmitted mainly by tick bites; primarily affects the central nervous system.
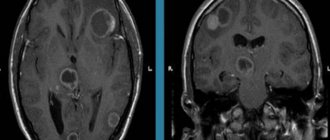
The causative agent of tick-borne encephalitis belongs to arboviruses, the flavivirus family, and is divided into three subspecies: Far Eastern, Central European and Siberian. The main carrier of encephalitis is ixodid ticks. In addition, it is transmitted through birds, rodents and predators. The incubation period averages 3-7 days. The clinical manifestations of the disease are varied. There are febrile, meningeal, meningoencephalitic, poliomyelitis and polyradiculoneuritic forms of the disease. Long-term virus carriage in the form of latent, persistent or chronic infection is possible.
In response to infection with the tick-borne encephalitis virus or vaccination against this virus, the immune system produces specific antiviral antibodies - immunoglobulin proteins. Already at the first symptoms of the disease, class M immunoglobulins appear in the blood. Their level reaches a maximum 3.5-4.5 weeks from the moment of infection and then gradually decreases over several months.
What is the research used for?
- To confirm the diagnosis of tick-borne encephalitis (both current and recent illness).
- As part of the differential diagnosis for damage to the central nervous system (infectious meningitis and encephalitis of other origins, epilepsy, aseptic meningitis, thrombosis of the arteries or veins of the brain, stroke, intracranial hemorrhage, febrile convulsions, HIV infection, cysticercosis, sarcoidosis, syphilis, meningeal carcinomatosis , paraneoplastic encephalomyelitis, etc.).
When is the study scheduled?
If you suspect current or past tick-borne encephalitis.
What do the results mean?
Reference values
Result: negative.
CP (positivity coefficient): 0 - 0.99.
Reasons for a positive result
- Early stages of tick-borne encephalitis (in this case, IgG to the tick-borne encephalitis virus is not detected). In this case, it is recommended to repeat the study after 7-10 days.
- Current or recent tick-borne encephalitis (in combination with a positive test for IgG to the tick-borne encephalitis virus), provided that no vaccination against tick-borne encephalitis has been carried out.
- Recent vaccination against tick-borne encephalitis.
Reasons for a negative result
- Absence of recent infection and, accordingly, an immune response to the tick-borne encephalitis virus (if IgG is also not detected).
- The presence of active immunity due to a recent infection or successful vaccination (if the test for IgG to the tick-borne encephalitis virus is positive).
- Weak immune response (or lack thereof) to tick-borne encephalitis due to immune system disorders (if IgG to the tick-borne encephalitis virus is not detected).
What can influence the result?
The presence of cross-reacting antibodies to other pathogens of the flavivirus genus (West Nile virus, Japanese encephalitis virus, etc.).
Important Notes
- Prevention of tick-borne encephalitis is carried out in two ways. Firstly, this is vaccination, which is carried out if there is a risk of infection with tick-borne encephalitis, and secondly, revaccination for epidemic reasons before the tick-borne encephalitis season.
- Those who were treated with gamma globulin in the first days of the disease need an additional serological study after 2-3 months due to the fact that such therapy temporarily inhibits the formation of immunity.
Also recommended
- Tick-borne encephalitis virus, IgG
- Tick-borne encephalitis virus, antigen (in cerebrospinal fluid)
- Complete blood count (without leukocyte formula and ESR)
- Leukocyte formula
- Erythrocyte sedimentation rate (ESR)
- Total protein in liquor
- Glucose in cerebrospinal fluid
Who orders the study?
Infectious disease specialist, neurologist, therapist, general practitioner.
Treatment of encephalitis
During the treatment of encephalitis it is important:
- stop the infection process with antiviral drugs;
- monitor for any immediate complications, including fever, dehydration, epilepsy;
- prevent the development of long-term complications.
Most patients are hospitalized and placed in intensive care units. Oxygen masks are worn to help with breathing. The body is fed through feeding tubes.
For the infectious type of encephalitis, antiviral agents are used. The sooner drug therapy is prescribed, the lower the risk of death.
The post-infectious type of the disease is treated with corticosteroid drugs. High dosages are prescribed. The number of days of admission is determined depending on the severity of the disease and the general condition of the patient. Corticosteroids calm the immune system and reduce inflammation.
Autoimmune encephalitis is treated with:
- corticosteroids;
- plasmapheresis;
- immunoglobulin therapy.
Additionally, immunosuppressants may be prescribed.
Chronic encephalitis of the subacute type can only be resolved. In this case, death occurs within 1-2 years after diagnosis. In such situations, antiviral treatment is prescribed.
Concept
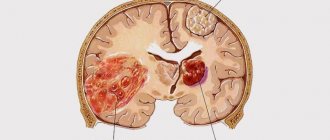
Viral encephalitis is a painful condition of the human body, manifested in inflammatory foci of a diffuse nature, which are localized in the tissues of the brain. The presented disease manifests itself as a result of specific viral microorganisms entering the body. The symptoms of the disease have various types of systemic disorders, all of which are directly dependent on the type of infection and the state of the patient’s immunity. In addition, it is composed of general infectious indications, cerebral manifestations and specific inflammatory foci.
Possible complications
In some cases, if treatment was started on time, the person recovers and does not suffer any complications after suffering from encephalitis. If the patient was delivered in serious or moderate condition, then there is a high risk of acquiring:
- aphasia (problems with the speech apparatus);
- memory problems (the most common complication);
- difficulty concentrating;
- epilepsy;
- instability of mood and emotional background;
- problems with physical activity;
- personal and behavioral changes.
What symptoms should you be wary of?
Naturally, many are interested in what signs can be used to unravel the disease. Evgenia Parshina lists a number of symptoms that are alarming and require consultation with a doctor. Among them:
- disorders of the nervous system. We are talking about both speech and hearing;
- development of psychomotor agitation;
- the appearance of hallucinations;
- development of cramps and spasms in the muscle area;
- problems with sensitivity of the body and face and other negative manifestations.
“When a doctor conducts a survey and collects a patient’s medical history to establish a diagnosis, you should draw his attention to the fact that, for example, you were recently bitten by a tick, especially if this happened while visiting endemic areas,” says Evgenia Parshina.
The pining of Rus'. What you need to know about the parasites that drink our blood Read more
FAQ
Who is most at risk for encephalitis?
Encephalitis is a rare disease, but it can manifest itself in representatives of both sexes. According to statistics, it most often affects people with weakened immune systems.
Can the vaccine cause encephalitis?
There really are such cases. But the risk of getting sick from what you are vaccinated against is much higher than the risk of getting a complication such as encephalitis. Therefore, it is unreasonable to refuse vaccination.
Next move
An inflammatory process of an encephalitic nature can cause a huge number of serious consequences, in particular the formation of swelling of the brain and the formation of a dislocation disorder, which provokes compression of the main organ in the area of the column. This process can be the main factor in death. If a coma develops, the person switches to a vegetative mode. The death of the patient in some cases is associated with the connection of microorganisms of an intercurrent nature, the progression of cardiac failure and respiratory failure.
With viral encephalitis, the patient begins to experience epilepsy, persistent neurological deficits, hearing loss, mental disorders, etc. According to the information received, the further prognosis for people with a similar disease depends on the form, severity of development and general condition at the beginning of treatment. Based on information from interviews with many medical workers, almost 30% of patients with the tick-borne form of the disease end up fatal. The Japanese stage is distinguished by a large number of deaths and a high percentage of residual consequences in those who have recovered from the disease. The post-vaccination form often has a favorable prognosis. The only exception is a disease that spreads after an anti-rabies injection like Landry's ascending paralysis and provokes the risk of death as a result of bulbar deformities.
In order to prevent damage to the body by such a disease, it is necessary to adhere to the following medical recommendations:
- Apply protective measures against insects that are active carriers of inflammation.
- Timely seeking qualified help from specialists if an infection occurs.
- Monitor your immunity level.
- Carefully choose doctors for vaccinations.
- Observe the dosage and administration of the drug.