Tests
Watch the video if you are too lazy to read
Watch the video if you are too lazy to read
- Rules
- Exercise
- Testing instructions
- Decoding the results
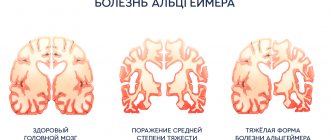
Alzheimer's disease is a neurodegenerative disease and the most commonly diagnosed form of dementia. The disease is named after the German scientist Alois Alzheimer, who was the first to describe the significant differences between dementia of neurodegenerative and vascular origin.
Alzheimer's disease is responsible for more than half of all diagnosed cases of dementia. At the same time, there is an increase in the number of cases around the world, mainly due to the aging of the world population.
Causes of Alzheimer's disease
© wildpixel / Canva
Work to establish the cause of Alzheimer's disease has been going on for many decades, but it is still not known for certain. There are only hypotheses, the most probable of which are the following:
- disturbances in the protein structures of neurons, complicating the transmission of signals between nerve cells and, ultimately, leading to their death.
- Infection of the brain by the bacterium Porphyromonas gingivalis, which lives in the oral cavity and causes gum disease.
- Accumulation of the beta-amyloid enzyme in the brain.
At the same time, factors that increase the likelihood of developing Alzheimer's disease are known for certain. The main ones are listed below:
- age;
- genetic predisposition;
- accumulation of aluminum in the body (in the brain in particular);
- arterial hypertension;
- smoking;
- overweight;
- diabetes;
- increased blood cholesterol levels;
- atherosclerosis.
Can Alzheimer's disease be cured?
© Ildar Imashev / Canva
Alzheimer's disease is a serious and incurable disease. As the disease progresses, a person develops cognitive impairment, worsens memory problems, develops speech disorders, executive functions, perception disorders, etc. At the stage of severe dementia, a person can no longer cope without outside help.
However, although Alzheimer's disease cannot be cured, modern medicine has methods that can stop or slow down the progression of the disease as much as possible. A responsible approach to the diagnosis and treatment of the disease allows a person to maintain cognitive functions until old age. Therefore, it is extremely important to identify signs of dementia at the earliest stages and consult a doctor in time for help. To do this, you need to know the symptoms of early manifestations of Alzheimer's disease.
Early symptoms and diagnosis of Alzheimer's disease
© Daisy-Daisy / Canva
When Alzheimer's disease develops, memory is the first to suffer. In this case, a person forgets recently occurring events or information received, while a person continues to remember events and knowledge acquired in the distant past well.
If you suspect Alzheimer's disease, you should consult a psychiatrist. The doctor will first ask the patient to take one of the cognitive tests. If, based on the test results, the doctor concludes that there are no impairments in cognitive functions, then the diagnosis will end, and the patient can be sure that at the moment he is not at risk of Alzheimer’s disease. If the test results are unsatisfactory, the doctor will refer the patient for more accurate examinations. In particular, the most accurate of them is brain imaging (magnetic resonance, computer, two-photon emission, etc.), which allows you to obtain layer-by-layer images of the brain and study its structure in great detail.
Cognitive tests that detect early Alzheimer's disease are simple and can be done at home. This is especially important given the fact that many older people refuse to see a doctor, unwilling to admit that they need help and treatment. Below are the most common tests and techniques practiced in clinics around the world.
Puzzle tests
Text from letters and numbers
People with Alzheimer's disease have difficulty reading. The text in the picture below can be quickly read and understood the first time only by a person who does not have problems with fluent reading. If a person sees only a meaningless set of letters and numbers, he may have a predisposition to Alzheimer's disease.
Extra digit
This is an attentiveness test. Ask the subject to find a six among the nines.
A healthy person will find a six in less than a minute. If a person takes more than a minute to complete this test, they may have a predisposition to Alzheimer's disease.
Optical-spatial activity
To complete this test, you will need to copy the following drawing onto paper.
Invite the subject to draw arrows from number to letter in increasing order: that is, from number 1 to letter A, then to number 2, etc. If a person connects the circles in the following order: 1-A-2-B-3-C-4-D-5-D, and the arrows do not intersect, the test is passed. If a person makes a mistake and does not notice it himself, he may have a predisposition to Alzheimer's disease. In this case, we recommend using more detailed tests (you will find them below).
The simplest tests for asthma
This includes the easiest tests in content, which can be used for diagnosis not only by potential patients, but also by their relatives and even acquaintances.
Picture test
The simplest test for predisposition to Alzheimer's disease. The subject is presented with a series of four pictures. Three depict the same object (often from different angles), the fourth shows a different one. You need to find the extra picture. If a person is unable to pass a picture test for Alzheimer's disease, this may indicate not only the presence of the pathology, but also a predisposition to it. Typically, the first manifestation of AD is considered to be problems with memory, especially with remembering new information. However, researchers at the University of Louisville discovered that some simple tasks require a person to use the medial temporal lobes. This can help detect the disease before the first symptoms appear, since it is in these areas that abnormal proteins (tau protein and beta-amyloid) begin to accumulate.
Arizona Questionnaire
The Arizona Questionnaire was created in 2012 for relatives of potential patients with AD. This Alzheimer's Predisposition Test helps you understand whether changes in your loved one's behavior, personality, or intellectual abilities are a cause for concern. It helps to identify initial changes in 90% of cases. Using tests, the first signs of Alzheimer's in adult women and men can be detected long before moderate and severe dementia develops. The sooner the patient begins therapy, the longer he will be able to maintain his usual lifestyle.
Mini-Cog test
© Robert Kneschke / Canva
The Mini-Cog test was developed at the University of Washington by Su Borson, an MD who specializes in dementia. The advantage of the test is its brevity and the ability to be performed by people who are not specialists in the medical field.
This short test is often used as part of the initial diagnosis of senile dementia of the Alzheimer's type and other types of dementia in older people. The Mini-Cog test allows you to evaluate a person’s short-term memory function, hand-eye coordination, and ability to perform tasks. It allows you to detect the development of Alzheimer's disease at the earliest stages.
Test rules
The test is quite simple and does not take more than five minutes. It consists of three actions:
- The subject is given 3 words: orange, window, pyramid. A person must repeat them and try to remember them.
- After which the subject must draw on paper a clock with hands indicating the time - twenty minutes to eleven.
- Then the subject must remember and name 3 words.
Scoring and evaluation of results
For each correctly named word after drawing a clock, the subject receives 1 point.
3 points
– no dementia.
1-2 points
if the clock is correctly depicted, there is no dementia.
1-2 points
If there are errors in drawing a clock, dementia is suspected.
0 points
– dementia is suspected.
Scientific basis for the effectiveness of the test
Although this test is used throughout the world for the initial diagnosis of Alzheimer's disease, there are studies confirming that the results of the Mini-Cog test cannot be fully trusted.
Researchers from the Department of Psychiatry at Queen's University in Kingston, Canada, conducted a meta-analysis examining four studies of the sensitivity and specificity of the Mini-Cog test for detecting Alzheimer's disease in primary care settings. These studies examined 1,517 cases in which the results of the Mini-Cog test were compared with the results of a diagnosis carried out in accordance with standard criteria for detecting Alzheimer's disease. According to the results of a meta-analysis published in 2018, the sensitivity of the Mini-Cog test varies from 76 to 100%. The scientists concluded that at the moment, including due to the small number of studies, there is insufficient evidence to recommend the Mini-Cog test for the primary diagnosis of dementia. You will find a link to the study at the end of the article.
Diagnosis of moderate and severe dementia in AD
The simplest tests for diagnosing Alzheimer's disease are KSHOPS and mini-COG. The techniques are aimed at detecting moderate or severe brain dysfunction, and cannot help diagnose dementia at an early stage. In addition, they confirm the presence of a problem, but do not always indicate the specific cause of its occurrence. But they are easy to carry out at home, and during the initial examination in the clinic, they quickly make it clear whether the patient has difficulties in realizing mental activity.
Mini COG
This test for signs of Alzheimer's disease takes about five minutes and confirms the diagnosis of dementia with a high probability. The test evaluates visual-spatial coordination and memory.
Memory
At the beginning of testing, the patient must memorize three words by ear. At the end he is asked to reproduce them. If only one or two of the three are named, then the presence of amnestic disorders is assumed. Impaired short-term memory function due to damage to the hippocampus is one of the first to appear in AD symptoms, so all initial tests for Alzheimer's disease are primarily aimed at identifying symptoms of amnesia. The presence of amnesia in combination with any other cognitive disorder allows for a diagnosis.
Drawing a clock
Coordination test or Alzheimer's test - clock (dial). This procedure is already more accurate compared to the first; it is used to carry out differential diagnosis. Can be used alone or as part of other tests (for example, SAGE). The subject must independently draw a clock face and place the hands at the indicated time. The result is assessed on a special scale with a maximum score of 10 or 6 points. To simplify, the patient may be asked to complete the arrows on the image of the dial. He will be able to pass the Alzheimer's test completely only if he draws the clock himself. If a person is unable to draw a clock, but draws the hands correctly, another type of dementia is suspected. Based on the shape of the elements of the resulting picture, a specific type of pathology is sometimes diagnosed.
Evaluation of the “Clock Drawing” test on a six-point scale
| Number of points | Image Features | Violations |
| 1 | The circle itself, arrows and numbers are depicted correctly, the arrows point to the specified time | No |
| 2 | Uneven spacing between numbers, the numbers themselves are drawn separately, the patient turns the sheet or draws lines for orientation | Small spatial errors |
| 3 | The arrow is missing, the time is marked with words or is not marked at all | Perception of symbols is impaired |
| 4 | Numbers are missing or drawn in the wrong direction, the circle is shown twice, the inscriptions are unreadable | Spatial disorganization, dysgraphia |
| 5 | Similar, only to a more pronounced degree | Severe disturbances in spatial orientation |
| 6 | The drawing does not look like a clock; all attempts to complete the task are unsuccessful. Sometimes the subject makes no effort at all | Definitely moderate to severe cognitive impairment |
KSHOPS or MMSE
This Alzheimer's disease screening test takes 10-15 minutes. Suitable for more advanced screening. Evaluates orientation in time and space, delayed recall, memory, speech, reading, counting, and concentration. Consists of 30 questions, the result is read on a scale of up to 30 points. This test for detecting Alzheimer's disease can be performed at home, but in this case its diagnostic value decreases. According to foreign studies, the sensitivity of KSHOPS is 1.0 and the specificity is 0.81. This means the test identifies 81 percent of people with dementia and correctly identifies 100 percent of those tested who do not have cognitive impairment. The procedure is well suited for detecting senile dementia of the Alzheimer's type.
Frontal Dysfunction Battery
The BDL test to screen for Alzheimer's disease is used for differential diagnosis. Consists of six tasks, average duration about 20 minutes. Vocabulary, praxis, ability to generalize, simple and complex forms of choice reaction, and reflexes are assessed. The maximum possible score is 18. To pass the Alzheimer's disease test, you need to score between 16 and 18 points. Using BDL, it is possible to confirm damage to the cerebral cortex, and the results of KSHOPS often show a high level. In moderate to severe dementia, both tests show low results. With a mild degree, at first there is a decrease in the KSHOPS indicators (less than 24 points), and the BDL results are close to normal. A person with a medical background must conduct and evaluate the test, since reflexes are also tested during the procedure.
Test "Drawing a clock"
© Peshkova / Canva
A very popular test for the initial diagnosis of Alzheimer's disease is drawing a clock face. This test is used in many methods of studying cognitive functions (including the Mini-Cog test described above).
The “Clock Drawing” test was developed more than a century ago – back in 1915. However, in those days it was used to diagnose aphasia and apraxia. It was only in 1989 that this test began to be used to diagnose cognitive impairment (link to material at the end of the article).
Exercise
Give the person a piece of paper and a pencil and ask them to draw a large round clock face with numbers and hands so that the clock indicates the time 11:10. The drawing is scored in points from 0 to 4. Only a result of 4 points is considered a sign of complete health. The lower the score, the more severe the Alzheimer's disease or other type of dementia.
Evaluating a drawing
To rate a drawing, add 1 point for each part:
1 point
for a vicious circle;
1 point
for depicting the numbers in the correct places on the dial;
1 point
for depicting all 12 numbers on the dial;
1 point
for correctly placed arrows.
Decoding the test result
Add up all points scored. If 4 points are scored, there is no dementia. Any result below 4 suggests Alzheimer's disease or another type of dementia. The more mistakes the subject makes in drawing a clock, the higher the severity of dementia.
Scientific basis for the effectiveness of the test
Scientists at University Hospitals Cleveland (Ohio, USA) conducted a study to determine the effectiveness of the Clock Drawing test for detecting Alzheimer's disease in the earliest stages, as well as to identify the most useful drawing elements for diagnosing this disease. The clock drawings of 41 patients over 39 years of age with MMSE test scores (presented below) of 24 points or higher were analyzed.
Based on the results of the study, scientists came to the conclusion that the most important diagnostic value is the image of the clock hands
. If you make two or more mistakes when drawing clock hands, there is a high probability of developing Alzheimer's disease in a person. In turn, the correct image of the clock hands does not exclude the possibility of developing Alzheimer's disease, but such a possibility is unlikely. You will find a link to the study at the end of the article.
Clinical Dementia Test GP-COG
GP-COG testing is used to pre-assess the risk of dementia. Each question is asked once. If the task is completed accurately, 1 point is given (indicated in parentheses).
- They name and ask to remember 5 words indicating the person’s address and name, for example, Moscow, Vernadsky Avenue, building 7, Ivan Andreev (not assessed).
- They ask you to name the date (1).
- Draw the dial (1).
- Show in the dial figure the correct location of the hands for the indicated time interval (1).
- Talk about recent news in the world (1).
- They ask you to give the address and name from step 1 (1 for each correct word).
If the score is 9, then the subject is mentally healthy. If the score is less than 8, proceed to the next stage and examine changes in cognitive function over time.
For each question there are 3 possible answers: “yes”, “no”, “I don’t know”. For each “no”, 1 is awarded.
- Has the patient's memory problems become more severe over the past 5 years?
- Are conversations that took place 2-3 days ago forgotten?
- Do you have difficulty finding words in a conversation?
- Do you have problems paying bills or shopping at the store?
- Are there any difficulties in following the doctor's orders?
- Have you encountered any problems when using public or private vehicles?
If the test taker answers all 6 questions; “No,” then he gets a 6, which rules out dementia. If the score is 0-3, the patient is asked to undergo additional tests for dementia.
Mini-Mental State Examination (MMSE)
©mail272/Canva
The Mini Mental State Examination (MMSE) is a short 30-point test that assesses the state of cognitive function and the degree of impairment. It is widely used in various clinics for the initial diagnosis of Alzheimer's disease, as well as for screening as it is treated.
MMSE was developed in 1975 by psychiatrists Marshall Folstein, Susan Folstein and Paul McHugh. Since then, this test has undergone minor changes, and is still used today in clinics around the world.
If anyone in your family complains of problems with short-term memory, concentration, mental arithmetic, speech, or other cognitive functions, suggest taking this test. It is quite simple and can be done at home.
Testing instructions
Orientation in time and space
The test subject must correctly name today's date, month, year, as well as the day of the week and time of year. Also, a person must correctly name his location: the name of the country, locality, region, house number or name of the institution, floor.
For each correct answer, 1 point is counted. For an incorrect answer - 0 points. Thus, the subject can receive from 0 to 10 points.
Perception
Ask the subject to remember three words that you tell him. Then say three words slowly and clearly: orange, window, pyramid (other option: apple, carpet, key). Then ask the person to say them.
For each word reproduced, 1 point is counted. Thus, the subject can receive from 0 to 3 points.
Concentration and mental arithmetic
Ask the subject to subtract the number 7 from the number 100 five times in succession (calculations must be done mentally). Thus, he must name 5 answers: 93, 86, 79, 72, 65. For each correct answer, count 1 point.
If the subject does not want to make calculations, offer another task: pronounce the word “EARTH” backwards. Score 1 point for each letter pronounced correctly. In other words, if the answer is correct, the subject must say “YALMEZ”, and he will be given 5 points. If the subject says “YAMLEZ”, only 3 points will be counted, etc.
Short-term memory
The subject must remember and say 3 words that you asked him to remember during the perception test. For each correct word, 1 point is counted. Thus, the subject can receive from 0 to 3 points.
Oral speech
Show the subject a wristwatch and ask him to name this item. Do the same with a stationery pen. For each correct answer, count 1 point.
Ask the subject to say the phrase “no ifs, ands, or buts.” If the phrase is pronounced without errors, count 1 point.
Thus, this task can be scored from 0 to 3 points.
Action in 3 stages
Give the subject a sheet of blank paper and say the following: “Take the sheet in your right hand, fold it in half and place it on the floor.” For each correctly performed action, count 1 point. The maximum number of points is 3.
Reading
Give the subject a piece of paper on which the command “CLOSE YOUR EYES” is clearly and legibly written, and ask him to do what is written on the sheet. If the subject closes his eyes, count 1 point.
Letter
Give the subject a blank sheet of paper and ask him to come up with and write down a meaningful sentence on any topic that will contain a noun and a verb. Spelling, grammatical and punctuation errors do not matter in this case. If the patient wrote a sentence, score 1 point.
Copying a drawing
Give the subject a blank sheet of paper and a sample drawing that shows two intersecting equiangular pentagons (as in the picture below). Ask to copy the drawing exactly. If the subject has drawn both pentagons, their lines are connected, and they intersect as in the sample, 1 point is counted. If one of the figures has more/less angles, the lines are open or the figures do not intersect, the point is not counted.
Test result evaluation
The result is calculated by summing the points scored for each test task. The maximum possible score is 30 points, which corresponds to a normal state of cognitive functions. The lower the total score, the more severe the degree of dementia. The result, depending on the amount of points scored, is interpreted as follows:
- 28 – 30 points:
cognitive abilities are normal. - 24 – 27 points:
there are cognitive impairments. - 20 – 23 points:
mild dementia. - 11 – 19 points:
moderate dementia. - 0 – 10 points:
severe dementia.
Scientific basis for the effectiveness of the test
Scientists at the University Foundation for Medical Sciences (Bogotá, Colombia) conducted a meta-analysis to investigate the effectiveness of the MMSE test for detecting Alzheimer's disease in people with mild cognitive impairment. The meta-analysis pooled and analyzed the results of 11 heterogeneous studies that examined data from 1569 patients with mild cognitive impairment.
In the meta-analysis, the researchers found no evidence to recommend the MMSE test as the sole diagnostic tool for identifying patients with mild cognitive impairment who are at risk of developing Alzheimer's disease. Doctors are recommended to use additional diagnostic methods in addition to the MMSE test. You will find a link to the study at the end of the article.
MMSE test
To determine dementia, they resort to the neuropsychological research method MMSE (from the English Mini Mental State Examination). In the Russian version, the test is called the Brief Mental Status Assessment Scale (KSHOPS).
We previously wrote a detailed article about the MMSE test (scale), and in this chapter we will look at it briefly.
The MMSE includes questions that are scored from 1 to 5 (indicated in brackets). The test questions are aimed at identifying violations:
- Time orientation (0-5). Indicate today's date.
- Terrain orientation (0-5). Name the country, city, address of the clinic.
- Memorization (0-3). 3 words are given. They need to be repeated.
- Attention (0-5). It is suggested to count backwards or subtract several times, for example, 25 from 500, or read the word backwards.
- Short-term memory (0-3). They are asked to name the words suggested in paragraph 3.
- Speech skills (0-2). You need to name objects and repeat the phrase.
- Motor skills (0-1). It is proposed to perform 3 actions, for example, they verbally give the command: take paper and pen, draw a circle, fold the paper in half.
- Reading and writing skills (0-3). Commands are written legibly on paper, asked to be read and followed. The first command is to perform a simple action. The second command is to write a meaningful sentence.
- Spatial thinking (0-3). It is required to redraw the proposed geometric shapes.
Decoding test results
For an error or leading questions in points 1, 2, 4, 6, the maximum possible score is reduced by 1 point. In points 3, 5, 7, 8, 9, one point is awarded for each correct answer.
If the sum of the test answers is in the range of 28-30, then the person being tested is healthy and has no signs of dementia. A result of 24-27 indicates mild cognitive impairment.
A total score of 20-23 indicates mild dementia. A score of 11-19 indicates moderate dementia. In severe dementia, the subject is unable to score more than 10 points.
The Alzheimer's Questionnaire
© Jivko / Canva
This questionnaire will help you determine whether someone close to you has Alzheimer's disease or whether there is no reason to worry. The test evaluates all of a person's abilities that are affected by the development of dementia. The questionnaire consists of 21 questions. For each affirmative answer, 1 or 2 points are counted, for a negative answer - 0 points. The higher the score, the higher the likelihood of dementia.
Memory
- Does your loved one have a bad memory? (Yes – 1, no – 0)
- If there are problems, have they gotten worse in recent years? (Yes – 1, no – 0)
- Does your loved one ask the same questions, repeat the same stories throughout the day? (Yes – 2, no – 0)
- Does he forget about planned activities or visits? (Yes – 1, no – 0)
- Does he lose things more than once a month? OR puts things in random places and then can't find them? (Yes – 1, no – 0)
- Does he express suspicions that things are being hidden, shifted or stolen from him when he finds it difficult to find them? (Yes – 1, no – 0)
Orientation in time and space
- Does your loved one often have difficulty remembering the time of day, today’s date, month, year? OR does he use the calendar or other sources several times a day to remember today's date? (Yes – 2, no – 0)
- Does he become disorientated in unfamiliar places? (Yes – 1, no – 0)
- Does he experience uncertainty and confusion when away from home or when traveling? (Yes – 1, no – 0)
Functionality
- Does your loved one have difficulty handling money, such as calculating change when shopping? (Yes – 1, no – 0)
- Does he have difficulty paying bills or handling finances? (Yes – 2, no – 0)
- Do his memory problems affect how regularly he takes his medications? (Yes – 1, no – 0)
- Does your loved one have difficulty driving? OR did he stop driving for reasons unrelated to physical limitations? (Yes – 1, no – 0)
- Does he have difficulty operating household appliances (microwave oven, stove, alarm clock, etc.)? (Yes – 1, no – 0)
- Does he have difficulty (not related to physical limitations) with chores? (Yes – 1, no – 0)
- Has your loved one given up or significantly reduced the time devoted to previous interests (sports, fishing, favorite craft, etc.) for reasons unrelated to physical limitations? (Yes – 1, no – 0)
Visuospatial orientation
- Does your loved one get lost in familiar places (not far from their own home)? (Yes – 2, no – 0)
- Does it happen that he chooses the wrong direction of movement? (Yes – 1, no – 0)
Speech
- Does it happen that your loved one cannot remember the appropriate words in a conversation (except names and titles)? (Yes – 1, no – 0)
- Does he confuse the names of family members or close acquaintances? (Yes – 2, no – 0)
- Does it happen that your loved one does not immediately recognize a person they know? (Yes – 2, no – 0)
Decoding the results
If you received less than 5 points
, this means your loved one does not have signs of dementia.
If the result is between 5 and 14 points
, your loved one should seek medical help because he has signs of mild cognitive impairment, which in the future may develop into dementia, incl. Alzheimer's type.
If you received more than 14 points
, it is likely that your loved one has already developed dementia and needs to seek medical help as soon as possible.
Development and scientific substantiation of the effectiveness of the questionnaire
In November 2010, a pilot project of the above questionnaire was published in the journal Alzheimer's Disease. Its development, analysis and research were carried out by a group of scientists with the support of the Banner Sun Health Research Institute (Arizona, USA) and a number of other scientific and medical centers. Scientists investigated the effectiveness and feasibility of using the above questionnaire for a more informative assessment of dementia.
During the study, the questionnaire was completed by informants of 188 patients, 50 of whom had normal cognitive abilities, 69 had mild cognitive impairment, and 69 were diagnosed with Alzheimer's disease. According to the results of the study, high sensitivity and specificity of this questionnaire was found to detect both mild and severe impairment of cognitive functions. At the same time, scientists noted that this questionnaire is not intended to completely replace the diagnostic examination of people with cognitive impairment. The full text of the study can be found at the link at the end of the article.