List of abbreviations
MRI - magnetic resonance imaging
NPN - neuroma of the hypoglossal nerve
SCT - spiral computed tomography
Neuroma is a benign tumor arising from the Schwann sheath of the cranial and peripheral nerves. Neuroma (schwannoma) of the hypoglossal nerve (HLN) is a fairly rare pathology, accounting for about 5% of all non-vestibular intracranial neuromas [1-5]. NPNs were first described by De Martel in 1933 (cited from [6]). At the same time, it was hypothesized that the site of initial growth of the IPN is the intracanal portion of the hypoglossal nerve (by analogy with vestibular neuromas, which almost always originate from the area of the internal auditory canal). Published by S. Weindling et al. [7] describing a series of 40 patients in whom lesions of this localization were determined, only 16 patients had NPN, in 15 cases juxtaarticular cysts were detected and in 9 cases bone cysts of the hypoglossal canal area were detected. Tumors can be sporadic (more often) or be a manifestation of neurofibromatosis type 2 [5, 7]. The disease is detected between the ages of 11 and 78.5 years (mostly at 37-56 years). The disease affects women somewhat more often [6, 7].
The manifestation of a tumor, as a rule, begins with deviation and hypotrophy of the tongue. As the tumor spreads to the brain stem and upper cervical segments of the spinal cord, pain in the cervical spine is added to the symptoms. When the walls of the hypoglossal nerve canal are destroyed, the bones that form the jugular foramen are destroyed, and the tumor affects the bulbar group of nerves, swallowing and phonation disorders occur. With compression of the brainstem and cerebellum, patients may exhibit static and gait disturbances and pyramidal insufficiency [1, 3, 5].
Magnetic resonance imaging (MRI) of the brain is the leading method for diagnosing the disease. The study identifies a tumor whose neuroimaging characteristics correspond to a neuroma of any other location. NPN at the stage of clinical manifestations has several clearly visible parts on MRI. The intracranial part of the tumor is located, as a rule, at the level of the craniovertebral junction and causes compression of the medulla oblongata. The intraosseous fragment of the tumor is located in the expanded canal of the hypoglossal nerve. The extracranial part emerges from the expanded canal of the hypoglossal nerve, compressing the internal carotid artery and internal jugular vein located here, the fibers of the first spinal nerves, as well as the roots of the caudal group of nerves. Spiral computed tomography (SCT) of the brain allows one to assess the bone anatomy, as well as the degree of destruction of the hypoglossal nerve canal and its relationship with the area of the jugular foramen [7].
According to the classification of NPN proposed by A. Kaye (1984), the following types of tumor are identified:
- type A - intradural tumor;
- type B - tumor of the “dumbbell” or “hourglass” type;
- type C - extracranial tumor.
Recently, type D has been additionally identified as a tumor of the peripheral parts of the hypoglossal nerve [2, 3, 5].
Patient management options, as with neuromas of other locations, include watchful waiting, surgery, and radiation therapy. Observational tactics are adopted when the patient refuses any treatment method or when a small tumor is newly detected [1, 3, 5].
For surgical treatment, retrosigmoid suboccipital, median suboccipital, transcondylar and far-lateral approaches are used [4, 5]. Until the 70s of the last century, postoperative mortality reached 50% and was caused, in most cases, by respiratory failure due to worsening bulbar symptoms. At that time, a recommendation was even made to perform a tracheostomy at the preoperative stage [4, 5]. Carrying out surgery at the present stage includes mandatory neurophysiological monitoring of the caudal group of nerves (IX-XII cranial nerves).
Total tumor removal, even under conditions of neurophysiological monitoring, is associated with a high risk of unfavorable outcome. It is only possible using a traumatic transcondylar approach, which also does not guarantee total removal, and the likelihood of complications is quite high [3, 5, 6]. Bulbar disorders in the postoperative period occur in 100% of cases, and the degree of their severity determines the outcome. They can be either transient, manifested by dysphonia, or permanent, up to the absence of any swallowing and breathing movements, which requires tube feeding and artificial ventilation. The most preferred tactics are subtotal tumor removal, achieving decompression of the brain stem and cranial nerves, followed by stereotactic irradiation of tumor remnants [3, 5].
Description of a clinical case
Patient B
., 43 years old, entered the clinic of the Federal State Institution “National Medical Research Center for Neurosurgery named after. acad. N.N. Burdenko" with complaints of pain in the cervical-occipital region, mainly on the right, which has been bothering her for the last 4 months.
During the examination, the clinical picture revealed: deviation of the tongue to the right, mild dysfunction of the bulbar group of nerves without impaired swallowing, pain in the cervico-occipital region mainly on the right, with irradiation to the right shoulder.
MRI of the brain with paramagnetic signal amplification revealed a parastem tumor on the right, compressing the medulla oblongata and emanating from the enlarged canal of the hypoglossal nerve. The smaller tumor component was located in the canal cavity and extended extracranially (Fig. 1).
Rice. 1. MRI of the brain of patient V. before surgery. When the signal intensifies, a tumor on the right is detected, corresponding to a neuroma, in the shape of a “dumbbell”, located in one part at the level of the craniovertebral junction and causing compression of the brain stem, and the other part in the bone structures.
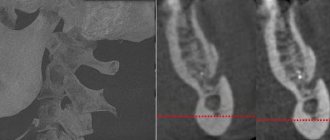
SCT of the brain in bone mode revealed an enlarged canal of the hypoglossal nerve with destruction of its walls. The posterolateral wall was practically absent, as a result of which the canal cavity communicated with the lumen of the jugular foramen (Fig. 2).
Rice. 2. SCT of the brain of patient V. in bone mode before surgery. Destruction of the hypoglossal nerve canal on the right is determined; the canal is separated from the cavity of the jugular foramen by a thin bone septum (indicated by an arrow).
Using diffusion tensor tractography, the caudal group of nerves and the corticospinal tract were reconstructed. The latter is compressed by the tumor and pushed to the left. The roots of the upper cervical segments of the spinal cord and hypoglossal nerve were located at the lower pole. The glossopharyngeal and vagus nerves were located at the upper pole of the tumor and were deformed (Fig. 3).
Rice. 3. Diffusion tensor tractography of the brain of patient V. before surgery. The corticospinal tract in the brain stem is identified, the glossopharyngeal and vagus nerves are located at the upper pole of the tumor, and the accessory nerve and CI root pass along the anterior pole. a - corticospinal tract, b - roots of the IX, X, XI cranial nerves, c - acoustic-facial group of nerves, d - tumor.
The patient underwent surgery to remove the tumor. In the “concord” position (lying face down on the operating table), a median suboccipital approach was performed with resection of the posterior arch of the CI vertebra and the squama of the occipital bone with lateralization of the trepanation window to the right. The dura mater is cut in an arcuate manner over the right hemisphere of the cerebellum and the brain stem to the CII vertebra and fixed with ligatures. The arachnoid membrane of the cistern magnum was opened, the cerebellar hemisphere was retracted using a spatula, a light yellow tumor with a capsule and a small number of vessels on its surface, emanating from the lateral part of the foramen magnum, was discovered. Neurophysiological monitoring of the cranial nerves on the inferior and anterior surfaces determined the location of the abducens nerve roots and the CI root.
At the oral pole there were also separate roots of the abducens nerve and the glossopharyngeal and vagus nerves. The tumor capsule was opened and its removal began. The tumor looked like a typical neuroma with a dense, low-bleeding stroma. After reducing the volume of the tumor, its lower part is mobilized. The vertebral artery and the posterior inferior cerebellar artery arising from it were found under the caudal pole. These vessels and nerves are separated from the tumor, and this part of the neuroma is removed. Then the upper part of the tumor was isolated, from which the roots of the IX-XI nerves were separated. Next, a well-defined dissection plane was found between the trunk and the tumor, along which the tumor was separated and removed to the very edge of the foramen magnum. It was established that the bulbar group of nerves went into the intact jugular foramen, and the tumor spread into the dilated and destroyed canal of the hypoglossal nerve. During exploratory stimulation of the hypoglossal nerve, it was not possible to clearly verify it as a structure; only a few positive responses were received from the surface of the tumor. The tumor most likely originated from the intracanal portion of the hypoglossal nerve. Under the arachnoid membrane on the anterior surface of the tumor, many roots became visible, responses were received from the IX-XI cranial nerves and an unclear response was received from the XII nerve. When the intracanal part of the tumor was isolated from the area of the jugular foramen, venous bleeding occurred. The tumor in the canal was just as dense; its isolation and aspiration with a vacuum aspirator was not possible. Considering that the intracranial paratrunk part of the tumor was completely resected and compression of the trunk was eliminated, and the intraosseous part of the tumor has no clinical significance, but its removal is associated with a high risk of complications, they decided to refrain from doing this. Thus, the tumor was removed subtotally. Hemostasis was performed, the dura mater was sutured hermetically, the bone flap was placed in place and fixed with bone sutures. The wound is sutured in layers. The progress of the surgical intervention is shown in Fig. 4.
Rice. 4. Progress of surgical intervention in patient V. a — dissection of the dura mater over the cerebellar hemisphere and brain stem; b, c — neurophysiological monitoring of the IX, X, XI cranial nerves was established; d — view of the tumor before removal; one of the roots of the 11th nerve is located on the posterior surface (arrow); d — opening the tumor capsule and reducing its volume; e — isolation and excision of the upper pole of the tumor; g — isolation of the superomedial part of the tumor, on which the root of the IX nerve is located (arrow); h - isolation of the lower pole of the tumor (on the surface of the tumor there are roots of the XI nerve and CI (arrow); i, j - isolation of the lower and inferomedial part of the tumor (the vertebral artery and the origin of the posterior inferior cerebellar artery are visible - indicated by arrows); l - after removal in the anterior part of the tumor, the roots of the IX, X, XI, XII nerves (arrows) are visible through the arachnoid membrane; m - stimulation of the roots of the caudal nerves (response received from all nerves).
During an MRI of the brain of patient B
. On the 3rd day after surgery, a residual part of the tumor was detected in the canal of the hypoglossal nerve (Fig. 5).
Rice.
5. MRI of the brain of patient V. on the 3rd day after surgery. When the signal is amplified with a paramagnetic agent, the remainder of the tumor is determined in the canal of the hypoglossal nerve on the right (indicated by the arrow). In the patient's neurological status, in addition to local pain, there was an increase in bulbar disorders, which were not an indication for the installation of a nasogastric tube or tracheostomy, and mild disturbances in static behavior and gait were noted.
Histological examination of the biopsy specimen shows a typical neuroma.
Next, radiation therapy is planned for the residual intracanal part of the tumor.
Symptoms of damage to the hypoglossal nerve
With neuropathy of the hypoglossal nerve, weakness of the tongue appears when speaking and difficulty swallowing. As the disease progresses, tongue weakness increases. Depending on the level of nerve damage, central or peripheral paresis develops. Peripheral damage occurs when the nucleus of the hypoglossal nerve, as well as the nerve fibers emanating from it, is damaged. Hypotonia of the tongue muscles on the affected side is noted, the surface of the tongue becomes wrinkled and uneven; muscle atrophy gradually appears in the tongue. A distinctive feature is fibrillary twitching in the muscles of the tongue. The tongue deviates in the direction of the lesion. Damage to the nerve on both sides is more severe (20%) - glossoplegia (immobility of the tongue) and speech impairment in the form of dysarthria occur.
| Peripheral type lesion of the left hypoglossal nerve | Damage to the left hypoglossal nerve of the central type |
A comment
The article presents a clinical observation of a case of schwannoma arising from the hypoglossal nerve with a predominant intracranial spread. Neuromas of the hypoglossal nerve can be localized both in the parastem zone and in the upper cervical region, although in some cases they take on an “hourglass” shape. Currently, fewer than 30 individual case reports of hypoglossal neuromas have been published, highlighting the rarity of this pathology. Specific neurological manifestations in the form of slowly progressive hemiatrophy and deviation of the tongue, accompanied by fasciculations, are complemented as the tumor grows by compression of the brain stem and damage to nearby cranial nerves. In cases where the tumor is located in the extracranial part of the hypoglossal nerve, difficulties in swallowing and local bulging in the upper cervical region are associated. A characteristic diagnostic sign of hypoglossal nerve neuromas emanating from the intracanal segment of the nerve is the expansion of the corresponding bone canal, demonstrated in the article. For neuromas of the hypoglossal nerve, accompanied by compression of the medulla oblongata and bulbar syndrome, the main goal of surgical intervention is decompression of the brain stem, which was successfully carried out by the authors of the article. When the tumor is intracranial, some authors use an extremely lateral, transcondylar approach, which facilitates total tumor removal. The choice by the authors of the article of a median approach with its lateralization towards the tumor seems justified, since it provides the least traumatic approach along the nuchal line, and staged intracapsular resection of neuroma allows timely detection of the plane of surgical dissection with the brain stem, vertebral artery and its branches and cranial nerves. The intracanal part of the tumor, the removal of which is often accompanied by venous bleeding from the tumor’s own vessels, and sometimes from the jugular vein bulb, in the absence of a bone wall with a sharply widened canal of the hypoglossal nerve, can not be resected, but, if necessary, subsequently subjected to radiosurgery. The presented observation, supplemented by a brief review of the literature, shows the success of the chosen tactics of surgical intervention, serves as an example of a successful solution to a complex clinical problem and emphasizes the professionalism of the authors.
Yu.A. Grigoryan (Moscow)
Treatment of hypoglossal nerve damage
- Anticholinesterase drugs, B vitamins.
- Oral hygiene.
- Treatment of the underlying disease.
Treatment is prescribed only after confirmation of the diagnosis by a medical specialist.
Essential drugs
There are contraindications. Specialist consultation is required.
- Prozerin (inhibitor of acetylcholinesterase and pseudocholinesterase). Dosage regimen: orally for adults, 10-15 mg 2-3 times a day; subcutaneously - 1-2 mg 1-2 times a day.
- Milgamma (B complex of vitamins). Dosage regimen: therapy begins with 2 ml intramuscularly 1 time per day for 5-10 days. Maintenance therapy - 2 ml IM two or three times a week.
What are the symptoms of the disease?
Symptoms of glossopharyngeal neurosis are characterized by the appearance of pain in the tonsils or root of the tongue, radiating to the throat, ear, palate, and less often to the neck and eyes. The average duration of pain attacks is 2 minutes. It is localized on the right side of the tongue, that is, it is one-sided. The main symptom of the disease, as with any other type of neuralgia, is severe pain. Sometimes patients complain of dry mouth during an attack.
In medicine, trigger zones are also identified, the irritation of which can cause an attack (palatine tonsils, arches). The disease can also be accompanied by a cough, decreased blood pressure, increased salivation, taste disturbances (a person thinks that everything is bitter), and the aggravation occurs in the autumn-winter period. All symptoms are individual and depend on the cause of neuralgia.
Effective treatment of the disease
If you suffer from neuralgia of the glossopharyngeal nerve, then contact us, where highly qualified neurologists with extensive experience will conduct a full examination, identify the causes of the disease and prescribe comprehensive treatment.
Our clinic is open every day, including weekends and holidays. The appointment is by appointment, you will not need to stand in line and spend a lot of time to get to the neurologist.
Treatment of this type of neuralgia takes place comprehensively after differential diagnosis. The doctor may prescribe an orthopantomogram - an x-ray of the upper and lower jaw. This will enable the doctor to identify enlargements of the styloid process. If it is normal, then a computer and/or magnetic resonance imaging of the brain is done, where the presence or absence of tumors, aneurysms, and skull injuries will be seen. Additionally, electroneuromyography is performed, which records nerve impulse disorders.
After the diagnosis is made, adequate treatment is prescribed - this can be surgical intervention, when during the operation the glossopharyngeal nerve is freed from compression by tissues. The doctor performs microvascular decompression of the nerve or resection of the styloid process, depending on the indications. During the operation, special endoscopic equipment is used, which makes it possible to cause fewer injuries and increase the success of the operation.
In addition to surgical intervention, physiotherapy and drug treatment are also used, in which a number of analgesics, antipsychotics and other drugs are prescribed.
Remember that glossopharyngeal neuralgia is treatable, and this can be done in our medical center!
Doctor's advice
Treatment of the disease is long, sometimes it takes 2-3 years until complete recovery, so be patient and follow all the doctor’s orders. In most cases, the disease appears regardless of the patient, that is, there is no prevention as such. The only thing that can be done is to avoid injuries to the jaw and head, and also not to trigger viral and infectious diseases.
| Make an appointment | Make an appointment by calling +7 (812) 600-67-67 or filling out the online form - the administrator will contact you to confirm your appointment |
UNION CLINIC guarantees complete confidentiality of your request.
Recommendations
A consultation with a neurologist and magnetic resonance imaging of the brain are recommended.
| • | Leading specialists and institutions for the treatment of this disease in Russia: |
| Doctor of Medical Sciences, Head of the Department of Russian State Medical University, Professor, Academician of the Russian Academy of Medical Sciences Gusev E.I. | |
| • | Leading specialists and institutions for the treatment of this disease in the world: |
| G. AVANZINI, Italy. |
Neuralgia of the glossopharyngeal nerve - causes
Glossopharyngeal neuralgia develops against the background of severe diseases of the skull or advanced infectious diseases. Causes:
- inflammation of the cerebral cortex;
- aneurysm;
- atherosclerosis;
- chronic tonsillitis, sinusitis, sinusitis, tonsillitis;
- tumors of the brain, pharynx, larynx;
- complications of infectious diseases such as influenza;
- tetraethyl lead intoxication;
- injuries of the tonsil spoon;
- laryngeal cancer;
- narrowing of the jugular foramen in the skull;
- ossification of the stylohyoid ligament.
As you can see, all diseases that cause neuralgia of the glossopharyngeal nerve are serious and require immediate treatment.
Incidence (per 100,000 people)
| Men | Women | |||||||||||||
| Age, years | 0-1 | 1-3 | 3-14 | 14-25 | 25-40 | 40-60 | 60 + | 0-1 | 1-3 | 3-14 | 14-25 | 25-40 | 40-60 | 60 + |
| Number of sick people | 0 | 0 | 0 | 0.3 | 0.5 | 0.8 | 0.8 | 0 | 0 | 0 | 0.3 | 0.5 | 0.8 | 0.8 |
Structure of the glossopharyngeal nerve
N. glossopharyngeus or glossopharyngeus nerve begins in the nuclei of the medulla oblongata. It is based on motor, sensory and autonomic parasympathetic fibers. Moreover, the sensory fibers begin in the sensory nucleus common to the vagus and glossopharyngeal nerves. They innervate the mucous membrane of the pharynx, soft palate, tongue, tonsils, and Eustachian tube. The sensation of taste in the anterior two-thirds of the tongue is provided by taste fibers emerging from the nucleus of the tractus solitarius. The taste fibers of the glossopharyngeal nerve are responsible for the taste sensations of the posterior third of the tongue and epiglottis.
The motor fibers originate in the nucleus ambiguus and innervate the stylopharyngeal muscle, which is necessary for raising the pharynx. Together with the vagus nerve, they form the reflex arcs of the pharyngeal and palatal reflexes.
Parasympathetic fibers originate in the salivary nucleus. Being part of the tympanic and lesser petrosal nuclei, they reach the autonomic ganglion, and with the branch of the trigeminal nerve they regulate salivation of the parotid gland.
Since the pathways and nuclei of the glossopharyngeal and vagus nerves are common, isolated pathology n. Glossopharyngeus. But more often symptoms of combined lesions are observed.
Diagnostic methods
The diagnosis is made by a neurologist, who, if necessary, can involve an otolaryngologist and dentist. During the examination, the doctor determines analgesia, that is, the absence of pain sensitivity at the base of the tongue, upper parts of the pharynx, and tonsils. Taste sensitivity is also studied, for which a taste solution is applied to symmetrical areas of the tongue. The diagnosis is confirmed by isolated unilateral taste disorder in the posterior third of the tongue. Bilateral disruption is typical for diseases of the oral mucosa, such as chronic stomatitis.
The pharyngeal reflex needs to be checked. To do this, touch the back wall of the throat with a paper tube, which provokes a swallowing movement and occasionally a cough. Normally, touching the soft palate should be accompanied by a lifting of the palate and uvula. Sicard syndrome is characterized by the absence of reflexes on one side. But a similar symptomatic picture can occur with damage to the vagus nerve. If the pharynx and pharynx are strewn with herpetic rashes, the doctor can diagnose ganglionitis of the ganglionitis of the glossopharyngeal nerve nodes, which differs in almost identical n. Glossopharyngeus clinical picture.
To establish the root cause of symptomatic neuritis, neuroimaging diagnostics is needed:
- MRI or CT scan of the brain;
- Electroencephalogram;
- Echo-EG;
- Ophthalmoscopy with consultation with an ophthalmologist.
It is necessary to distinguish between neuralgia of the glossopharyngeal nerve and diseases that cause painful paroxysms of the face and head. These include:
- Neuralgia of the ear ganglion;
- Trigeminal neuralgia;
- Oppenheimer's syndrome;
- Glossalgia;
- Ganglionitis of the pterygopalatine ganglion;
- Retropharyngeal abscess;
- Tumors of the pharynx.
Symptomatic picture
Clinical signs include painful paroxysms lasting from a few seconds to three minutes. A sharp acute pain originates at the root of the tongue and instantly spreads to the tonsils, soft palate, ear and pharynx. May radiate to the eye, neck and lower jaw. Pain can be triggered by coughing, chewing food, its temperature, yawning, swallowing and even talking. During paroxysm, dry mouth is noted, immediately after hypersalivation. But dryness is not a mandatory sign of diagnosis, because the secretory insufficiency of the parotid gland can be compensated by the remaining salivary glands.
Paresis of the levator pharyngeal muscle does not cause swallowing disorders. But difficulties in chewing and swallowing associated with impaired proprioceptive sensitivity, which is responsible for the position of the tongue, may be noted by patients.
The disease has a wave-like course, worsening in autumn and winter.