The risk of this disease increases in people over 45 - 50 years of age. Moreover, up to 40% of hemorrhages can be fatal. How to recognize the problem and what to do? Let's find out with the expert ALENA PARETSKAYA
Pathophysiologist, immunologist, member of the St. Petersburg Society of Pathophysiologists POLINA PETROSYAN Neurologist at SM-Clinic, specialist in cerebrovascular diseases and headaches
The second name for this pathology is hemorrhagic stroke. It occurs at any age, but most often mature and elderly people suffer - approximately 15 - 20% of all serious cerebrovascular accidents are caused by cerebral hemorrhage.
What is a cerebral hemorrhage
A cerebral hemorrhage is a life-threatening condition that occurs when one of the brain's arteries ruptures, causing blood to leak into the brain tissue.
The brain tissue becomes saturated with blood or a hematoma forms (an accumulation of blood that puts pressure on surrounding tissues); blood may leak into the ventricle of the brain, which disrupts the outflow of cerebrospinal fluid and increases intracranial pressure. The part of the brain that has lost blood due to rupture of blood vessels and those tissues that are saturated with blood stop working, the cells die. Accordingly, the larger the vessel that ruptures, the more dangerous the consequences will be for life and health.
Surgical treatment of cerebral aneurysms in the acute period of hemorrhage
5 / 5 ( 3 voices)
Photo from right to left: V. Dolens, A. Korolev (Head of Nho KOKB), J. Herniemi, A. Vorobiev
Non-traumatic intracranial hemorrhages due to ruptured aneurysms are one of the most severe forms of cerebrovascular accidents. In Russia, about 18,000 subarachnoid hemorrhages (SAH) are registered annually, i.e. 13 per 100,000 population per year. What is an aneurysm and who is it most common in?
SAH most often develops in middle-aged and elderly people. In patients aged 40 to 59 years, its frequency reaches 50%.
An aneurysm is a protrusion of the wall of an artery, usually at the bifurcation of the vessel or at the site where major branches arise from it. Characteristic of an aneurysm is the absence of a three-layer vascular wall - the absence of a muscle layer and an elastic membrane. The wall of the aneurysm consists of connective tissue that grows into the outer and inner membranes. The dome is represented by one thin inner layer, so bleeding occurs from here.
According to their configuration, they are saccular, fusiform and fusiform, as well as single-chamber and multi-chamber. Based on their size, aneurysms are divided into milranic (up to 3 mm), ordinary (from 4 to 15 mm), large (from 15 to 25 mm), and giant (more than 25 mm). Aneurysms are usually single, but can also be multiple (in 15% of cases), located on different arteries. In the overwhelming majority of observations (90-91%), aneurysms are located in the anterior part of the arterial circle of the cerebrum (circle of Willis) and only 9-10% of aneurysms are localized in the VSB.
Example of multiple aneurysms. Saccular and fusiform (fusiform) aneurysms of the right anterior cerebral artery (ACA).
An example of a multichamber aneurysm of the right MCA bifurcation.
In SAH, blood enters under the arachnoid membrane and spreads through the basal cisterns of the cerebrum. Blood also enters the cisterns of the posterior cranial fossa (prepontine, greater occipital, cerebellopontine angle) and then enters the spinal canal. The source and intensity of hemorrhage determine the nature of the spread of blood through the subarachnoid spaces - it can be local, or it can fill all subarachnoid spaces of the brain with the formation of blood clots in the cisterns. When brain tissue is destroyed in the area of hemorrhage, areas of parenchymal hemorrhage appear in the form of saturation of the brain matter with blood or the formation of a hematoma in the brain matter (subarachnoid-parenchymal hemorrhage).
Rupture of the PSA aneurysm with massive basal and parenchymal (and some ventricular) hemorrhage.
With a significant flow of blood into the subarachnoid space, blood reflux may occur into the ventricular system through the inversions of the fourth ventricle (foramina of Magendie and Luschka) and further through the cerebral aqueduct into the third and lateral ventricles. Direct penetration of blood into the ventricles of the brain through the damaged end plate is also possible, which more often occurs with rupture of an aneurysm of the anterior communicating artery (subarachnoid-ventricular hemorrhage). With significant parenchymal hemorrhage against the background of SAH, the hematoma may break through into the ventricles of the brain (subarachnoidal-parenchymal-ventricular hemorrhage).
Clinic for ruptured brain aneurysms.
The clinical picture of SAH with a ruptured aneurysm develops acutely, sometimes against the background of or after physical and emotional stress. A severe headache occurs. More often, patients describe it as a headache of a “burning”, “bursting” nature, “as if boiling water had been spilled in the head.” Against the background of headache, short-term or long-term depression of consciousness develops from moderate stupor to coma. In the acute period of hemorrhage, psychomotor agitation, hyperthermia, tachycardia, and increased blood pressure often occur. The neurological picture is characterized by the development of meningeal syndrome (stiff neck muscles, positive Kernig sign, photophobia, increased sensitivity to noise, etc.). A similar typical clinical picture of SAH is observed in 72% of patients. However, almost every third patient with SAH has a different clinical picture. The following atypical variants of SAH are distinguished, which are characterized by one of the leading syndromes: - migraine-like; - false inflammatory; - false hypertensive; - false-radicular; - false psychotic; - false toxic.
Neurological symptoms that develop with rupture of aneurysms of one location or another are caused not only by the effect of SAH itself or parenchymal hemorrhage, but also by ischemic changes in the brain tissue due to vascular spasm, and then the clinical picture of the disease is determined by the pool of spasmodic arteries, the degree of narrowing of the arteries and the characteristics of the collateral blood circulation In addition, when assessing clinical manifestations, it is necessary to take into account the timing of the disease, each stage of which is characterized by a certain frequency of occurrence and form of complications (repeated bleeding from the aneurysm, intracerebral hematoma, hemorrhage into the ventricles, hydrocephalus, arterial spasm and cerebral ischemia, electrolyte and endocrine disorders, cardiovascular and pulmonary complications, etc.). With all the diversity of the clinical picture in practical neurology and neurosurgery, classifications of the severity of the condition are used. To date, more than 50 classifications are known that are used to assess the severity of the condition in SAH. The most common of them is the classification proposed by W. Hunt and R. Hess
I. Asymptomatic or mild headache and mild neck stiffness. II. Moderate or severe headache, neck stiffness, cranial nerve palsy. III. Stupefaction, drowsiness, confusion. Moderate neurological deficit. IV. Stupor, moderate or severe hemiparesis, early decerebrate rigidity. V. Deep coma, decerebrate rigidity, appearance of a dying person.
Diagnosis of subarachnoid hemorrhages.
Verification of hemorrhage is traditionally performed by lumbar puncture.
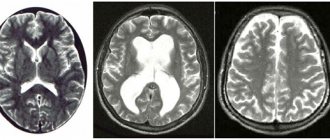
Computed tomography (CT) of the brain.
It is the leading method in diagnosing SAH, especially in the first hours and days of hemorrhage. Using CT, we determine not only the intensity of basal hemorrhage and its distribution in the cisterns, but also the presence and volume of parenchymal and ventricular hemorrhages, the severity of hydrocephalus, the presence and prevalence of foci of cerebral ischemia, the severity and nature of dislocation syndrome. In addition, with the help of CT, it is sometimes possible to diagnose the true cause of hemorrhage. The detection rate of SAH in the first 12 hours after hemorrhage reaches 95.2%, within 48 hours 80-87%; on days 3-5 - 75% and on days 6-21 - only 29%. The degree of detection of blood clots in SAH depends not only on the intensity of the hemorrhage itself, but also on the ratio of blood clots and the plane of sections on CT. The optimal condition for diagnosing SAH is when the plane of the clots is perpendicular to the plane of the CT slices and the thickness of the clots exceeds the width of the CT slice. Therefore, SAH is more often detected with blood clots thicker than 1.5 mm.
The most common CT classification of hemorrhage is the classification proposed by S.M Fisher et al. in 1980
CT data clearly correlate with the severity of the condition and prognosis of the disease. The more pronounced the hemorrhage according to CT, the more likely the development of cerebral vasospasm and, accordingly, fatal ischemic complications.
Diagnosis of the source of bleeding.
Direct visualization of an aneurysm is possible using three diagnostic methods: digital subtraction angiography (DSA), magnetic resonance angiography (MRA), and computed tomography angiography (CTA).
Diagnosis of cerebral aneurysms (CA) should begin with non-invasive methods. Computed tomographic angiography. Modern three-dimensional CTA with 3D reconstruction (KT-3D-A) has a sensitivity ranging from 87.9 to 97% and a specificity from 95 to 100%. With CTA, it is possible to obtain a three-dimensional image and determine the spatial configuration of the aneurysm and its relationship with nearby structures.
KTA. Aneurysm of the right vertebral artery.
Magnetic resonance angiography.
MRA provides verification of intracranial aneurysms with sensitivity ranging from 74 to 100% and specificity from 74 to 100%. The sensitivity of MRA in detecting aneurysms larger than 3 mm in diameter is 86%, which is comparable to the results of DSA. A decrease in the sensitivity of MRA was noted when the aneurysm diameter was less than 3-5 mm. There are a number of parameters that affect the ability of MRA to detect aneurysms: the size of the CA, the speed and direction of blood flow in the aneurysm relative to the magnetic field, thrombosis and calcification - therefore, MRA is preferably performed in the first 3 days after hemorrhage. In the period from 3 days to 3 weeks after hemorrhage, its accuracy decreases due to the biotransformation of the hemoglobin molecule. As a non-invasive method, MRA is widely used as a screening test in patients at high risk of having CA.
Digital subtraction angiography.
Selective DSA must be performed in the following cases: it is not possible to perform CTA or MRA; if these studies do not reveal the source of hemorrhage or the data obtained are insufficient for surgical intervention. The study should be performed in the following volume: both carotid areas and both vertebral arteries. DSA is carried out in direct, lateral, oblique, and, if necessary, in other atypical projections. In addition to identifying the source of hemorrhage, it is necessary to assess the severity and prevalence of vascular spasm and the characteristics of blood circulation. In the absence of visualization of the aneurysm during DSA in patients with a typical clinical picture of aneurysmal SAH, with angiographic signs of vascular spasm, it is advisable to perform a repeat angiographic study 3-4 weeks after the hemorrhage, which makes it possible to identify previously uncontrasted aneurysms in approximately another 3% of patients.
Diagnosis of vasospasm.
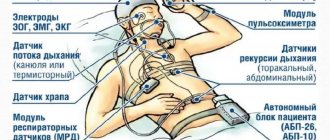
Vascular spasm develops exclusively with ruptures of aneurysms and is practically not observed with ruptures of arteriovenous malformations and SAH of other etiologies. Vascular spasm should be understood as changes in all layers of the arterial wall, leading to a narrowing of the lumen of the artery. They occur in response to hemorrhage in the cerebral cisterns. Morphological changes in the vascular wall are as follows: swelling and desquamation of the endothelium, contraction of smooth muscle cells with their subsequent necrosis and replacement sclerosis, destruction of elastic fibers of the outer and inner elastic membranes, collagen fibers of the adventitia. Such morphological changes lead to a narrowing of the lumen of the arteries, changes in the elastic properties of the artery, parietal thrombus formation and sometimes complete thrombosis of the cerebral arteries (in 20% of cases). From the morphological changes described above, it follows that, firstly, the term “vascular spasm” is very conditional, the term “constrictive angiopathy” is more appropriate, and secondly, it becomes more clear why therapy for arterial spasm with antispasmodic drugs is ineffective. Typically, vasospasm in SAH develops from 3-4 days from the onset of the disease, its peak is observed on days 7-14 and regression is observed in the following days. An important role in assessing the severity of vasospasm and the nature of cerebral ischemia developing in a patient is played by transcranial Dopplerography - TCD, EEG and registration of acoustic brainstem evoked potentials. TCD is the most sensitive method for diagnosing spasm. When the linear velocity of blood flow increases to 120 cm/s, the narrowing of the lumen is detected on angiograms, and when the linear velocity of blood flow increases to more than 200 cm/s, neurological disorders caused by cerebral ischemia are detected in patients.
Surgical treatment of patients with aneurysm rupture.
The main purpose of surgery in patients with aneurysms is to exclude the aneurysm from the bloodstream to prevent recurrent bleeding and to remove blood clots from the basal cisterns to prevent vascular spasm and cerebral ischemia. Considering that both ischemic complications and recurrent hemorrhage occur several days after aneurysm rupture, it is necessary to strive to perform the operation within the first 3 days of the disease. In cases of late hospitalization of patients with SAH and delayed diagnosis of an aneurysm, when vascular spasm and cerebral ischemia develop, surgery must be postponed for several weeks until the ischemic complications resolve. In the first 2 weeks after aneurysm rupture, repeated bleeding occurs in 15-20% of patients. In the first 6 months after aneurysm rupture, they develop in 50% of patients with a mortality rate of up to 60%. Subsequently, the risk of rebleeding is 3% per year with a mortality rate of 2% per year, which inclines many neurosurgeons to the tactics of early surgical interventions.
Indications for open surgical interventions.
1) patients with I-II severity of SAH according to Hunt-Hess; 2) patients with severity III of SAH according to Hunt-Hess with mild or moderate vasospasm (blood flow velocity in the M1 segment less than 200 cm/s); 3) patients with III-IV severity of SAH according to Hunt-Hess, if the severity of the condition is due to intracerebral hematoma with the development of dislocation syndrome.
Indications for delayed surgical treatment are:
1) III-IV severity of SAH according to Hunt-Hess in the presence of moderate or severe vasospasm (blood flow velocity in the M1 segment less than 200 cm/s), III-IV type of EEG changes; 2) anatomically complex aneurysms (giant aneurysms, aneurysms of the basilar artery); 3) V degree of severity of SAH according to Hunt-Hess without intracerebral hematoma.
Endovascular methods for treating aneurysms.
Absolute indications: 1) impossibility of clipping the aneurysm during open surgery.
Priority indications: 1) inaccessibility of the aneurysm for direct surgical intervention (aneurysm of the cavernous and paraclinoid sections of the ICA, vertebrobasilar region); 2) patients of the older age group (over 75 years old); 3) serious condition of patients (III-IV degree according to Hunt-Hess); 4) fusiform and dissecting aneurysms.
Surgeries for ruptured aneurysms are performed under general anesthesia, always using an operating microscope and microsurgical equipment.
A surgeon works with a microscope (Helsinki, Finland, Prof. Niemeli M.).
General view of the neurosurgical operating room (Helsinki, Finland).
The operation consists of several stages: craniotomy in the frontotemporal region, opening of the dura mater, dissection of the arachnoid membrane at the base of the brain and aspiration of CSF, isolation of the great vessels of the brain, isolation of the aneurysm-carrying artery, the aneurysm itself and its exclusion from the bloodstream by clipping.
Risk factors in aneurysm surgery in the acute period of hemorrhage are:
- serious condition of the patient (IV-V degree according to Hunt-Hess); - presence of widespread spasm and cerebral ischemia; - intracerebral hematoma with a volume of more than 30 ml; - breakthrough of blood into the ventricles of the brain and occlusive hydrocephalus; — displacement of the midline structures of the brain more than 5 mm.
Treatment in the postoperative period.
To date, there are no effective methods of drug therapy for vascular spasm. Therefore, when an aneurysm ruptures, to prevent cerebral ischemia or treat it, therapy is carried out aimed at normalizing cerebral perfusion. For this purpose, the so-called MN therapy (hypertensia, hypervolemia, hemodilucia) is widely used. It has not yet been established which of these components is most important. Blood pressure is kept at 15-20% above the normal pressure for a given patient using sympathomimetics. Hypervolemia is achieved by intravenous administration of albumin and plasma, hemodilution - saline. The hematocrit number should not exceed 38-40. Such therapy can significantly reduce the risk of developing cerebral ischemia (up to 15%) or reduce its severity. However, such therapy does not prevent the development of repeated bleeding from the aneurysm. In addition, with MN therapy, the risk of developing cardiopulmonary failure, renal failure, water and electrolyte balance disorders, and coagulopathies increases. To prevent ischemia and in its treatment, it is necessary to use a calcium antagonist - nimodipine. Being a calcium channel blocker, nimodipine prevents the flow of calcium ions through the damaged membrane into the cell and prevents its damage. Initially, the drug is administered intravenously through an infusion pump, bringing the infusion rate to 5 ml/hour, under the control of blood pressure, then administered orally. The use of the drug can reduce the number of neurological disorders caused by spasm by 12%. It must be remembered that with intravenous administration of nimodipine, arterial hypotension may develop, so sympathomimetics must be administered in parallel. maintaining normal brain perfusion.
When writing the article, materials from the methodological recommendations (No. 37) of the Moscow Department of Health 2008 were used. Developer institution: Research Institute of Emergency Medicine named after. N.V. Sklifosovsky. Compiled by: Academician of the Russian Academy of Medical Sciences prof. V.V. Krylov , Ph.D.
honey. Sciences A.E. Talypov. Author of the article: neurosurgeon Anton Viktorovich Vorobiev Frame around the text
Why choose us:
- we will offer the most optimal treatment method;
- we have extensive experience in treating major neurosurgical diseases;
- We have polite and attentive staff;
- Get qualified advice on your problem.
Causes of cerebral hemorrhage in adults
There are many reasons why blood vessels rupture and blood spills into the brain tissue. Among the most common are:
- arterial aneurysms (thinning of the wall, the formation of a sac with blood that overflows and bursts);
- vascular malformations (birth defects, thinning, tortuosity of the walls);
- ruptures of blood vessels during a hypertensive crisis due to the prohibitive load on the walls;
- head injuries with vascular ruptures;
- tumors that grow and damage arteries;
- taking blood thinning medications (if dosages are not followed);
- the development of certain systemic diseases in which the walls of the arteries are affected (for example, amyloidosis).
At a young age, the leading causes of hemorrhage are injuries and congenital vascular anomalies. In the elderly – damage to blood vessels by atherosclerosis and their rupture due to hypertension, tumor processes.
Causes and symptoms of ependymoma in adults
It is extremely difficult to establish the exact causes of cerebral ependymoma in adults. It is believed that the tumor appears under the influence of several provoking factors, including the influence of common viruses and chemical carcinogens. Clinical manifestations of the disease depend on the location of the tumor.
Ependymoma of the 4th ventricle of the brain
Ependymoma of the 4th ventricle is the most common. The clinical picture is associated with increased intracranial pressure due to impaired outflow of cerebrospinal fluid. Patients also experience classic focal symptoms.
Characteristic signs of ependymoma of the 4th ventricle:
- headache and other signs of intracranial hypertension;
- reflex tension of the neck muscles, forced position of the head;
- vomiting, combined with an attack of headache, which appears mainly after physical exertion and a change in body position;
- dizziness;
- tonic convulsions.
Ependymoma of the second and third degrees can cause mental disorders. The neoplasm affects the centers that are responsible for the adequacy of behavior and stress resistance. The disease requires a detailed and comprehensive examination and timely surgical treatment. Patients may die due to compression of the respiratory center and dislocation of the brain, in which its structures change their position.
Ependymoma of the lateral ventricles
When the tumor is localized in the area of the lateral ventricles, focal symptoms appear quite late. Clinical manifestations are associated with increased intracranial pressure, which causes headache, vomiting, signs of disorientation, and memory loss. Some patients may experience seizures.
As the tumor grows, the risk of hydrocephalus increases. It often leads to a crisis, severe headaches, vomiting and loss of consciousness.
Anaplastic ependymoma
According to the WHO classification, ependymomas can have varying degrees of malignancy. The most dangerous anaplastic tumor. It is classified as fourth degree malignancy. Anaplastic ependymoma of the brain is the most common and in most cases has an unfavorable prognosis.
Suspicion of the presence of anaplastic ependymoma is an indication for a qualitative examination. Differential diagnosis is carried out with glioblastoma. When contrast is used, heterogeneous accumulation of the drug is noticeable. In glioblastoma, the contrast agent is distributed peripherally.
The appearance of symptoms of brain ependymoma is an indication for contacting a neurosurgeon. Early initiation of treatment helps to take control of the patient’s condition and avoid dangerous complications.
Symptoms of cerebral hemorrhage in adults
The key symptoms that occur during a cerebral hemorrhage were given to us by neurologist Polina Petrosyan. According to her, intracerebral hemorrhage is characterized by an acute onset, with a rapid development of the clinical picture:
- sudden severe headache;
- nausea and vomiting;
- dizziness.
Depending on the volume and location of the hemorrhage, the following may occur:
- one-sided weakness in the limbs (hemiparesis) up to a complete lack of movement in them (hemiplegia);
- restriction of eyeball movement;
- speech impairment - both its reproduction and understanding;
- difficulty swallowing and breathing;
- disturbance of consciousness up to coma.
Much of the severity of symptoms depends on what part of the brain is damaged, how much blood leaks out, and how large the vessel is.
Symptoms
You can avoid the serious consequences of cerebrovascular accidents if you immediately identify the pathology and undergo a course of treatment. The main thing is to know what symptoms the victim is experiencing.
The initial period of hemorrhage with blood penetration into the lateral cavities of the brain is characterized by throwing back the head. In this case, the victim:
- The teeth are closed.
- Hands point inward.
- Fingers clenched into fists.
- Legs straightened.
- The feet are held in plantar flexion.
Also, one of the most pronounced signs of the development of a pathological process is a coma, but this occurs only when blood enters the brain cavity in large quantities. Often, coma in stroke victims with hemorrhage in the ventricles is registered in the first hours. If the hemorrhage is small, then consciousness is lost gradually.
With the accumulation of blood in the ventricular cavities and the development of cerebral edema, the degree of loss of consciousness increases. In such cases, other problems develop:
- Respiratory and cardiac disorders.
- Vasomotor disorders.
- Blueness, redness of the skin.
- A sharp increase in body temperature (when blood enters the third ventricle).
Spontaneous tonic spasms with throwing back of the head, convulsive seizures, and early hemiplegic contracture are recorded in victims. An increase in pressure in the cranial cavity may indicate the development of an acute circulatory disorder.
Intraventricular hemorrhage is usually accompanied by the rapid development of cerebral edema and the formation of hematomas. The healthy tissue surrounding the pathological focus is gradually compressed, as indicated by symptoms such as:
- Increasing severe headache.
- Nausea.
- Swelling of the optic discs and blurred vision.
- Convulsive seizures.
- Coma.
Often hemorrhage is accompanied by reflex paresis of the eyeballs, “floating gaze”, convergent or divergent strabismus. Signs of Babinski's symptom are also revealed, when the plantar reflex changes shape when stimulated by strokes.
In case of traumatic intraventricular hemorrhages, bilateral or unilateral lesions of the brain stem are detected. In this case, due to edema, the brain stem is displaced, as indicated by impaired consciousness, respiratory arrest, constriction of the pupils, and impaired pupillary reaction.
Diagnostics
A doctor may suspect a brain hemorrhage based on typical symptoms, especially if they are associated with injury or other risk factors.
But the gold standard for diagnosis is brain CT. On the first day after the onset of hemorrhage, the data will be most accurate, even more significant than with MRI. On tomograms, fresh hematomas are clearly visible; the doctor can determine their exact location, size and shape. In addition, he immediately assesses how damaged the brain structures, membranes and cerebrospinal fluid circulation system are. If hemorrhage is detected after 3 days or more, an MRI will be more accurate. It will better identify a hematoma in which the blood already has oxidized, partially disintegrating hemoglobin.
If these are young people without hypertension, they may be prescribed angiography of cerebral vessels. Additionally, an ECG, chest X-ray, blood tests for electrolyte levels, PTT with APTT (coagulation indices) are performed.
Consequences of cerebral hemorrhage in adults
The most dangerous thing with a cerebral hemorrhage is the consequences that can develop.
Among them, Polina Petrosyan notes: “The consequences can lead to disability, but may not affect a normal lifestyle and ability to work,” says Dr. Polina Petrosyan. – After hemorrhage, one-sided weakness in the limbs, decreased sensitivity in them, and various speech disorders may persist. Full recovery is possible if rehabilitation measures are taken in a timely manner and if the patient independently puts effort into rehabilitation measures.