Doctor of Medical Sciences, professor, oncologist, hematologist, radiologist (radiation therapist) of the highest category, Alexander Pavlovich Seryakov, in an interview with the portal of the Komsomolskaya Pravda publication, spoke about the causes and symptoms of the development of cancer, diagnostic and treatment methods.
Doctor of Medical Sciences, professor, oncologist, hematologist, radiologist (radiation therapist) of the highest category, Alexander Pavlovich Seryakov, in an interview with the portal of the Komsomolskaya Pravda publication, spoke about the causes and symptoms of the development of cancer, diagnostic and treatment methods.
Among all tumors in the central nervous system, spinal cord lesions account for approximately 12% in adults and about 5% in children. What is the cause of these pathologies and how are they treated?
Most often, tumors localized in the spinal cord are detected in people aged 30 to 50 years. Mostly, in about 85% of cases, they affect the membranes of the brain and surrounding structures.
What is a spinal cord tumor
“Spinal cord tumors,” says oncologist Alexander Seryakov, “are pathological neoplasms of a malignant and benign nature that are localized in the spinal cord. They are rare. By location there are:
- intramedullary (18 - 20% of cases) - grow inside the spinal cord;
- extramedullary (80 - 82% of cases) - located near the spinal cord, developing from nearby tissues.
Among benign lesions, the most common are ependymoma (63%) and astrocytoma (30%). Much less common are non-malignant hemangioblastoma and malignant oligodendroglioma.
Causes of spinal cord tumors in adults
The true causes of tumor growth that occurs in the spinal cord have not been determined to date. Scientists have identified a number of risk factors that may increase the likelihood of tumor growth in children or adults, but definitely do not lead to the formation of pathology. These include:
- hereditary predisposition (features of genes passed on from parents to children);
- exposure to substances with carcinogenic effects (chemical dyes, petroleum products);
- development of lymphoma (this is a malignant lesion in the lymphatic system);
- the presence of Hippel-Landau disease (a tendency to grow tumors, both benign and cancerous, is inherited);
- development of neurofibromatosis type 2 (this is a disease associated with gene breakdowns in which multiple tumors are formed - schwannomas or meningiomas in the area of nerves and the nervous system);
- exposure to harmful environmental factors (chemical pollution, radiation exposure);
- maintaining an unhealthy lifestyle - smoking, drinking alcohol, poor nutrition;
- constant stress;
- a sharp decrease in immunity;
- Excessive tanning (in a solarium, on the beach).
Often several factors influence at once and special conditions must be created for the tumor to begin to grow.
Treatment of gouty arthritis
The goal of treatment for gouty arthritis is to improve disease outcomes. For this purpose, mainly medicinal treatment methods are used. Non-drug methods are of auxiliary value.
Drug treatment
The main objectives of drug treatment of gouty arthritis are:
- relieving inflammation and pain in acute arthritis;
- preventing attacks of arthritis by reducing uric acid in the blood.
Treatment of an acute attack of arthritis
The following drugs are used to relieve an attack of gouty arthritis:
- Colchicine
is a dry extract of autumn crocus seeds. Available in tablets. Effective in the first 12 hours from the onset of a gout attack. The result of its use is the elimination of swelling and pain. The drug is prescribed in small dosages. The daily dose is divided into several doses. First, most of the daily dose is prescribed, then an hour later - a smaller one. If necessary, the dose can be repeated several times a day. A day after the onset of an attack, minimum dosages cannot be used; they are increased, which contributes to the manifestation of side effects, mainly from the gastrointestinal tract. All dosages are selected by the doctor. - Nonsteroidal anti-inflammatory drugs (NSAIDs)
– relieve inflammation, pain and swelling. These drugs are divided into 2 groups: non-selective and selective. Non-selective or 1st generation NSAIDs suppress the action of biologically active substances - prostaglandins, which support inflammatory processes. But they do not act selectively, also suppressing the action of prostaglandins that protect the gastric mucosa. Therefore, drugs such as Diclofenac, Indomethacin, Ibuprofen have side effects from the gastrointestinal tract (GIT). However, they are suitable for some patients and are often prescribed, both orally and intramuscularly. Selective NSAIDs (Nimesulide, Etoricoxib, Celecoxib) belong to the second generation. They act selectively on pro-inflammatory prostaglandins and have almost no effect on the gastrointestinal tract. The selection of the drug is carried out individually, in accordance with the characteristics of the patient’s body. - Glucocorticoid hormones (GCs)
- quickly relieve inflammation, pain and swelling, but are not suitable for everyone, as they can increase blood pressure, blood sugar and cause exacerbation of peptic ulcer disease. Prescribed in short courses orally (Prednisolone), intramuscularly (Betamethasone), in the form of intra-articular injections. Currently, they are trying to use mainly drugs from the NSAID group and only if there are contraindications for their use, GCs are used. - Canakinumab (trade name Ilaris)
is a monoclonal antibody to interleukin-1beta (IL-1b). IL-1b is a messenger protein molecule (cytokines) responsible for the inflammatory response. Antibodies bind to IL-1b and neutralize its action, which leads to the elimination of inflammation and pain. Canakinumab is used in an individually selected dosage for patients who have contraindications to the use of Colchicine, NSAIDs and GCs.
Drugs for the treatment of gouty arthritis
Decrease in uric acid levels in the blood during the interictal period
Outside of attacks, patients suffering from gouty arthritis are prescribed long-term courses of urate-lowering therapy (UST), which lower the content of uric acid (UA) in the blood serum, preventing the formation of UA crystals in tissues. With a low content of uric acid in the blood, the crystals already present in the tissues gradually dissolve. In the presence of chronic gouty arthritis and tophi, the UA content is reduced to a minimum (below 0.3 mmol/l), which contributes to the accelerated elimination of tophi. In the absence of tophi, an acceptable UA content of 0.36 mmol/l is acceptable.
For urate-lowering therapy for gouty arthritis, the following groups of drugs are used:
- A group of drugs that interfere with the formation of uric acid. They suppress the action of the enzyme involved in the formation of uric acid. When prescribing them, constant monitoring of UA content in blood serum is necessary. These medications include:
- Allopurinol is a drug that has been used to treat gout for more than 50 years. It is prescribed in long courses 2 weeks after the end of a gout attack with small doses, which are gradually increased to the required levels. Sometimes it gives side effects from the kidneys, liver, severe allergic skin reactions. At the initial stage of treatment, it often causes an exacerbation of gouty arthritis, so it is combined with the prescription of NSAIDs.
- Febuxostat (trade names: Adenuric, Azurix) is a more modern drug of this group; it acts selectively on only one enzyme involved in the synthesis of uric acid. It does not inhibit other enzymes, so it has fewer side effects. It works softly and effectively. Doses are selected individually and initially combined with the use of NSAIDs.
- Drugs that enhance the excretion of sUA through the kidneys. Prescribed for intolerance to drugs of the first group or ineffectiveness of their use:
- Probenecid - prescribed in long courses, contraindicated in the presence of kidney stones.
- Enzymes that are absent in humans can reduce the level of sUA in the blood. The enzyme uricase is present in the blood of some mammals and reduces the level of UA in the blood, but it is not present in human blood. The drug rasburicase (recombinant bacterial uricase) was produced using genetic engineering from bacteria, which is used for gouty arthritis if other methods fail to reduce UA in the blood. The disadvantage of the drug is increased allergenicity, so it is used strictly according to indications.
Peguricase is a uricase with polyethylene glycol, which suppresses increased allergenicity. A more modern drug, but it is also used strictly according to indications.
Crunching in joints - when to worry
Intra-articular injections of hyaluronic acid
Non-drug treatment
This type of treatment includes:
- diet;
- control over the course of comorbid (often combined with gout and aggravating its course) diseases;
- physiotherapeutic procedures;
- folk remedies.
Diet for gouty arthritis
Patients suffering from gouty arthritis should not consume foods rich in purine bases. But recent studies have found that only animal products have a negative effect. This is fatty red meat, offal (liver, kidneys, heart, brains), strong meat broths, canned fish in oil, canned meat and pates.
On the contrary, plant foods containing purine bases should not be completely excluded from the diet. These are nuts, peas, beans, lentils, legumes, cocoa and coffee. Dairy-vegetable diets with low-fat dairy products, a variety of vegetables and fruits are very useful. Especially useful are foods rich in vitamin C, which helps eliminate uric acid.
Alcohol should be excluded from the diet: strong spirits and beer, including non-alcoholic beer. Only a small amount of dry wine is allowed. You should not consume sweets, baked goods, and especially sweet carbonated drinks. It is also necessary to stop smoking.
Monitoring the course of comorbid diseases
Gouty arthritis is often combined and aggravated by obesity, diabetes mellitus, cardiovascular and kidney diseases.
Obesity requires constant monitoring of body weight. This includes following a diet with a reduced daily caloric intake, an active lifestyle, and courses of therapeutic exercises.
Diabetes mellitus also requires constant monitoring, laboratory monitoring and supportive treatment.
Frequent concomitant diseases with gouty arthritis are also arterial hypertension (consistently high blood pressure) and coronary heart disease with angina attacks. Currently, there are medications that can stabilize the condition of such patients, but this requires constant monitoring by a cardiologist.
Any renal pathology also complicates the course of gouty arthritis. She also needs to be observed and treated.
Physiotherapeutic procedures
Physiotherapy is an additional treatment for gouty arthritis. During a gouty attack, electrophoresis with glucocorticoid hormones and ultraviolet irradiation of the affected area are prescribed.
Electrophoresis with glucocorticoid hormones and ultraviolet irradiation are used to treat gouty arthritis.
During the period of remission, courses of magnetic and laser therapy are prescribed to improve blood microcirculation and restore damaged joint tissue.
In the absence of gout attacks, sanatorium treatment can be carried out for six months. The Caucasian Mineralnye Vody and Crimea sanatoriums are suitable.
Read about other methods of treating arthritis in this article.
Folk remedies
To relieve inflammation, swelling and pain during a gout attack, traditional medicine recommends compresses with activated carbon. Previously, charcoal was used for this purpose, today it is enough to take 50 tablets of activated carbon, crush, dilute with water to the consistency of homemade sour cream, add a tablespoon of vegetable oil, mix and apply to the inflamed area, apply a napkin, compress paper, cotton wool on top, bandage and leave all night long. Perfectly relieves inflammation, swelling, reduces pain.
Surgery
For large tophi, which often suppurate and compress surrounding tissues, disrupting their function, they are removed.
Surgical operations aimed at restoring joint function are carried out strictly according to indications, in case of destruction of cartilage tissue, proliferation of bone tissue with articular deformation and loss of limb function. If the joint is completely destroyed, it is replaced with an artificial one (endoprosthetics).
Symptoms of a spinal cord tumor in adults
There are no typical or characteristic symptoms only for a tumor; all signs can mimic other diseases, especially in the early stages. Therefore, you should consult a doctor to determine or rule out the problem with the following complaints.
- Pain syndrome. The most common manifestation of a tumor is pain that occurs in the area of the spine where the tumor began to grow. In the early stage, the pain may be mild or more severe, but there are no significant neurological symptoms. As the tumor progresses, disturbances in sensitivity and movement occur, the pain becomes stronger against the background of coughing or sudden movements, sneezing, physical activity, at night and when moving, tilting the head.
- Movement disorders. Muscle weakness is also possible, which occurs in combination with sensitivity disorders, the phenomenon of muscle atrophy, sharp and sudden contractions, twitching of muscle groups that are relaxed.
- Sensitivity disorders. Sometimes there is no pain, but superficial sensitivity may suffer, while maintaining a deep tactile sense. The patient may not feel pain, temperature, or touch, but perceives pressure and vibration.
- Problems with the functioning of the sphincters. Possible disturbances in urinary functions and, less commonly, bowel movements. This leads to retention of urine or stool.
Also, as the process progresses, scoliosis of the spine may occur, which is formed due to pain, motor dysfunction or destruction of the vertebral bodies.
It is impossible to identify spinal cord tumors externally; they are located quite deep in the spinal canal.
Causes of bone marrow edema
Damage to the spongy substance most often occurs due to back injuries (falls, bruises, wounds, etc.). If the vertebral body is damaged, the following are possible:
- violation of the integrity of bone structures;
- ruptures of lymphatic and blood vessels;
- release of liquid exudate into the area of the spongy substance.
The swelling observed in this case is called primary. The process can spread to paravertebral tissues (muscles, tendons, ligaments, synovial membranes).
The causes of secondary bone marrow edema are pathological phenomena in the surrounding tissues:
- infectious diseases (spondylitis, osteomyelitis, spinal tuberculosis);
- inflammatory changes in articular elements in osteoarthritis;
- allergic reactions;
- benign and malignant neoplasms;
- spine surgery;
- endocrine pathologies and diseases accompanied by impaired cellular metabolism;
- degenerative-dystrophic phenomena (osteochondrosis, hernias, deforming arthrosis, etc.)
Inflammatory processes in the vertebral bone tissue increase the permeability of the capillaries of the spongy substance and are accompanied by the active release of liquid exudate into the intercellular space. Diseases that occur with the formation of multiple purulent foci, which provoke an increase in swelling of the surrounding structures, are dangerous.
As the oncological process develops in the vertebral area, the trabeculae are destroyed. There is perifocal edema localized in the bone marrow area. Malignant tumors can damage blood vessels, increasing the amount of fluid in the spongy substance.
Metastases on MRI, signs of perifocal bone marrow edema
Degenerative-dystrophic pathologies lead to changes in the structure of the vertebra, reduce tissue trophism and cause aseptic inflammation of bone and cartilaginous elements. Subarachnoid and trabecular edema may develop.
Bone marrow overhydration in most cases is a protective mechanism in case of damage to the spongy substance. To effectively treat pathology, it is necessary to find out the cause of the pathology and eliminate the damaging factor.
Classification of spinal cord tumors in adults
There are many options for classifying tumors localized in the spinal cord. It is possible to divide into groups according to a number of characteristics - the location of the tumor focus relative to the spinal cord, spine or meninges, features of the histological picture, as well as the specific location of the lesion.
If we divide tumors by origin, they can be classified into two groups:
- primary is tumor tissue that developed from the cells of the spinal cord itself, its roots or membranes;
- secondary are tumors of a different localization that affect the spinal cord (including metastatic ones).
Based on the location of the tumor, they can be divided into several groups:
- extradural tumor - a lesion above the area of the dura mater;
- intradural – tumor under the dura mater;
- intramedullary - grows inside the spinal cord, originating from its cells.
Tumors can be located behind the spinal cord, in front, on the sides, affecting the cervical or thoracic, lumbar or sacral regions.
There is a very wide classification based on the origin and type of cells; tumors are determined based on biopsy data.
Types of Spinal Tumors
Benign Tumors
The term benign tumor is used to refer to tumors that have a low likelihood of spreading (metastasizing) to other organs and tissues. But, nevertheless, benign tumors can also cause big problems due to compression of tissues or blood vessels. Fortunately, most benign tumors can be successfully treated.
The following are examples of benign tumors that can occur in the spine or surrounding tissues:
Osteoid osteoma is a benign tumor that has the unique feature of occurring on the back of the vertebrae during puberty. It develops primarily in the legs and back, and not in the vertebral body. This type of tumor occurs in approximately 10% of all spinal bone tumors. Typically manifested by back pain, especially at night, and the use of aspirin or other NSAIDs (for example, ibuprofen) is quite effective. Often poorly visualized by radiography and therefore preferable to CT. Treatment options include long-term use of NSAIDs or surgery (especially radiofrequency ablation). With surgical treatment, pain quickly disappears and relapse is extremely rare.
Osteoblastoma is a variant of osteoid osteoma measuring more than 2 cm. It is also characterized by localization in the posterior part of the vertebrae. But the symptoms of osteoblastomas are more pronounced and surgical treatment is usually required. The recurrence rate is significantly higher than that of osteoid osteoma and is up to 10% (and in the same place).
Aneurysmal bone cyst. This is a benign tumor that often occurs in the cervical spine and can affect the posterior elements of the vertebrae or the vertebral body itself. These tumors are more common in older adolescents and present with pain and, in some cases, other neurological problems. Therapeutic measures for this type of tumor are excision of the tumor, curettage of the affected area and, if necessary, decompression of the spinal structures.
Giant cell tumors are poorly understood. They tend to be located in the vertebral body (the front side of the spinal column), and although technically "benign", they can be very aggressive and sometimes spread to other tissues. They may present with pain or symptoms of spinal cord compression. They most often occur between the ages of 20 and 40, but are also possible at other ages. Treatment of these tumors is surgical (resection or total removal of pathological tissue) and surgical treatment is the treatment of choice. In some cases, tumor embolization and preoperative irradiation are performed and this improves the results of surgical treatment. They can present local pain as well as symptoms of spinal cord compression. These tumors require a careful preoperative approach. Incomplete removal of a giant cell tumor can lead to possible malignant transformation.
Eosinophilic granuloma : a benign bone lesion characterized by pain and a characteristic radiographic appearance of “vertebra plana” - flat vertebrae, thinning of the vertebral bodies. It occurs in both children and adults. These tumors can occur either independently or as part of a syndrome with damage to other organs and tissues. Treatment of such tumors is selected individually, and different treatment methods are used, both surgical and radiation.
Enchondromas are benign tumors consisting of cartilage. Potentially, when enlarged, these tumors can affect spinal structures. The recommended treatment is surgery. Sometimes it is possible to transform these tumors into a poorly differentiated malignant cartilaginous tumor - chondrosarcoma. Fortunately, this happens quite rarely. But the rapid development of a tumor requires a mandatory biopsy, and this helps prevent the malignancy of a benign tumor from becoming malignant.
Malignant Tumors
Doctors use the term malignant to indicate the possible invasion of a tumor into other tissues and organs. Accordingly, the treatment of malignant tumors is much more difficult than the treatment of benign tumors (less prone to invasive growth)
The following are examples of malignant tumors that can occur in the spine and surrounding tissues:
Metastases. Any malignant tumor can metastasize to bone tissue, but most likely to spread from the following organs: breast, prostate, kidney, thyroid, and lungs. Hematogenous metastasis can occur in two ways: through the venous system or through the arterial system. The spine and its surrounding tissues have a good blood supply, with drainage of many structures of the pelvic area through the venous system called Bateson's plexus. Lymphatic channels can also be a route of metastasis, but only in a third of cases. Spread or metastasis of tumors from anywhere in the body to the spine is possible after a long period of tumor growth in the primary site. Metastatic tumors are usually accompanied by severe pain. If the metastatic tumor is large enough, then a compression effect on the spinal cord is possible, which can manifest itself as impaired conduction of the motor functions of the limbs, dysfunction of the intestines and bladder. As a rule, metastatic cancer is not curable, and the goal of treatment is aimed at reducing pain and decompressing neural structures (by surgical methods) and thus preserving the patient’s quality of life to the maximum extent possible. Surgery, chemotherapy, and dosed radiation therapy help reduce pain from spinal metastases.
Myeloma is the most common type of primary, malignant bone tumor. Typically, the disease occurs in adults over 40 years of age. Various bone tissues are involved in the process, including the spine. Pain syndrome is most characteristic of this disease. But sometimes lesions of the spine can occur without pain for a certain period of time. Treatment for this disease is palliative (implying only a reduction in symptoms, but not a cure). Chemotherapy is used to reduce pain and slow tumor progression. Surgical treatment is used in the presence of fractures or the need for decompression of spinal structures.
Osteogenic sarcoma is the second and most common primary malignant tumor of bone tissue. There are two age groups in which this type of tumor develops more often: adolescents, young adults and the elderly. Spinal involvement with this tumor is quite rare. Modern advances in neuroimaging, chemotherapy, and surgical treatment of osteosarcoma have significantly improved 5-year patient survival to 80 percent. This is a significant medical success, since 20 years ago this tumor was almost always fatal.
Leukemia . Various forms of leukemia may be accompanied by pain in the lower back or neck, which is caused by degeneration of the bone marrow of the vertebrae. But with leukemia, general symptoms such as anemia, fever, general weakness bother the patient much earlier than back pain.
Diagnostics
Diagnostics is a step-by-step process that allows you to determine the size and type of tumor and draw up a plan for its treatment. First of all, the doctor is interested in the patient’s complaints, symptoms, and medical history. It is important when symptoms developed and how they changed over time.
A full neurological examination is also carried out - determination of muscle tone, reflexes, muscle strength, spinal mobility, sensitivity.
To refine the pathology you need:
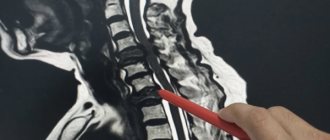
- MRI with contrast - this method helps to determine the condition of the entire spinal cord, its structures and determine the tumor;
- CT myelography is a technique for assessing the tumor border;
- diffusion-weighted and diffusion tensor MRI;
- scintigraphy;
- direct angiography.
After clarifying the type, location and size of the tumor, a treatment plan is drawn up.
Symptoms
Pain can be a symptom of a spinal tumor, especially if it is resistant to treatment and is accompanied by other symptoms such as weight loss and fatigue. The pain may be worse at night and may not necessarily be related to activity level. When there are other neurological symptoms (fecal incontinence, difficulty urinating, radiating pain), then suspicions in favor of the tumor nature of the symptoms increase. In addition, the presence of bruises, skin changes or other manifestations of the possible presence of a tumor in other parts of the body is important.
Symptoms depend on the location, type of tumor, and the general health of the person. Metastatic tumors (those that have spread to the spine from other organs) often progress quickly, while primary tumors often progress slowly over weeks to a year.
Intramedullary (within the spinal cord) tumors usually cause symptoms that damage most of the torso. Extramedullary (outside the spinal cord) tumors can develop for a long time before causing nerve damage. The most typical symptoms for spinal tumors are:
Backache
- Can be in any area, but most often in the middle of the back and lower back
- Worsens when lying down
- Intensifies with coughing, sneezing, stress, etc.
- Pain may radiate to the hip, leg, or arms
- The pain can be diffuse in all extremities.
- The pain may be localized in a specific area of the spine.
- Pain tends to progress
- The pain is intense and is not relieved by analgesics
Sensory disorders
- More in the legs
- Sensory disturbances tend to progress.
Motor impairments (muscle weakness)
- More in the legs
- Gait disturbances (difficulty walking)
- Muscle weakness tends to progress.
- Falls while walking or standing
- Feelings of cold feet or hands
- • Fecal incontinence
- • Urinary incontinence
- • Paresis or paralysis of muscles
- Fasciculations (muscle twitching)
Diagnostics
Most spinal column tumors are discovered during routine examinations performed in the presence of neck or lower back pain. The examination begins with a physical examination. If there are tumors in other organs, it is necessary to inform the doctor as necessary for an adequate examination. X-rays are used to diagnose bone changes in the spine. But the X-ray results are not informative enough. And when there is a need for clearer visualization of both bone tissue and soft tissue, a CT or MRI is prescribed. In addition, if a malignant tumor in the spine is suspected, scintigraphy may be prescribed. Laboratory studies are necessary to clarify the nature of the tumor and possible complications from other organs and systems (especially with malignant tumors).
Modern methods of treatment
“The main type of treatment,” says oncologist Alexander Seryakov, “is a neurosurgical operation in which the tumor is completely removed and decompression (removal of compression) of the spinal cord is performed. Micro-neurosurgical techniques, intraoperative neuroimaging and neuronavigation are often used.
For malignant tumors of the spinal cord, in addition to surgical treatment, the patient may be prescribed chemotherapy and radiation therapy (stereotactic radiotherapy and radiosurgery using linear accelerators of the CyberKnife type).