How the hypothalamic-pituitary system works: features of regulation, functions, processes
The action of the hypothalamic-pituitary system is possible due to the constant communication between these organs. Here are the features of the regulation of processes and functions of this axis:
- Hypothalamus
As a structure of the nervous system, it constantly receives a huge amount of information from all parts of the body. In response, it can generate different types of reactions - stimulating other areas of the brain or producing a hormone, a chemical particle that can carry information. Here are some other processes that occur in this part of the brain:
- Pituitary
An important mediator in the hormonal activity of the hypothalamus. Hormones from the hypothalamus reach the pituitary gland in two ways. The first is the direct transmission of hormones along nerve fibers. This is how vasopressin and oxytocin are transported. Once produced in the hypothalamus, they are sent to the posterior pituitary gland, from where they then enter the bloodstream.
The second method is with those hormones of the hypothalamus that control the functioning of the pituitary gland. These include various subtypes of releasers (excitatory hormones) and statins (inhibitory hormones). Hypothalamic liberins and statins travel from the hypothalamus to a special network of tiny blood vessels through which they travel directly to the pituitary gland. When in contact with the cells of the anterior pituitary gland, they regulate their activity and the production of pituitary hormones.
Although the hypothalamus is the primary structure of the hypothalamic-pituitary axis, the connection can be bidirectional. The pituitary gland also has the ability to influence the hypothalamus. The adjustment of the entire axis is based on so-called positive and negative feedback. When hormones are released from the pituitary gland, their blood levels increase and the hypothalamic-pituitary axis is suppressed. On the other hand, if this hormone is needed, the hypothalamus stimulates the pituitary gland and increases its secretory activity. The correct functioning of the feedback system is a necessary condition for maintaining homeostasis, that is, the internal balance of our body.
Hypothalamic-pituitary hormones in the human body
The hypothalamic-pituitary axis is a “two-story” system with many interconnections. None of its structures will be able to perform its function independently. The hypothalamic-pituitary axis is a powerful tool that regulates the entire hormonal balance of our body. The most important hormones in the human body, produced by the hypothalamus and pituitary gland:
- Oxytocin, vasopressin (ADH)
- Somatoliberin (GH-RH)
- Somatostatin (GH-IH)
- Corticoliberin (CRH)
- Thyroid hormone (TRH)
- Gonadoliberin (GnRH)
- Prolactoliberin (PRH)
- Prolactostatin (PIH)
As you can see, the hypothalamic-pituitary axis determines the functioning of the entire body through a huge number of hormones. The most important functions of hormones along this axis are presented below.
- Oxytocin
Oxytocin and vasopressin are two hormones of the hypothalamus that do not affect the pituitary gland. The role of the pituitary gland is only to store them. Once they receive the appropriate signal, they enter the bloodstream. Oxytocin is the hormone that plays the most important role during childbirth. It promotes contraction of the uterus. The second task of oxytocin is to facilitate lactation. The baby's sucking of the nipple stimulates the release of oxytocin into the mother's blood, which leads to the secretion of milk from the mammary glands.
- Vasopressin
Also known as antidiuretic hormone (ADH). It is a hormone that regulates the body's water balance. As the name suggests, antidiuretic hormone reduces urine output. Vasopressin is released when you become dehydrated, when your blood thickens, or when your blood pressure drops. By acting on the kidneys, vasopressin increases the density of diuresis. Thanks to this, you can save water and store it inside the body.
- Somatoliberin
This is the first example of a typical hormone of the hypothalamic-pituitary system. Produced in the hypothalamus, somatoliberin reaches the pituitary gland and stimulates its cells to secrete pituitary somatropin, also known as growth hormone. The somatotropin-somatotropin-releasing axis ensures the growth and development of all body tissues, which, in turn, determines the correctness of the growth process.
- Somatostatin
It is a hormonal opponent of somatoliberin. Its effect on the pituitary gland leads to a decrease in the release of growth hormone. In addition to its functions in the hypothalamic-pituitary axis, somatostatin is also produced locally in the gastrointestinal tract, where it inhibits, for example, the release of intestinal hormones.
- Corticoliberin
Known as corticotropin releasing hormone (ACTH). It is part of the hypothalamus-pituitary-adrenal system. Most active in stressful situations. The effect of ACTH on the adrenal cortex increases the release of one of the most important “stress hormones” - cortisol. The corticotropin-corticotropin-adrenal axis also regulates the metabolic balance of the entire body.
- Thyroid hormone
It is a hormone that causes the release of thyroid-stimulating hormone (TSH) from the pituitary gland. Thyrotropin levels are one of the markers indicating current thyroid function and are often measured in patients with thyroid disease. Thyrotropin stimulates the development of the thyroid gland and increases the secretion of its hormones. This in turn affects our heart rate, gastrointestinal function, nutrient metabolism and daily activities.
- GnRH
The role of GnRH in the hypothalamic-pituitary system is to stimulate the production of the so-called pituitary gonadotropin. These include: follicle-stimulating hormone (FSH) and lutropin (LH). GnRH is an example of a hormone secreted in a pulsatile rhythm, and the frequency of this rhythm is determined by the type of gonadotropin secreted. A low frequency of GnRH pulses causes the secretion of FSH, and a high frequency of LH (this occurs, for example, in women immediately before ovulation). Pituitary gonadotropins influence the ovaries of women and the testes of men, determining proper puberty and reproduction.
- Prolactoliberin
This is a hypothalamic hormone that stimulates pituitary cells to produce prolactin. Prolactin is the main factor that prepares the mammary glands for the process of lactation. The secretion of prolactin by the pituitary gland is a good example of a negative feedback mechanism in the hypothalamic-pituitary axis. During lactation, when prolactin levels in the body are highest, gonadotropin production is again suppressed. It is for this reason that breastfeeding women do not menstruate after childbirth.
- Prolactostatin
The hormone that inhibits prolactin release is generally not a typical hypothalamic statin. Its function is performed by the neurotransmitter dopamine. This is increased dopaminergic signaling in the hypothalamic-pituitary axis, which reduces the production of prolactin.
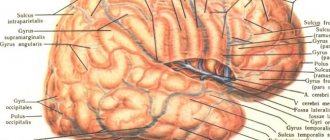
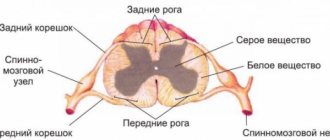
Pituitary hormones and the pituitary-adrenal system
The hypothalamic-pituitary system connects the endocrine system with the nervous system. It regulates the synthesis of hormones in the body that are necessary for the correct functioning of organs. Dysfunction of the hypothalamic-pituitary system leads to pathologies of internal organs and can even cause death. Why is the hypothalamic-pituitary system needed? The correct functioning of the entire body is impossible without the correct functioning of the nervous and endocrine systems. The nervous system, formed directly by neurons, neuroglia and connective tissue, permeates the entire body. Neurons conduct nerve impulses. Neuroglia surrounds nerve cells, protecting them and providing conditions for the transmission and formation of impulses, and also performs part of the metabolic processes of nerve cells. Connective tissue is essential for connecting parts of the nervous system. The central nervous system (CNS) is made up of the brain and spinal cord, and the peripheral nervous system is made up of the nerves and ganglia that lie beyond them. Even primitive animals, such as coral polyps, have a nervous system.
The endocrine system regulates the functioning of internal organs using hormones. Endocrine cells are present in most tissues of the body. The proper functioning of the endocrine glands gives the body the ability to adapt to environmental conditions, while simultaneously maintaining the coordinated functioning of the organs of the body itself.
The coordinated interaction of the nervous and endocrine systems is ensured by the hypothalamic-pituitary system, formed by the pituitary gland and the hypothalamic stalk. The pituitary gland is responsible for the production of hormones that regulate metabolism, tissue growth, and reproductive function. This is a small area, weighing less than a gram, located at the base of the brain and consisting of three lobes. The hypothalamus is located in the diencephalon and is connected to almost all parts of the central nervous system.
The list of its functions is extensive:
• Body thermoregulation; • Formation of an emotional response; • Formation of behavioral characteristics.
The hypothalamus connects the nervous system with the endocrine system through the pituitary gland. The hypothalamic-pituitary system is formed early, even in the first weeks of intrauterine development. Then the synthesis of hormones starts.
What are the substances responsible for?
Adrenocorticotropic hormone is responsible for the activity of the adrenal glands.
Getting into them with the bloodstream, the hormone stimulates the production of glucocorticoids - cortisol, cortisone and adrenocorticosterone. These hormones are actively used by the body to stimulate certain cells and glands. The mechanism of action of hormones is based on their binding to specific adrenergic receptors located in many tissues and blood vessels. As mentioned above, these hormones are “stress”, i.e. increase the activity of the body in the presence of danger or as a result of the action of any pathogenic factor.
These hormones have an active anti-inflammatory effect, which is why their synthetic derivatives have found use in medicine. In addition, there is a certain connection between adrenal hormones and ACTH: the substance increases the concentration of adrenal hormones, and their excess leads to the fact that ACTH (hormone) ceases to be produced. What kind of phenomenon this is and why this happens is still not known, but this paradox itself is called “feedback”.
Cortisol. The hormone is released in stressful situations, which causes blood flow to the muscles and heart. With this unique ability of the body to make muscles much stronger, the reaction is lightning fast, mental processes do not work, only the instinct of self-preservation.
Somatotropin, or growth hormone, is a growth hormone that regulates the development processes of the entire organism. This substance is produced in the anterior lobe of the pituitary gland. The synthesis of growth hormone is controlled by two main regulators: somatotropin-releasing factor (STGF) and somatostatin, which are produced by the hypothalamus.
Somatostatin and STHF activate the formation of somatotropin and determine the time and amount of its elimination. HGH is an anabolic hormone; the intensity of lipid, protein, carbohydrate and mineral metabolism depends on it. Somatotropin activates the biosynthesis of protein, glycogen, DNA, accelerates the mobilization of fats from the depot and the breakdown of fatty acids. STH is a hormone that has lactogenic activity. The biological effect of somatotropic hormone is impossible without the low molecular weight peptide somatomedin C. When GH is administered, “secondary” growth-stimulating factors—somatomedins—increase in the blood. The following somatomedins are distinguished: A1, A2, B and C. The latter has an insulin-like effect on fat, muscle and cartilage tissue.
Somatomedin-C (Insulin-like growth factor 1, IGF-1) is a polypeptide that functions as an endocrine mediator of somatotropic hormone (GH). The concentration of somatomedin-C in the blood depends on the level of the hormone GH: with an increase in the concentration of GH, the content of somatomedin-C increases. Somatomedin-C is synthesized mainly in the liver, less so in skeletal muscles. The stimulus for its production is an increase in the level of growth hormone in the blood, as well as food intake. In the blood, the hormonal mediator circulates bound to proteins.
The biological effects of somatomedin-C are similar to insulin, which is why it is called insulin-like factor 1 (there are 6 known insulin-like factors). It enhances the flow of glucose and amino acids into muscle and fat cells. IGF-1 affects the growth of the body in a similar way to growth hormone, stimulating the growth of bones in length.
Blood catecholamines: produced in the adrenal medulla in response to a strong physical or emotional stimulus. They improve the conduction of nerve impulses to the brain, are responsible for the body’s adaptation and response to stress, and activate the processes of breakdown of glycogen into glucose and breakdown of fats and proteins.
Catecholamines include:
• Adrenaline
It is considered the main hormone produced by the adrenal medulla. It is formed by synthesis from norepinephrine, after which it settles in chromaffin cells. The release of adrenaline into the blood most often occurs due to psychological and/or physical stress. At the same time, a person’s blood pressure rises sharply, blood flow in the coronary arteries increases, the heartbeat quickens, and the sugar level rises.
• Norepinephrine
It is a hormone and neurotransmitter that ensures the transmission of nerve impulses between neurons. It is formed as a result of the synthesis of dopamine in the cells of the sympathetic or central nervous system (93% of the hormone), the adrenal medulla (up to 7%). In terms of biological value, norepinephrine is comparable to adrenaline, but has a pronounced vasoconstrictor effect.
• Dopamine
It is the primary neurotransmitter of the central nervous system and the precursor of other catecholamines. A significant proportion of dopamine is produced by the central nervous system and only 2% by the adrenal glands. Dopamine is formed from L-tyrosine in neurons of the central nervous system and is part of the “reward system” of the brain (responsible for feelings of satisfaction or pleasure). A significant part of the dopamine entering the circulation is formed in the gastrointestinal tract; a significant amount of free dopamine excreted in the urine is formed in the kidneys.
Serotonin is produced in the brain and gastrointestinal tract. Serotonin molecules are formed from the amino acid tryptophan. Most of the neurotransmitter (90–95%) is synthesized in the intestine and only 5–10% in the pineal gland. A small proportion of the hormone is present in platelets and the central nervous system. Bright sunny color is very important for the production of serotonin. That is why on summer days your mood and well-being are always much better than in winter.
For a full life, the body must constantly have at least 10 mg of the neurotransmitter. Research has shown that serotonin, which is produced in the brain, is also used by it. The body’s need for the hormone of “happiness” is covered by a substance synthesized by the intestines.
Preparing for analysis:
• Given on an empty stomach; • Avoid fatty and heavy foods the day before.
Treatment and tests are ANONYMOUS!
Disorders of the hypothalamic-pituitary system: pathologies of increased hormone concentrations
Gigantism: Disorders of the Hypothalamic-Pituitary System
Although hormone levels in the hypothalamic-pituitary axis are mutually controlled, their regulatory mechanisms sometimes do not work. Disorders of the hypothalamic-pituitary system develop. As a result, a person deals with endocrine pathologies that arise as a result of an excess or deficiency of hypothalamic-pituitary hormones. Here are diseases that develop due to pathologies of increased concentrations of hormones of the hypothalamic-pituitary axis:
- Syndrome of inappropriate vasopressin production
An example of excessive activity of hypothalamic hormones is precisely the syndrome of inappropriate vasopressin production (SIADH). As a result of too high a concentration of this substance, there is increased water retention in the body and dilution of body fluids. SIADH syndrome mainly causes neurological symptoms, and in its advanced form can lead to cerebral edema.
- Hyperthyroidism or hyperfunction of the adrenal glands
Increased levels of hormones of the hypothalamic-pituitary system can lead to secondary hyperfunction of other endocrine glands - hyperthyroidism or adrenal hyperfunction. High concentrations of ACTH can cause so-called ACTH-dependent Cushing's syndrome. Secondary hyperthyroidism leads to the following conditions: increased heart rate, excessive weight loss, and diarrhea. Excessive psychomotor excitability also occurs.
- Gigantism or acromegaly
Often occurs against the background of these violations. And it happens to both men and women.
- Infertility
An increased concentration of prolactin, that is, hyperprolactinemia, is one of the most common hormonal causes of infertility. Prolactin suppresses the secretion of pituitary gonadotropins, which, in particular, leads to ovulation disorders.
- Pituitary adenomas
The most common cause of elevated pituitary hormone levels is pituitary adenomas, which escape the control of the hypothalamic-pituitary system and produce hormones independently of it. Their symptoms may result from elevated levels of one hormone or an overlapping excess of several types of hormones. Increased levels of peripheral hormones, such as cortisol or thyroid hormones, always require the exclusion of dysfunction of the hypothalamic-pituitary axis, which may be the cause of these disorders.
Hypothalamic-pituitary insufficiency
This pathology is characterized by a decrease in the level of hypothalamic hormones, leading to hypomenstrual and hypermenstrual (less commonly) syndrome - scanty or heavy menstruation.
In women with hypothalamic-pituitary insufficiency, the uterus is reduced, the cervix has a conical shape, the tubes are elongated, thin, tortuous, and the vagina is narrow. This pathological condition is called sexual infantilism. Such anatomical features of the genital organs play a certain role in the occurrence of infertility, but the absence of ovulation is of primary importance.
Treatment of endocrine infertility is carried out depending on the nature and location of the pathological process.
For hypothalamic-pituitary insufficiency and infantilism, hormone therapy is used. Treatment should be carried out strictly as prescribed by a gynecologist under regular monitoring of the amount of sex hormones (estrogen) in the blood and urine.
Disorders of the hypothalamic-pituitary system: decreased concentration of hormones
A disease with a mechanism opposite to the SIADH described above is diabetes insipidus. The cause of this disease is a deficiency of vasopressin produced in the hypothalamus, caused by dysfunction of hypothalamic cells. Such disorders of the hypothalamic-pituitary system are very common.
- Decreased vasopressin levels make urinary water loss uncontrollable.
- The amount of urine produced increases significantly, leading to symptoms of dehydration and a constant feeling of thirst.
A deficiency of pituitary hormones can cause symptoms of secondary endocrine gland insufficiency:
- Thyroid gland
- Adrenal glands
- Gonad
Worth knowing: Decreased gonadotropin levels can cause infertility and sexual dysfunction.
Deficiency of thyrotropin leads to secondary hypothyroidism, which manifests itself in the form of chronic fatigue, weight gain and constipation. Reduced levels of growth hormone have serious consequences, especially in children, delaying the growth process. On the other hand, prolactin deficiency can lead to lactation disorders. Hypopituitarism rarely manifests itself as a deficiency of a single hormone. More often, damage to this gland leads to a decrease in the production of several hormones. Pituitary dysfunction can have various causes. These include:
- Injuries
- Neoplasms infiltrating the pituitary gland
- Bleeding
- Congenital diseases (for example, hypoplasia, that is, underdevelopment of the pituitary gland)
When diagnosing a hormonal deficiency, you should always remember to check the functioning of the hypothalamic-pituitary axis (by measuring hormone levels of this axis). Thanks to this, it is possible to determine whether the deficiency of a particular hormone is the result of a violation of its peripheral production or a central violation of the hypothalamic-pituitary regulation.
Diagnosis of hypothalamic-pituitary dysfunction
To diagnose disorders in the hypothalamic-pituitary-ovarian system, a full range of clinical, laboratory, biochemical blood tests, hormone studies, and an X-ray of the skull (the area of the sella turcica where the pituitary gland is located) is necessary. Measuring basal temperature is informative. During the period of ovulation, there is an increase in rectal temperature by an average of 1 °C. If the luteal phase is insufficient, there is a shortening of the second phase of the cycle; the temperature difference in both phases of the cycle is less than 0.6 °C.
Ultrasound scanning of follicle growth and endometrial thickness is performed throughout the menstrual cycle.
An endometrial biopsy is performed 2–3 days before the onset of menstruation, which makes it possible to determine the functionality of the endometrium, and laparoscopy.
An informative method for studying the pituitary gland is computed tomography (CT). X-ray CT examination of the head allows us to identify changes in the density of the pituitary gland, differentiate micro- and macroadenomas, “empty” sella and cysts from normal pituitary tissue.
To diagnose neoplasms of the hypothalamic-pituitary region, MRI is used. A normal pituitary gland on MRI has the outline of an ellipse. MRI makes it possible to distinguish the pituitary stalk, the slightest changes in the structure of the pituitary gland, individual cysts, cystic tumors, hemorrhages, and cystic degeneration of the pituitary gland. The advantage of MRI is that it does not involve x-ray radiation, which makes it possible to repeatedly examine the patient over time.