Sections
Some patient stories are especially memorable. For example, this one.
At the time of his illness, Pyotr Ivanovich was 65 years old. All his life he worked as a carpenter, and recently he worked in our hospital. He repaired everything that was broken. A man with golden hands.
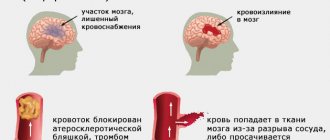
Like many people, he did not monitor his blood pressure, and suffered a stroke .
His left hand stopped working. For Pyotr Ivanovich it was a real disaster.
He couldn't do anything on his own: get dressed, take a shower, work with his hands.
Unfortunately, not all patients can regain the functionality of their arm, but in the case of Peter Ivanovich, rehabilitation could be very effective.
Rehabilitation after a stroke at the Almadeya Clinic
Almost every day patients come to us with the problem of increased muscle tone in the arm or leg after a stroke.
We carried out botulinum therapy, stretched the muscles, gave exercises and tasks to restore the arm.
The hand recovered best when Pyotr Ivanovich received his working tools and performed exercises with them. The nurses walked around and were amazed at how Pyotr Ivanovich easily copes with the repairs, although he is still undergoing a rehabilitation course.
We managed to restore his hand and Pyotr Ivanovich remained to work in the hospital.
This story shows that spasticity can be managed through movement and drug therapy. Using familiar activities can help restore activity to your sore arm.
Spasticity after stroke: features and rehabilitation
Not everyone experiences spasticity after a stroke. But, if a muscle is in spasm all the time, it can shorten. If the muscles of the injured arm or leg are not stretched, pain will begin over time. Contracture may develop - the muscle will shorten and the limb cannot be straightened without surgery.
How to avoid complications:
1. You should stretch muscles that have increased tone.
- You should stretch very carefully, slowly and gradually.
- The patient should not experience pain.
- Stretching is done several times a day, every day.
- Stretching can be done by the patient himself or by an assistant.
2. For spasticity, medications are used for treatment - botulinum therapy.
- It is very effective in reducing muscle tone and is safe.
- Botulinum therapy is successfully used in all countries with developed medicine.
- Botulinum therapy is carried out by additionally trained doctors. They give injections to those muscles that have high muscle tone.
- The effect does not occur immediately, but within several weeks, and lasts for an average of 3 months.
- If the patient's spasticity is severe, then botulinum therapy should be carried out 2-4 times a year.
- Botulinum therapy can be used to reduce tone, relieve pain and limited mobility. It can also help restore movement
These drugs are quite expensive, but they can be obtained free of charge through the state program if the patient has a disability group.
After 2 weeks of botulinum injections, the patient’s muscle tone decreases and a “rehabilitation window” opens.
At this time, rehabilitation will be very effective.
The secret is that the better the patient moves his arm or leg, the less muscle tone. You can get rid of spasticity through proper use of the affected arm for dressing, preparing and eating food, washing the body, and also when walking.
Therefore, in rehabilitation it is important to combine botulinum therapy with non-drug therapy:
- physical therapy
- classes with a speech therapist
- occupational therapist
- psychologist
- rehabilitation nurse
In some cases, after a series of botulinum injections and rehabilitation courses, the patient manages to get rid of spasticity completely.
Pyotr Ivanovich had just such a case. He managed to regain hand function using botulinum therapy and rehabilitation. Good interaction between specialists, doctors, psychologists, occupational therapists and physical therapists allows you not to waste time and effectively plan rehabilitation after botulinum therapy.
Write to us what difficulty you encountered, and we will suggest further steps for rehabilitation or provide the missing information.
Muscle spasticity and pain syndromes after stroke in a clinician’s practice
Stroke, being the main cause of deep and long-term disability of the population [7], poses serious medical and social challenges to society, and the provision of care to patients who have suffered a stroke needs further improvement and reorganization [1, 4].
Impaired motor functions are one of the main causes of disability in patients after a stroke. Movement disorders in post-stroke patients are often caused by increased muscle tone, which leads to impaired performance of simple movements, a decrease in the level of daily life activity and, accordingly, a violation of the quality of life [1, 3]. In addition, patients with spasticity have an increased risk of falls, and therefore fractures; they often experience contractures, limb deformities, pain syndromes, bedsores, dysfunction of the pelvic organs, etc. An increase in muscle tone occurs in 65% of patients after a stroke [ 1].
Spasticity is considered a movement disorder characterized by increased muscle resistance to passive stretch, which results from damage to the upper motor neurons and the corticospinal tract. Damage to the corticospinal tract and cerebral cortex often leads to flaccid paresis and paralysis with low muscle tone. At the same time, disruption of functional connections between the pyramidal and extrapyramidal systems often causes severe spasticity.
To prevent spasticity and to combat this complication of stroke, physical, physiotherapeutic and medicinal methods and means are used.
When carrying out exercise therapy in order to prevent spasticity or reduce increased muscle tone, it is advisable to use a facilitating technique based on the influence of sensitive stimuli on the main reflexes, which change against the background of structural damage to the brain.
Basic principles of this technique:
- taking into account the relationship between proprioceptive sensitivity and movement, on the one hand, and basic reflex activity, on the other;
- the use of various postures to facilitate reflex activity and, accordingly, movements;
- motor learning, which is based on repetition of movements and frequent stimulation;
- treatment of the body as a whole.
It is advisable to use the following concepts, of which the facilitative exercise therapy technique is an integral part: proprioceptive neuromuscular stimulation (PNF), Bobath concept, Brunnstrom concept and Feldenkrais system.
The PNF concept is based on the principles of body biomechanics and neurophysiology and can significantly improve the functional state of motor centers by enhancing the signal from proprioceptors that respond to stretching or compression, which are embedded in muscles, joints and ligaments.
It is based on the following principles and mechanisms:
- the use of complex movements, the basis of which is a combination of elements of rotation and diagonal motor patterns;
- stimulation of muscle activity through proprioceptive manual techniques and verbal and/or visual commands;
- extensive use of muscle synergy to maximize stimulation of weak muscle groups.
When conducting classes using the PNF method, the use of special manipulations is aimed at influencing proprioceptors, as a result of which it becomes possible to stimulate, initiate and facilitate various movements. These manipulations also help correct the direction, strength and volume of movement.
The use of the PNF technique leads to the formation and, which is extremely important, consolidation of movements at higher levels of the central nervous system, and this, in turn, contributes to the formation of new, correct, static and dynamic motor stereotypes and, accordingly, to an increase in the range of movements and an increase in the level of motor skills. activity.
The Bobath concept, like PNF, is neurophysiologically based and represents a holistic, complex therapy that is aimed at suppressing pathological movement patterns and stimulating the development of physiological movements. When conducting classes according to the Bobath concept, the processes of neuroplasticity are stimulated, which is accompanied by a facilitation of the movement of function from the affected areas of the brain to the intact ones.
The Bobath concept is based on three basic principles [6].
- Inhibition is the inhibition of pathological movements, body positions and reflexes that interfere with the development of normal movements.
- Facilitation is the simplification of the performance of correct, physiological movements, facilitating neuromuscular transmission.
- Stimulation using tactile and kinesthetic stimuli. Stimulation helps the patient develop the correct perception of physiological movements and normal body position in space.
The principles of therapeutic treatment used in therapy based on the Bobath concept:
- weight transfer;
- slow stretches directed from proximal to distal sections;
- choosing the optimal speed of movement in order to normalize muscle tone;
- correct positioning.
Let's consider the goals of rehabilitation for various patterns of post-stroke spasticity.
There are five main patterns of upper limb muscle spasticity.
Pattern I - adduction, internal rotation and retraction of the shoulder. The goals of rehabilitation are to maintain the patient's body in a sitting position, facilitate dressing, ensure hygiene of the armpit, normalize balance, improve gait symmetry, prevent or eliminate contractures in the elbow and wrist joints, and increase range of motion.
Pattern II - flexion at the elbow joint. Rehabilitation goals: increasing postural stability, eliminating flexion contractures, increasing the range of motion in the elbow joint, normalizing the function of extending the upper limb and returning it to its original position.
Pattern III - pronation of the forearm. The goals of rehabilitation treatment are: normalization of hand function and prevention of carpal tunnel syndromes.
Pattern IV - flexion of the wrist and clenched hand. Rehabilitation goals: ensuring palm hygiene, normalizing the function of grasping, holding and releasing objects.
Pattern V - flexion and adduction of the thumb towards the palm. Goal of therapy: normalization of the function of grasping objects.
There are also five main patterns of spasticity in the muscles of the lower limb.
Pattern I—spasticity of the hip adductors. Rehabilitation goals: improving hemiparetic gait, ensuring hygiene of the perineal area, facilitating bladder catheterization (if necessary), simplifying sexual contacts.
Pattern II - extension in the knee and/or hip joints, muscle spasms when trying to bend the leg in these joints. Rehabilitation goals: maintaining the patient’s body in a sitting position, reducing the load of one’s own body on a healthy lower limb, normalizing gait.
Pattern III - flexion in the knee joint, muscle spasms when trying to straighten the lower limb in the knee joint. Rehabilitation goals: maintaining the patient’s body in a sitting position, improving the patient’s verticalization process.
Pattern IV - plantar flexion and rotation of the foot. The goal of rehabilitation: correction of the position of the foot to provide the patient with the opportunity to “tear off” the heel from the floor.
Pattern V is plantar flexion of the toes and hyperextension of the big toe. The goal of rehabilitation is to facilitate the process of putting on shoes and other self-care skills.
Features of exercise therapy for post-stroke spasticity depend on the time elapsed after the stroke, as well as on the severity of muscle paresis and muscle tone.
In the first days after a stroke, passive movements and positional treatment are used.
Positional treatment is a set of measures aimed at ensuring that the patient is positioned correctly in bed, when the muscles potentially prone to increased tone are in a relaxed position as much as possible, and the attachment points of the antagonist muscles are in the closest possible position; in this case, the placement and fixation of the limbs should be short-lived.
Positioning of the upper limb: extension of the arm in the joints and abduction from the body at an angle of up to 30–40° with gradual movement up to 90°, the shoulder is rotated outward, the forearm is supinated, the fingers are straightened.
When positioning the lower limb, it is possible to give it a slightly bent position at the knee joint. When laying the leg straightened at the knee joint, a low cushion is placed under this joint; the foot should not rest against anything.
The duration of positioning treatment depends on the patient’s sensations. If there are complaints of discomfort and/or pain, the position of the patient’s limbs must be changed.
Fixation of the limbs can lead to a significant decrease in muscle tone; in such cases, after fixation, passive movements are carried out, gradually bringing their amplitude to the limits of physiological mobility in the joints.
Below is a diagram of an exercise therapy session for patients with severe hemiparesis who are in bed, which is due to the loss of the ability to move [5].
1. Exercises for a healthy upper limb:
- abduction and adduction of the arm;
- flexion and extension of the arm at the elbow joint;
- pronation and supination of the forearm;
- straight arm movements forward, to the side, up;
- rotational movements in the wrist joint.
Number of repetitions - 5 times.
2. Flexion and straightening of the affected upper limb at the elbow joint using the healthy arm (3–4 times).
3. A set of breathing exercises - slow inhalation and exhalation with raising and abducting the shoulders (4 minutes).
4. Exercises for a healthy lower limb:
- leg abduction;
- adduction of the leg and crossing with the affected leg;
- bending the leg at the knee joint;
- dorsiflexion of the foot;
- plantar flexion of the foot.
Number of repetitions - 5 times.
5. Alternately bringing together (as you exhale) and spreading (as you inhale) the shoulders (3-4 times).
6. Passive rhythmic, with increasing amplitude and range of motion in the joints of the hand of the affected upper limb (5 times).
7. Passive rhythmic, with increasing amplitude of movement in the joints of the foot of the affected lower limb (5 times).
8. Active rotation of the arms in the elbow joints inward and outward (the upper limbs are bent at the elbow joints), if necessary, providing assistance to the patient (up to 10 times).
9. Active rotation of the affected upper limb inward and outward, providing assistance to the patient if necessary (5 times).
10. A set of breathing exercises - slow inhalation and exhalation with raising and abducting the shoulders (4 minutes).
11. Active exercises for the hand and fingers with the forearm in a vertical position, providing assistance to the patient if necessary, especially during flexion (5 times).
12. Passive rhythmic, with increasing amplitude and range of motion in the joints of the affected limbs (5 times).
13. Active abduction and adduction of the hips when flexing the lower extremities in the joints, providing assistance to the patient if necessary (5 times).
14. A set of breathing exercises - slow inhalation and exhalation with raising and abducting the shoulders (4 minutes).
15. Active circular movements of the shoulder joints (5 times).
16. Reduction of the shoulder blades and extension of the back (starting position - lying on the stomach, the pelvis is constantly pressed) (3-4 times).
17. A set of breathing exercises - slow inhalation and exhalation with raising and abducting the shoulders (4 minutes).
18. Passive opposition of the thumb to the hand, spreading the fingers of the hand, grasping objects (5 times).
Below is a diagram of a physical therapy session for patients with hemiparesis who are able to move [5].
1. Starting position - sitting or standing. Elementary active exercises for unaffected muscle groups, performed by the patient without any difficulty (4 minutes).
2. Starting position - sitting or standing. Exercises:
- passive movements in the joints of the affected limbs;
- muscle relaxation using healthy limbs;
- rolling the foot and hand of the affected limbs on a roller.
Guidelines for paragraph 2:
- exercises should be carried out with warm hands;
- movements should be smooth;
- movements must be performed with a sufficiently large amplitude;
- Friendly movements should not be allowed.
Duration: 5 minutes.
3. Starting position - standing. Walking.
Guidelines for paragraph 3:
- if necessary, providing assistance to the patient and his insurance;
- using a pattern on the floor/carpet to make walking easier;
- control of foot placement;
- control of the patient's posture;
- correction of flexion friendly movements;
- walking both on a flat surface and overcoming certain obstacles.
Duration - up to 10 minutes.
4. Starting position - lying/sitting/standing. Active exercises for the affected limbs with a lighter starting position, alternating with exercises for the torso and breathing exercises.
Methodological recommendations for paragraph 4:
- if necessary, providing assistance to the patient;
- implementation of passive movements, light manual manipulation in order to ensure muscle relaxation and reduce muscle rigidity.
Duration - up to 10 minutes.
To reduce muscle tone and reduce muscle spasticity, the patient must also exercise independently. In doing so, he should receive the following recommendations:
- independent exercises should be used as part of comprehensive rehabilitation;
- an optimal choice of clothing is necessary - one that does not restrict movement;
- an optimal choice of shoes is required - comfortable and with non-slip soles (sneakers, high top sneakers);
- exercises must be performed at a slow pace;
- it is important to control breathing without holding or forcing it;
- If discomfort and/or pain occurs during exercise, it is necessary to temporarily suspend exercise therapy.
It should be noted some features of therapeutic exercises for spastic paresis:
- cessation of exercise if muscle tone increases during the exercise (if muscle tone becomes higher than the original);
- combined movements in two or more joints are used only after the patient has achieved full independent movements in each individual joint in order to prevent the occurrence of conjugate movements;
- the transition from a slight amplitude to a full range of movement should be made gradually as muscle strength increases;
- if the patient gets tired after performing several repetitions of one exercise, it is necessary to take a 3-5 minute pause in a sitting or lying position;
- exercise control of breathing (breathing should be smooth, breath holding and shortness of breath should be avoided);
- ensuring a sufficiently early transition from exercise therapy to occupational therapy with further simultaneous use of these rehabilitation methods.
In addition, it is important to give recommendations to the patient and his relatives regarding undesirable measures when muscle tone increases. These include [2]:
- raising the upper limb bent at the elbow and abducted;
- attaching a flat splint to the upper limb;
- exercises with dumbbells and other sports equipment with the affected hand;
- squeezing an expander and other objects in the hand if it is impossible for the patient to fully open the hand and fully spread the fingers;
- training the motor functions of the hand (grasping small objects);
- holding a walker/cane in the affected hand.
Pain syndromes that trouble patients after a stroke primarily include pain in the shoulder.
Shoulder pain. Factors contributing to the development of shoulder pain after a stroke:
- neurological and functional:
– reflex sympathetic dystrophy (shoulder-hand syndrome);– damage to the brachial plexus;
– low muscle tone, contributing to displacement and/or subluxation of the shoulder joint;
– weakness and spasticity in the muscles of the upper limb;
- orthopedic:
– rotational tears of the shoulder cuff due to non-compliance with the rules of positioning and moving the patient;– adhesive capsulitis;
– arthritis of the shoulder joint;
– biceps tendovaginitis;
– subdeltoid bursitis.
Prevention of pain in the shoulder joint includes the following measures:
- Careful handling of a paretic hand, which requires careful positioning of patients:
– when the patient is positioned on the affected side, move the scapula forward;
– with the patient positioned on the healthy side, support the paretic arm with a pillow;
– with the patient lying on his back, support the shoulder joint with a pillow;
- avoiding pressure on the paretic arm when transferring and lifting patients;
- early use of passive movements of the paretic arm within the physiological range of motion;
- conducting exercise therapy classes in combination with alternating exposure to heat and cold on the shoulder joint area;
- supporting devices:
– an armrest attached to a regular chair or wheelchair;
– a board made of transparent material attached to the armrests of the chair, through which the patient can see the position of his legs;
– bandages and cuffs for the shoulder and arm (advantages: supporting a weak arm, preventing subluxation of the shoulder joint; disadvantages: slowing down the recovery process, promoting the development of muscle spasticity);
- functional electrical stimulation of the affected upper limb;
- ultrasonic influence on the shoulder area.
CONCLUSION
Management of patients after a stroke with increased muscle tone and pain syndromes occupies an important place in the complex treatment of this category of patients and requires adherence to certain principles and rules.
Relieving pain and spasticity after a stroke is one of the most important conditions for increasing the effectiveness of rehabilitation, the degree of restoration of patients’ functions, the level of their social and everyday adaptation and, ultimately, improving the quality of life.