Damage to the abducens nerve of the eye is one of the ophthalmological pathologies that have much in common with neurological disorders. With this disease, the movements of the eyeball are distorted. It often happens that it does not move, especially when you need to look to the right. Let's tell you more about this disease and its treatment.
In this article
- Pathogenesis of the disease
- Causes of abducens neuropathy
- Symptoms of pathology
- Diagnosis of abducens neuropathy
- Treatment of abducens neuropathy
Pathogenesis of the disease
The abducens nerve of the eye is included in the category of fibers of the central nervous system. Its main function is to ensure the mobility of the visual organs. The nerve is responsible for the movements of the eyeballs, eyelids, dilation and constriction of the pupil. With neuropathy of the abducens nerve, a malfunction of the extraocular muscles occurs, and communication with the central nervous system of the body is disrupted. Thanks to the work of the abducens nerve, a person can look around without turning his head. Impaired functioning leads to ophthalmological pathologies, the most common of which is strabismus - strabismus.
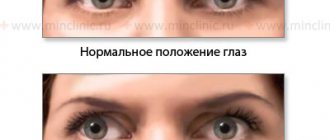
Lesions of the abducens nerve cause the eyeball to not move evenly in different directions. Problems arise when the pupil moves in the opposite direction from the bridge of the nose. The mobility of the rectus lateral muscle of the eye is impaired. This leads to the development of a converging form of heterotropia, as the intrinsic muscle “pulls” the eyeball towards itself. People who are faced with this problem suffer from dizziness, diplopia - double image, and lose orientation in space.
Strabismus is not the only problem that a person with abducens neuropathy may face. This pathology is especially dangerous in childhood. It often causes the development of amblyopia. This condition is often called "lazy eye." The disease occurs due to the fact that the organs of vision do not participate in the visual process at the same time. Against the background of neuropathy, paresis often develops - peripheral paralysis. This disease is included in the neurological group. It is characterized by damage to the facial nerve, impaired facial expressions, and disruptions in the production of tear fluid.
Why does abducens ophthalmic nerve paresis occur?
Paresis of the abducens ophthalmic nerve is a consequence of any disease in the head, central nervous system, or other organs and systems. Paresis of the abducens ophthalmic nerve can be caused by:
- infectious and inflammatory diseases of the brain (encephalitis, meningitis);
- infectious and inflammatory diseases such as syphilis, diphtheria, influenza, etc.;
- severe intoxication (alcohol, drugs, chemicals);
- botulism;
- stroke;
- heart attack in the head area;
- otolaryngological diseases;
- tumors in the brain;
- increased intracranial pressure;
- diabetes mellitus (in which the functioning and structure of blood vessels is disrupted);
- multiple sclerosis.
Causes of abducens neuropathy
The disease rarely develops on its own. It is usually a consequence of other diseases. Most often, neuropathy of the abducens nerve occurs against the background of pathologies of the cardiovascular system, after traumatic brain injury and neurosurgical operations. Much less often, the disease is congenital. Cases of a hereditary form of pathology are not excluded, but they are not so common in medical practice. Doctors consider the main causes of the development of abducens nerve neuropathy
- endocrine disorders (diabetes mellitus, hypothyroidism, hyperthyroidism);
- neurological pathologies (osteochondrosis of the cervical spine, multiple sclerosis, stroke);
- complications of infectious diseases (encephalitis, diphtheria, meningitis);
- intoxication of the body (poisoning with ethyl alcohol, chemicals, alcohol);
- chronic arterial pathologies (atherosclerosis, arteritis, phlebitis);
- cardiovascular diseases (varicose veins, arrhythmia, angina).
Doctors cannot always immediately determine what exactly caused the development of neuropathy of the abducens nerve of the eye. Diagnosis of this disease is often carried out by several specialists simultaneously, including: neurologists, cardiologists, endocrinologists, and traumatologists.
The disease is easier to detect in children than in adults. One of the causes of abducens neuropathy is hydrocephalus. This disease allows doctors to immediately carry out procedures that will allow them to diagnose the pathology.
How does oculomotor nerve palsy manifest?
The most negatively affecting the functioning of the visual organs is paresis of the oculomotor nerve. Symptoms of the disease will be pronounced and will allow the doctor to suspect this pathology. The oculomotor nerve performs a very important function in eye movement. It provides the work of the superior, inferior and medial rectus muscles, the inferior oblique muscle, and the muscle responsible for raising the upper eyelid. The oculomotor nerve innervates the sphincter of the pupil, ensuring its response to light (constriction and dilation). Therefore, if the oculomotor nerve is damaged, performing many eye movements becomes impossible.
Patients experience double vision, the pupil does not respond to light, ptosis develops, difficulty opening and closing the eye, and difficulty moving the eye.
Rarely, only the oculomotor nerve is affected. Usually the condition is accompanied by disruption of the abducens, trigeminal and lateral nerves. The pathology occurs against the background of diabetes mellitus, arterial hypertension, brain cancer, microinfarctions of the head vessels, and strokes.
Symptoms of pathology
The disorders that occur in the human body with this pathology affect various areas. The extent of optic nerve damage may also vary from patient to patient. Much depends on the immune system and the general condition of the body. Sometimes it happens that neuropathy affects the oculomotor nerve completely. In some cases, a partial disruption of its functions occurs. Therefore, it is very important for the doctor to analyze in detail the symptoms, which can be varied. The main signs of the disease include:
- drooping eyelid;
- pain in the eyes;
- immobility of the eyeball;
- decreased visual acuity;
- dilated pupils;
- diplopia.
A common consequence of abducens neuropathy is heterotropia. Typically, the patient develops convergent strabismus. More often this occurs in advanced forms of the pathology. Some people complain of high blood pressure, which is often due to problems with the brain. Headaches are another common symptom of this disease. It often happens that patients do not pay attention to the malaise and associate it with prolonged visual work.
Optic neuritis - symptoms and treatment
neuritis is an inflammation of the optic nerve. With the disease, vision sharply decreases, its field narrows and color perception is impaired. Spots and flickering appear before the eyes, pain occurs in the orbital area, which intensifies with eye movements [2].
Among all eye diseases, lesions of the optic nerve occur in 3.2% of cases [6].
The optic nerve is an atypical cranial nerve that contains approximately 1 million nerve fibers. It is the white matter of the brain located in the periphery. Its length is 35–55 mm [1]. Through it, visual information perceived by retinal cells is transmitted to the brain.
Nerve cell processes gather from throughout the retina to form the optic disc. Then they go to the brain, cross with the nerve fibers of the second eye and form the optic chiasm. The visual tract begins from it, which ends in the primary subcortical visual centers.
The optic nerve is divided into several parts:
- intraocular part and head of the optic nerve;
- retrobulbar part (behind the eye), or orbital;
- intratubular;
- intracranial.
The length of the intraocular part of the optic nerve is 25–35 mm. In the horizontal plane, the nerve bends in an S-shape, so that it is not stretched when the eyeball moves.
The intraocular part includes the optic disc. The optical fibers of the retina are connected in it, and vessels emerge from the center: narrow light red arteries and darker thick veins.
The retrobulbar or orbital part is a section of the optic nerve 25–35 mm long. It starts from the area where the nerve exits the eyeball and continues until it enters the optic canal.
The intracanalicular part of the optic nerve is enclosed in the optic canal. Its length is about 6 mm, the nerve here is fixed to the wall of the canal.
The intracranial part of the optic nerve passes into the optic chiasm. The length of this section is on average 10 mm. The intracranial region is particularly vulnerable to pathologies of adjacent structures, such as pituitary adenoma or aneurysm. With such disorders, the optic chiasm can be compressed, causing the visual field to narrow and the optic nerve to atrophy. If the optic nerve vessel is damaged, the patient ceases to see in one eye [2]. Hemianopsia, which is blindness in both eyes in half the visual field, also occurs.
With neuritis, the trunk and sheaths of the optic nerve in its various parts become inflamed. If the process extends to the optic nerve head, then such inflammation is called intraocular neuritis or papillitis . When the process occurs behind the eye, it is retrobulbar optic neuritis [3].
Causes of optic neuritis
It is not always possible to find out the exact cause of the disease, but most often inflammation of the optic nerve is caused by:
- multiple sclerosis is the most common cause of optic neuritis;
- other autoimmune diseases such as Sjogren's syndrome, systemic lupus erythematosus;
- Neuromyelitis optica is a demyelinating disease that primarily affects the eyes and spinal cord;
- demyelinating diseases associated with serum immunoglobulin G to myelin-oligodendrocyte glycoprotein (MOG-IgG) - for example, acute disseminated encephalomyelitis;
- granulomatous diseases - sarcoidosis, granulomatosis with polyangiitis[13];
- inflammatory diseases of the brain - encephalitis, arachnoiditis, meningitis, brain abscess, etc.;
- acute and chronic general infections - tuberculosis, Lyme disease, syphilis, brucellosis, typhus, erysipelas, influenza, smallpox, etc.;
- inflammatory diseases of the eyes and orbit;
- intoxication with lead or methyl alcohol; in children, helminthic intoxication is possible;
- penetrating wounds of the eye and orbit;
- traumatic brain injuries.
Diagnosis of abducens neuropathy
The level of development of medical technologies does not cause problems with the diagnosis of pathology. Abducens neuropathy does not occur overnight. Its development occurs gradually. Diagnosis of the disease is usually carried out not only by an ophthalmologist, but also by a neurologist. First of all, the doctor interviews the patient, collects a detailed history, and inquires about the presence of other diseases.
The first thing the doctor must do is to determine the cause of the neuropathy. Usually, an ophthalmoscopy is performed by an ophthalmologist for this purpose. This procedure allows you to analyze in detail the condition of the fundus. Ophthalmoscopy is performed to diagnose retinal breaks, identify thinned areas of the eye nerve, and analyze the condition of the fundus vessels. To carry out the procedure, oculists use an ophthalmoscope or fundus lenses.
If neuropathy of the abducens ophthalmic nerve is suspected, doctors often prescribe angiography of the ocular vessels to patients. Using a fluorescent dye and a special camera, the doctor takes a series of pictures called angiograms. They depict the vessels of the retina. Angiography allows you to identify pathologies of the optic nerve, a predisposition to blockage of blood vessels, and inflammatory processes occurring in the tissues of the eyeball.
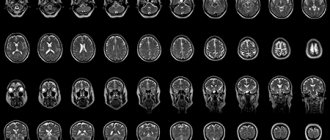
If the patient's condition is severe, doctors may recommend magnetic resonance imaging or computed tomography. This study allows you to obtain accurate data on the condition of the tissues and blood vessels of the eyeball. MRI and SCT diagnostics can be performed on adults and children. The list of contraindications to these procedures is quite small, which is why doctors often prescribe these studies to their patients.
Peripheral nervous system damage and tunnel syndromes
Peripheral nerve injury is one of the most common and complex injuries that occurs more often in young adults, while carpal tunnel syndromes are more common in relatively older ages. Peripheral nerve injury is not a life-threatening injury, although it can result in partial or total disability. Timely diagnosis and proper treatment are important to reduce the risk of developing diseases.
What is peripheral nervous system injury?
Damage to the peripheral nerve trunk can have various causes, for example, as a result of trauma caused by a blunt, sharp or piercing object, a firearm, or as a result of traction injury. Damage to the nerve trunk entails a violation of its integrity or partial damage, which leads to impaired function of the limbs (limited movement, impaired sensory function, pain and muscle wasting). To diagnose the peripheral nervous system, radiological and high-tech studies are used: electroneuromyography, echoscopy or magnetic resonance imaging (MRI) of the nerve.
New Hospitals uses a variety of methods to treat peripheral nerve injuries.
- Restoring nerve integrity
- Nerve neurolysis
- Endoneurolysis
What is carpal tunnel syndrome?
Tunnel syndrome is a disease of the peripheral nervous system caused by compression (squeezing, squeezing) of a nerve in anatomically narrow tunnels. The walls of the anatomical tunnel are represented by structures such as bones, tendons and muscles. Normally, peripheral nerves and blood vessels pass through the tunnels, but certain pathological changes cause the tunnel to narrow and put pressure on the nerve. Carpal tunnel syndromes can be caused by various conditions or injuries. For example, fractures of the bones of the limbs, injury to the ulna, prolonged sitting in one position (for example, when working with a computer), pregnancy, diabetes, etc. To diagnose carpal tunnel syndrome, X-ray studies are used, such as electroneuromyography, echoscopy or x-ray of the nerve.
There are different types of carpal tunnel syndrome:
Median nerve neuropathy (carpal tunnel syndrome) is characterized by a feeling of numbness in the middle of the first, second, third and fourth fingers, a sensation of electric shock, unbearable pain in the fingers that cannot be relieved by taking painkillers. Complaints with carpal tunnel syndrome are similar to complaints with cervical osteochondrosis.
Ulnar neuropathy (cubital tunnel syndrome) - characterized by numbness in the hand, some in the fourth and fifth fingers, weakness of the wrist and fourth and fifth fingers, difficulty extending the fourth and fifth fingers, muscle wasting between the thumb and index finger, cat's paw formation .
Radial neuropathy – one of the main clinical symptoms of radial neuropathy is a drooping hand. Drop hand is caused by paresis of the extensor muscles of the wrist and fingers. The patient cannot straighten his fingers and wrist.
Peroneal nerve neuropathy - at this time it is impossible to straighten the foot and toes (foot drop), sensory dysfunction occurs on the outer surface of the ankle and on the back of the foot.
Brachial plexus neuropathy - damage to the brachial plexus is one of the most complex and difficult to treat pathologies of the peripheral nervous system. The lesion may involve complete or incomplete disruption of nerve conduction. During this injury, loss of both motor and sensory function occurs throughout the entire limb due to blockade of nerve impulse conduction.
Tibial nerve neuropathy - Damage to the tibial nerve (neuropathy) causes paralysis of the flexor muscles of the foot and toes and the abductor muscles of the foot. With tibial nerve neuropathy, sensory dysfunction develops on the back surface of the ankle, foot, and dorsal surface of the toes.
New Hospitals uses various methods to treat carpal tunnel syndrome.
- Neurolysis or endoneurolysis of the nerve
- Nerve decompression in tunnel canals
- Nerve transposition
- Removal of the irritating factor (bone fragment, metal structure, after bone fixation)
What are benign and malignant peripheral nerve tumors?
Benign and malignant peripheral nerve sheath tumors, such as schwannoma, neurofibroma, malignant peripheral nerve sheath tumor, Barre-Masson tumor, develop from peripheral nerves without any impact. As for Morton's neuroma, it develops as a result of damage to the nerve of the foot. All tumors, both malignant and benign, can only be treated by removing the tumor. Tumors can be diagnosed using electroneuromyography, ultrasound, and magnetic resonance imaging (MRI) of the nerve.
Lesions of peripheral nerves can be either open or closed. Lesions can be caused by various injuries, such as wounds caused by a knife, glass shards or other sharp objects, bone fractures, soft tissue compression, etc. In the case of both open and closed nerve damage, its motor and sensory functions are impaired immediately after injury. Symptoms and complaints during these injuries correspond to the anatomical zone of innervation of the damaged nerve.
Peripheral nerve damage is accompanied by clinical signs—symptoms that may indicate damage:
Sensory impairment – sensory impairment accompanies nerve damage and anatomically corresponds to the zone of its innervation. This symptom appears immediately after injury and recovery is impossible without reconstruction of the nerve. Due to the lack of sensitivity, the main danger for such patients is frostbite, burns, etc.
Impaired motor function - when motor function is impaired, there is dysfunction of the muscles innervated by the damaged nerve. As a result, the patient finds it difficult to perform normal movements or cannot perform them at all.
Trophic disorders - damage to the peripheral nerve can lead to trophic disorders that reduce the elasticity and turgor of the skin, manifested in the form of thinning of the skin. The incidence of injuries and ulcers increases due to thinning of the skin. During this disorder, nail growth also slows down. The limbs become atrophic. Over time, trophic changes spread to the tendons, joint sac and ligaments, which leads to limited movement of the limbs and the development of contractures.
Damage to the radial nerve - one of the main clinical symptoms of damage to the radial nerve is a drooping hand. Drop hand is caused by paresis of the extensor muscles of the wrist and fingers. The patient cannot straighten his fingers and wrist.
Damage to the median nerve - when the median nerve is damaged, sensitivity develops on the palmar surface of the wrist, the first, second, third fingers and half of the fourth finger. Sensitivity is also impaired on the dorsal surface of the nail phalanges of the first, second and third fingers. Perception of the shape, size, consistency and temperature of an object when touched becomes difficult or impossible. In the early stages of the lesion, vasomotor, secretory, and trophic lesions are detected. The skin is dry, cyanotic, and easily damaged. The fingers are atrophied, the nails are deformed and brittle, their growth is slow compared to intact nails. The manifestation of clinical severity depends on the level of involvement.
Ulnar nerve damage - one of the main symptoms of ulnar nerve damage is impaired motor function in the wrist and fingers, accompanied by decreased sensitivity. It becomes impossible to straighten the fourth and fifth fingers and abduct the fifth finger. Strength in wrists and fingers weakens; approximately 1-2 months after the injury, muscle atrophy of the hand muscles is sharply felt; Muscle atrophy manifests itself especially quickly in the space between the first and second fingers. Due to the depletion of the interosseous and lumbrical muscles, bones are clearly visible on the dorsal surface of the hand. Later, the hand becomes deformed; when the hand is clenched into a fist, the fourth and fifth fingers do not reach the surface of the palm.
Treatment of abducens neuropathy
Treatment of pathology largely depends on the causes of its occurrence. The basis of treatment for this disease is strengthening the muscles of the eyeball. This allows you to activate blood flow. For this purpose, ophthalmologists prescribe eye drops, including:
- "Taufon";
- "Irifrin";
- "Emoxipin";
- "Vita-Yodurol";
- "Visiomax".
If pain occurs, doctors prescribe the following medications:
- "Tegretol";
- "Finlepsin";
- "Amelotex";
- "Dexalgin";
- "Baklosan";
- "Rekoksa";
- "Timonil."
These drugs have both an analgesic and anti-inflammatory effect, relieve muscle spasms, and reduce the excitability of nerve fibers. Any medications must be prescribed by a doctor. He will select a maintenance daily dose and frequency of administration.
Physiotherapy procedures, such as electrophoresis, have a good effect. To carry it out, doctors use the drug Neuromidin. It improves and stimulates impulse conduction in the nervous system. Treatment of neuropathy often includes wearing occlusive dressings and training glasses. In pediatric therapy, ophthalmologists often use stereo images, which they offer patients to view on a computer monitor.
It is very important to keep the muscles of the eyeball toned. To do this, doctors recommend that patients perform eye exercises. There are special complexes that are aimed at treating abducens nerve neuropathy. Most of them include exercises such as closing your eyes, alternate winking, and moving your eyes to the right side.
Cranial nerve palsy (CNP) is a rare complication of inadvertent dural puncture, with the sixth cranial nerve most commonly affected. Treatment usually involves infusion and alternating monocular occlusion. Results from epidural blood patch (EBP) remain controversial. In this case report, the authors describe the use of EBP early during CNP.A 40-year-old woman was admitted for surgical management of neurogenic bladder dysfunction. The epidural space was identified on the first attempt, and catheterization was performed. An epidural infusion of bupivacaine 0.0625% and fentanyl 2 μg/mL at a rate of 10 mL/hour was used for intraoperative analgesia for 4 hours of surgery. In the recovery room, the patient showed no signs of motor block; recovery occurred without any problems and the patient did not complain of pain. Six days after surgery, she complained of moderate frontal headache, discomfort with eye movements, and nausea. The headache was worse when the patient was in an upright position and better when she was in the supine position. On the 10th day after surgery, she noted diplopia. The diagnosis was post puncture headache (PDPH) with secondary cranial nerve palsy. EBP performed same day; 20 ml of autologous blood was injected into the epidural space at the T11-12 level. The patient immediately reported improvement in her diplopia. She remained in the supine position for 1 hour and complete headache relief was noted 2 hours after the procedure. The patient was discharged from the hospital on the 13th day after surgery and complete resolution of diplopia occurred 36 days after the inadvertent dural puncture.
Previous reports in the literature have shown that EBP performed >24 hours after symptom onset does not restore cranial nerve function even if the headache resolves. However, in our patient, blood filling within 24 hours from the onset of diplopia improved her well-being and led to complete regression of symptoms. Early treatment of cranial nerve palsy with EBP may be more successful than delayed blood patch, as it alleviates PDPH and provides partial improvement in diplopia.
Method for treating patients with lesions of the oculomotor nerves
The invention relates to medicine, namely to ophthalmology. Three round electrodes of different sizes are applied, the two smaller ones are placed on the skin of the orbital region and upper eyelids with the eyes closed. They are connected by a bifurcated wire to an electrode of a larger area, which is placed in the cervical-occipital region of the patient’s head. Electrophoresis of the affected areas is carried out with a 1.5% solution of Neuromidin using the oculo-occipital technique with the patient lying on his back. Current is applied to the electrodes until a slight tingling sensation is felt under the electrodes. Monitor the assigned current strength during the exposure time. The duration of the procedure is 15-20 minutes with a course of treatment of up to 15 daily sessions. The method allows local and targeted action on defective neuromuscular synapses of the eyeball, as well as the nuclear structures of the oculomotor nerves. 1 salary f-ly.
The invention relates to medicine, in particular to neurology, and can be used for targeted exposure to an electromagnetic field in the treatment of paralysis and paresis of the oculomotor muscles caused by lesions of the oculomotor nerves of various origins, mainly the oculomotor, abducens and trochlear nerves.
The overwhelming number of neurogenic lesions of the oculomotor striated muscles is caused either by a disorder of the conduction of nerve impulses along the axon of the corresponding neurons located in the brain stem, in the nuclei of the cranial nerves, in the cerebral peduncles and pons (usually infectious-allergic, vascular, traumatic lesions) or in the area neuromuscular junction (myasthenia gravis). In all these cases, there will be a deficiency of acetylcholine in the neuromuscular synapse of the oculomotor muscles, as a result of which there is no contraction of one or another striated muscle of the eye with the development of local or total ophthalmoplegia or ophthalmoparesis.
There is a known method of treating patients using pulsed low-frequency physiotherapy, which gives an analgesic, setative and anti-inflammatory effect and has a positive effect on general hemodynamics, neurohemodynamics and microcirculation, in which a targeted effect of a low-frequency electromagnetic field and local electrical stimulation with a pulsed current are carried out (Zaslavsky A.Yu., Markarov G.S. Pulse low-frequency therapeutic device IN-FITA, Journal of Medical Technology, No. 5, 1994, p. 39).
A significant drawback of this method is that the restoration of the patient’s functions impaired as a result of the disease occurs extremely slowly or does not occur at all.
There is also a known method of treating diseases of the central nervous system (cerebral arachnoiditis, cerebral atherosclerosis), which consists of administering medicinal substances (in particular, iodine) using the oculo-occipital technique (Bogolyubov V.M. Resortology and physiotherapy, vol. 1, Moscow: Medicine. 1985, p. 312. Ulashchik BC Galvanization and electrophoresis of medicinal substances).
However, this method is not used for the treatment of oculomotor disorders.
The closest known in its technical essence and the achieved result is the method of treating patients with lesions of the oculomotor nerves, mainly caused by vascular or inflammatory lesions of the brain stem, chosen as a prototype, in which a targeted effect of an electromagnetic field and local electrical stimulation with a pulsed current are carried out (see, for example, description of the invention to the RF patent No. 2146909, class A61F 9/00, published 03.27.2000).
The disadvantage of this method is its comparative ineffectiveness due to the duration of the therapeutic effect, especially in the treatment of partial atrophy of the optic nerve.
The technical result of the use of the invention is to provide an optimal combination of the drug Neuromidin (which has two important properties for the treatment of neurogenic muscle disorders - blockade of acetylcholinesterase, leading through an increase in acetylcholinesterase to increased transmission of the nerve impulse at the synapse to the eye muscle and the ability to enhance the release of potassium from the cell (while in sodium enters the cell, which leads to an additional increase in muscle contraction.
In addition, the introduction of neuromidin using the oculo-occipital technique allows local and targeted action on defective neuromuscular synapses of the muscles of the eyeball.
In addition, under the influence of electric current, neuromidin molecules move to the brain stem, where they have a stimulating effect on the nuclear structures of the oculomotor cranial nerves.
All ego contributes to increasing the efficiency and increasing the intensity of impulses passing through the axons of the cranial oculomotor nerves in the muscle of the eyeball and restoring their functions impaired as a result of the disease.
This technical result is achieved by the fact that in the method of treating patients with lesions of the oculomotor nerves, mainly caused by vascular or inflammatory lesions of the brain stem, in which three round electrodes of different sizes are applied, the two smaller ones are placed on the skin of the orbital region and the upper eyelids with closed eyes and connect a forked wire with an electrode of a larger area, which is located in the cervical-occipital region of the patient's head, and electrophoresis of the affected areas is carried out with a 1.5% solution of Neuromidin according to the oculo-occipital technique with the patient lying on his back, while current is applied to the electrodes up to a slight tingling sensation under the electrodes and control of the prescribed current strength during the exposure time with a procedure duration of 15-20 minutes with a course of treatment of up to 15 daily sessions.
In addition, after the procedure is completed and the electrodes are removed, the patient is lightly adapted with his eyes closed for 10 minutes.
The declared set of essential features is in a direct cause-and-effect relationship with the achieved result.
Comparison of the claimed technical solution with the prototype made it possible to establish its compliance with the “novelty” criterion, because it is not known from the prior art.
The proposed method is industrially applicable using existing technical means and meets the criterion of “inventive step”, because it does not clearly follow from the prior art, while the latter does not reveal any transformations characterized by essential features different from the prototype, aimed at achieving the specified technical result.
Thus, the proposed technical solution complies with the established conditions for patentability of the invention.
The applicant has not found any other known technical solutions of a similar purpose with similar essential features.
The proposed method is carried out as follows.
Stages of the proposed method of treating patients with lesions of the oculomotor nerves caused by vascular or inflammatory lesions of the brain stem, taking into account the proposed modification of electrophoresis with a 1.5% solution of Neuromidin using the oculo-occipital technique (with the patient lying on his back) and local electrical stimulation with pulsed current through the use of electrophoresis of the affected areas of the oculomotor nerves, is carried out as follows.
1. Place gauze pads moistened with a 1.5% solution of neuromidin, which has anticholinesterase properties and the ability to block the inhibitory substance potassium, under two round electrodes with a diameter of 5-6 cm2, and inject directly into the central and peripheral structures affected by the disease oculomotor nerves.
2. The electrodes are placed on the skin of the orbital region and upper eyelids of both closed eyes and in the cervical-occipital region of the patient’s head, while the bifurcated wire is connected at one end to two round electrodes with a diameter of 5-6 cm2, located on the closed eyes, and at the other to the electrode with an area of 30-50 cm2, located in the cervical-occipital region of the patient’s head.
3. Turn on the “Potok” (RF) apparatus and carry out galvanization and local electrical stimulation with pulsed current using the oculo-occipital technique (with the patient lying on his back) through the use of electrophoresis of the affected areas of the oculomotor nerves, for which the current strength is set from 1 to 3 mA in depending on the individual sensations of the Nazi to the sensation of a slight tingling sensation under the electrodes, and physiological monitoring of the patient’s condition is carried out during the entire duration of exposure. If necessary, after 10 minutes the current strength is adjusted to the initially prescribed level.
4. After the procedure is completed and the electrodes are removed, the patient is lightly adapted with his eyes closed, for which, to improve light adaptation, the patient remains lying with his eyes closed for 10 minutes.
The proposed method is illustrated by the following examples.
Example 1. Patient K., 42 years old, driver. After suffering a neuroinfection in August 2004, diplopia of the right abducens nerve (convergent strabismus) manifested itself, making it impossible to perform professional duties. A computed tomography scan performed three weeks later revealed a cyst in the posterior cranial fossa. Outpatient treatment (galantamine, piracetam, ketarol, diuretics) did not improve the patient's condition. After admission to the clinic of nervous diseases at the Moscow State Medical University (2nd neurological department of the city clinical hospital No. 50 in Moscow), 15 sessions of neuromidin electrophoresis were performed using the oculo-occipital technique (with the patient lying on his back). After the sixth procedure, the severity of convergent strabismus on the right decreased significantly; by the end of the course of treatment, diplopia ceased, and insufficiency of the external rectus muscle of the right eye was determined only in special tests. The patient was discharged home in satisfactory condition on maintenance oral doses of Neuromidin (40 mg) per day and subsequently returned to his previous work. Follow-up: six months later - no complaints.
Example 2. Patient K., 65 years old, was taken by ambulance to the 1st neurological department of the city clinical hospital No. 50 in Moscow, in December 2005, for several tens of minutes without loss of consciousness against the background of increased numbers blood pressure, ataxia and diplopia developed. Static and dynamic ataxia, more pronounced in the arms (especially in the right), mild pyramidal deficit in both legs (in the Barre position, paresis up to 4 points in the left leg), in the form of hyperreflexia and bilateral Babinski's symptom. Bilateral ptosis, external ophthalmoplegia on the right, slight voluntary movements medially are possible with the left eye, during which nystagmoid twitching occurs. Voluntary raising of the eyelids of both eyes is impossible. With passive lifting of the eyelids, there is bilateral divergent strabismus, more on the right, with diplopia and dizziness occurring. Magnetic nuclear tomography, performed three days after the disease, revealed signs of ischemic infarction in the basal parts of the medullary pons, mainly on the right. Conventional methods of treating acute cerebral ischemic stroke (antihypoxants, neuroprotectors, vascular drugs) reduced the severity of paresis in the left leg and ataxia, but had no effect on oculomotor disorders. After stable normalization of blood pressure, two weeks after admission to the hospital, treatment was started according to the proposed method with neuromidin electrophoresis using the oculo-occipital technique (with the patient lying on his back). At the fifth session, the patient was able to independently raise his eyelids and hold them for a minute. In this case, there was minimal diplopia and slight divergent strabismus on both sides. After the tenth session, voluntary holding of the eyelids increased to 10 minutes (with a compensatory position of the head), and divergent strabismus and diplopia practically did not bother the patient. The patient was discharged in satisfactory condition on maintenance doses of oral neuromidin. Follow-up: eight months later - the condition is satisfactory, he keeps his eyes open throughout the day (if tired, he takes breaks by closing his eyes).
Example 3. Patient G., 49 years old, was admitted to the neurological department No. 2 of the city clinical hospital No. 50 in Moscow with complaints of diplopia when looking down, which appeared two weeks before admission to the clinic after suffering an acute respiratory illness with high fever. Outpatient treatment (antibiotics, non-steroidal anti-inflammatory drugs, anitcholinesterase drugs, diuretics) were ineffective. Computed X-ray tomography revealed no changes in the brain substance or its membranes. The neurological status revealed bilateral paresis of the trochlear nerves (more on the right), absence of abdominal reflexes, high knee and Achilles reflexes. Based on clinical signs, the disease was regarded as brainstem arachnoencephalitis with bilateral paresis of the oculomotor (abducens) nerves. After the third session of treatment with neuromidin electrophoresis using the oculo-occipital method (with the patient lying on his back), according to the proposed method, slight downward movements of the eyeballs appeared; after the fifth session, such movements increased significantly, diplopia decreased, which stopped after the fifteenth session against the background of almost complete recovery downward movements of the eyeballs. At the same time, abdominal reflexes began to be evoked. Knee and Achilles reflexes normalized. The patient was discharged in satisfactory condition. Follow-up: six months later - no complaints.
This method does not require highly qualified medical personnel. Thus, the proposed method increases the effectiveness of therapeutic effects and confirms the clinical effectiveness of use in the treatment of paresis and paralysis of the oculomotor nerves that develop after vascular and inflammatory lesions of the brain stem.
1. A method of treating patients with lesions of the oculomotor nerves, mainly caused by vascular or inflammatory lesions of the brain stem, in which three round electrodes of different sizes are applied, the two smaller ones are placed on the skin of the orbital region and upper eyelids with the eyes closed and connected with a forked wire to an electrode of a larger area, which is placed in the cervical-occipital region of the patient's head and electrophoresis of the affected areas is carried out with a 1.5% solution of Neuromidin using the oculo-occipital technique with the patient lying on his back, while current is applied to the electrodes until a slight tingling sensation is felt under the electrodes and control of the prescribed current strength during the exposure time, duration of the procedure is 15-20 minutes with a course of treatment of up to 15 daily sessions.
2. The method according to claim 1, characterized in that after the procedure is completed and the electrodes are removed, the patient is lightly adapted with his eyes closed for 10 minutes.