What pathologies can develop?
As a rule, symptoms depend on which segment of the organ is affected by disease or injury, as well as on what type of pathology develops. Signs of brain dysfunction include:
- impaired innervation of the legs and arms or other areas of the body;
- severe pain syndrome in the spinal region;
- unauthorized bowel movement;
- psychosomatic disorders;
- impaired mobility of the torso;
- severe muscle or joint pain;
- muscle atrophy.
The following diseases may be accompanied by similar symptoms:
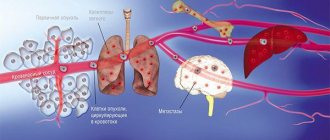
- Tumor. This includes both malignant and benign neoplasms, which can be located extradurally, intradurally, or intramedullarily. Extradural tumor is characterized by rapid progression and is localized in hard tissues. An intradural neoplasm develops under hard tissues. Intramedullary neoplasms are characterized by their development in a liquid substance.
- Intervertebral hernia. The initial stage of hernia development is protrusion. When the fibrous ring of the disc is destroyed, the contents exit into the spinal canal. If the spinal cord was involved in the lesion, the development of myelopathy (not compression or chronic) is diagnosed.
- Chronic myelopathy. Often (with untimely treatment) osteochondrosis becomes the cause of the development of spondylosis, which is the final degenerative change in the structure of tissues. In this case, the appearance of osteophytes is observed, which subsequently serve to compress the brain canal.
- Heart attack. Caused by impaired circulation of the organ, the occurrence of necrotic processes and is characterized by the formation of blood clots and dissection of the aorta. It is recommended to immediately contact a specialist if pain occurs in this department. This is the only way to prevent irreversible consequences.
Anatomical features
A rather thick tourniquet, white in color, located in the spinal canal - this is the human spinal cord. Its diameter is about 1-1.5 cm, and its length almost reaches half a meter (up to 45 cm). This organ weighs about 38 g.
- Reflexes
- Interesting Facts
- Reflex Bow
- Segmental structure
- What are the segments?
- Role and functions in the body
- Gray matter of the spinal cord
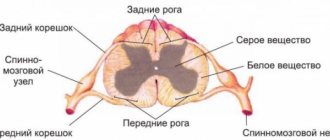
The narrow spinal canal is not only the location of an important organ, but also its protection. The core of the organ consists of a gray substance
It is covered by a white substance, which is also covered with protective and nourishing shells for the core. This is the general plan of the structure of the spinal cord.
Topography
The structure and functions of the spinal cord are quite complex. Neurosurgeon students study it in detail. Experts very carefully consider the development of the spinal cord. Ordinary people are interested in the question of what its topography is and familiarity with the leading role of this organ.
So, it is quite simple to describe the essence and goals that this body serves. The cervical spinal cord at the level of the back of the head in the area of the foramen passes into the cerebellum. The spinal cord ends at the level of the first 2 lumbar vertebrae. The conus spinal cord is located where a pair of vertebrae are located in the lumbar region. Next is the well-known “terminal thread”.
But this fragment is considered atrophied. It is called the “end” region. Nerve endings called “roots” are distributed along the entire circumference of the thread. The filum terminale is equipped with a substance containing a small proportion of nervous system tissue. But the outer part is not even equipped with a similar fabric.
The topography of the organ includes a pair of thickenings where the innervating processes emerge (cervical thickening of the spinal cord and lumbar). The outer and rear surfaces of the bundle are separated by slits called “middle”. The one in front is deeper, the back one is smoothed.
External structure
The general structure of the spinal cord suggests its division into a number of surfaces: posterior, anterior and two lateral. The spinal cord has faint grooves on the lateral surface. They are located longitudinally, and nerves extend from the grooves. They are also called “roots”. In the lumbar area, together with the terminal filament, they form a tail, which is commonly called a horse's tail. The grooves divide half of this cord into the following structures:
- front;
- lateral;
- posterior (cords).
The grooves of the spinal cord extend along the canal. The roots are divided into anterior ones - they are formed by efferent neurons, and posterior ones, created by afferent neurons. Their bodies converge into a knot. The roots unite and form a nerve. So, on all sides of the tourniquet there are over 30 nerve endings, forming exactly the same number of pairs. This is the external structure of the spinal cord.
White matter
All cords are made entirely of white matter of the spinal cord. They consist of longitudinal nerve fibers. These threads converge, forming peculiar conductors. Based on their functional purpose, fibers are divided into 3 types:
- motor;
- associative;
- sensitive.
The first are represented by short bundles and combine all parts into a single system. The second ones are called ascending. They give signals to the centers. Still others are descending. They provide signals from central structures to areas of the horns.
Important Mania. delusions of persecution, delusions of grandeur, hypochondria. causes, symptoms, diagnosis of mental disorder and treatment
Gray matter
It structurally resembles grouped longitudinal plates consisting of homogeneous neurons. It contains not only neuronal bodies, but also neuropil, glial cells and capillaries. Along the entire spine it forms 2 columnar types, left and right. They are connected by gray adhesions.
The anterior horns contain the largest neurons. They form the motor nuclei of the spinal cord and inhibitory neurons. The structure of the gray matter of the background horns is not the same. It contains a huge number of intercalary type neurons.
The lateral horns of the spinal cord fill the centers of the ANS, the dilation of the pupil, the bases of innervation of the digestive system and other important organs of the human body. In the nucleus of the gray matter of the spinal cord there is a canal that neurosurgeons call “central.” It is filled with liquor. In adults, in some places it is filled with cerebrospinal fluid, and in others it is overgrown.
Shells
Anatomy of the spinal cord describes the membranes of the spinal cord:
- vascular soft;
- hard;
- avascular or arachnoid.
The characteristics of shell 1 are as follows: soft, penetrated by vessels and nerves. It is enveloped by the avascular part. There is some space here called “subarachnoid”. The cerebrospinal fluid generated in one of the systems flows into this niche. The last shell is made up of connective tissue; it is strong and flexible. The membranes of the spinal cord and brain are identical and form a single structure.
Copy of the Encyclopedia = Copy of the encyclopedia Translate: Englisch ↔ Russian Library = LibraryLATERAL HORNS OF THE GRAY SUBSTANCE OF THE SPINAL CORD
[lateral horns of the spinal cord]
The lateral horn, cornu laterale, is an anatomical structure of the gray matter of the spinal cord. In a cross-section of the spinal cord, the columns of gray matter on each side have the appearance of horns. There is a wider anterior horn, cornu ventrale (anterius), a narrower posterior horn, cornu dorsale (posterius) and a lateral horn, cornu laterale. The anterior and posterior horns correspond to the anterior and posterior columns of the spinal cord. The lateral horn corresponds to the lateral intermediate column (autonomous) of gray matter, located between the anterior and posterior horns. Throughout the VIII cervical to II lumbar segment, the gray matter of the spinal cord has a protrusion - the lateral horn. In the medial part of the base of the lateral horn, the thoracic nucleus (Clark's nucleus), nucleus thoracicus, consisting of large nerve cells, is noticeable, well outlined by a layer of white matter. This nucleus extends along the entire posterior column of gray matter in the form of a cellular cord. I. Clarke, Jacob Augustus Lockhart Clarke, 1817-1880, British physician, physiologist, histologist. This nucleus reaches its greatest diameter at the level from the XI thoracic to the I lumbar segment. The lateral horns contain the nerve centers of the sympathetic part of the autonomic nervous system in the form of several groups of small neurons united in the lateral intermediate (gray) substance, substdntia (grisea) intermedia lateralis. The axons of these neurons pass through the anterior horn and exit the spinal cord as part of the ventral roots. In the intermediate zone there is a central intermediate (gray) substance, substantia (grisea) intermedia centralis. The processes of the neurons of this nucleus participate in the formation of the spinocerebellar tract. At the level of the cervical segments of the spinal cord, between the anterior and posterior horns, and at the level of the upper thoracic segments, between the lateral and posterior horns, in the white matter adjacent to the gray matter, there is a reticular formation, formatio reticularis. The reticular formation here looks like thin bars of gray matter intersecting in different directions and consists of nerve cells with a large number of processes. See: spinal cord: anatomy, spinal cord: histology.
See: Neurology: Dictionary, Neurology: Internet Resources.
| LIBRARY = LIBRARY Human Physiology = Human Physiology, Human Anatomy = Human Anatomy, Human Biochemistry = Human Biochemistry, Human Psychology = Human Psychology, Medicine = Medicine, Mathematics = Mathematics, Chemistry = Chemistry, Physics = Physics, General Scientific Literature = General Science Lexis. Click here to access any source in the site's library! Click here and receive access to the any reference of the library! “I AM LEARNED. . . N E D O U C H A ?” T E S T V A S H E G O I N T E L L E C T A Premise : The effectiveness of the development of any branch of knowledge is determined by the degree of compliance with the methodology of knowledge - the knowable entity. |
Error? Click here and fix it! Search on the site E-mail of the author (author)
Reflexes
The functional diversity of neurons in spinal structures creates conditions for reflex activity, both with the participation of its own elements and central ones - the cortex and subcortical centers.
Each such reflex arc necessarily contains the following links:
- afferent – perceives impulses;
- intercalary – connects sensory and motor neurons;
- efferent - transmits the impulse to the immediate performer.
Among the motor reflexes, attention should be paid to myotatic ones, which are aimed at stretching/contracting muscles, as well as skin ones - plantar and abdominal. With their help, every person can perform voluntary and involuntary movements.
In addition to motor reflexes, there are other reflexes. Thus, autonomic ones are usually divided into sympathetic and parasympathetic. Their common task is to control and ensure the constancy of the internal environment of the body to maintain human life.
Interesting Facts
This organ has not yet been fully studied - it still hides many secrets from doctors, and their solution in the future may lead to the cure of currently incurable diseases of the nervous system. Here are some interesting facts about this organ:
- If the spine grows over 20 years, then the spinal cord only grows for 5 years.
- Stress leads to a serious decrease in the number of neurons. If the normal number of neurons is 13-14 million, then as a result of stress their number drops by half - this is especially true for pregnant women.
- In the process of evolution of vertebrate organisms, the spinal cord appeared first, and only then the brain. The first performed all the simplest functions, including reflex ones.
- Some living beings are able to live after losing their brain, remaining only with their spinal cord.
- Damage to a specific area of the organ not only causes loss of sensation below the rupture site, but also the ability to sweat. This forces people with injuries to spend more time in the shadows, as the body has partially lost its thermoregulatory function, which is extremely important for life.
- Scientists have not yet come to a general conclusion, and cannot establish the mechanism of hair loss throughout the body in people with spinal cord injuries.
- If the thoracic organ has been affected, the person may lose the ability to cough.
- A biopsy and analysis of the white matter of an organ can detect hundreds and thousands of human diseases.
- The spinal cord very sensitively senses the rhythm of music, and therefore is automatically able to send signals that will make the body move to the rhythm.
- People with a healthy spine are much more active in their sexual life.
The organ is located in the spinal canal, and its length is no more than 45 cm, which is less than the length of the spine itself. This is due to the fact that the brain grows only until the age of five, and the spine, as a rule, until the end of puberty.
This organ controls absolutely all motor processes in the body, including contraction of the heart muscles, breathing and movement of the limbs.
We study the anatomy of the spinal cord:
Location of the spinal cord and its functions:
Thus, the loss of certain functions, for example, leg movements, makes it possible to determine which part was damaged. Injuries to this organ are among the most serious, and the damage is often irreparable. The main thing is to monitor the health of your spine and not overload it unless absolutely necessary.
Related article: How we are made
Reflex Bow
Reflex = stereotypical response
Important Convulex and Convulex retard (100, 300, 500 mg)
There are afferent fibers that transmit their excitation directly to the motor neurons of the anterior horn cells, which in turn control the muscles through their efferents. This reaction occurs at the level of the spinal cord and is called a simple reflex. The underlying neural circuit is called a reflex arc. The afferent may pass directly to the motor neuron (monosynaptic reflex arc) or involve interneurons (multisynaptic reflex arc) that reach the motor anterior horn cells.
Self-reflex
In self-reflex, the receptor and effector are located in the same organ. The reflex arc proceeds monosynaptically.
Example:
Patellar tendon reflex = PSR
The patellar tendon reflex is a monosynaptic reflex.
A blow to the patellar tendon causes the hamstring muscles to contract. The receptors that sense the stimulus are stretch receptors in the muscle spindle of the quadriceps femoris muscle. Sensory afferents travel to the dorsal horn of the spinal cord and are transmitted to the anterior horn motor neurons at the L2-L4 level by only one synapse. The effects now travel through the lumbar plexus and are then isolated in the femoral nerve back into the muscle and cause it to contract.
What is important for the clinical assessment of a reflex is not the strength of the response to a stimulus, but the fact that the reflex can be evoked on both sides.
External reflex
In an external reflex, the receptor and effector are not located in the same organ. Several synapses are inserted into the reflex arc.
Examples:
polysynaptic flexor reflex
The flexion reflex is a protective reflex. Nociceptors are stimulated, and the excitation spreads to various levels of the spinal cord. The flexors on the irritated side and the extensors on the opposite side contract.
- Cremaster reflex
- Abdominal cutaneous reflex
- Eyelid reflex
Structure of the lateral horn
The structure of the anterior horn
The anterior horn consists of large motor root neurons, which form two groups of nuclei - medial and lateral. The medial nuclei stretch along the entire length of the spinal cord, innervating the muscles of the trunk, neck and proximal parts of the limbs. The lateral group of nuclei is present in the areas of thickening and innervates the limbs. The largest number of nuclei is contained in the anterior horns of the cervical thickening of the spinal cord, from where the upper limbs are innervated, which is determined by the participation of the latter in human labor activity. The latter, due to the complication of the movements of the hand as an organ of labor, has significantly more of these nuclei than in animals, including anthropoids.
Between the anterior and posterior horns of the gray matter of the spinal cord there is an intermediate zone. That part of it that surrounds the central canal forms the middle intermediate substance. The neurons of this substance participate in the formation of the anterior spinal tract, and the rest is called the lateral intermediate substance. It includes the lateral horns, and consists of the roots of autonomic neurons, the axons of which exit the spinal cord as part of the ventral roots of the spinal nerves and go to the autonomic ganglia.
Structure of the lateral horn
The lateral horns project only in the thoracolumbar spinal cord and contain sympathetic neurons. Here lie the medial and lateral intermediate nuclei.
Parasympathetic neurons are located below, reaching the V sacral segment. They also form an intermediate nucleus. Its fibers go to the pelvic internal organs.
The gray matter of the spinal cord directly passes into the gray matter of the brain stem, and part of it spreads along the rhomboid fossa and the walls of the aqueduct, and part of it is divided into separate nuclei of cranial nerves or nuclei of bundles of pathways.
The gray matter of the spinal cord consists mainly of nerve and glial cell bodies. The non-identity of their number at different levels of the spinal cord causes variability in the volume and configuration of gray matter. In the cervical region of the spinal cord, the anterior horns are wide; in the thoracic region, the gray matter on a cross section becomes similar to the letter “H”; in the lumbosacral region, the size of both the anterior and posterior horns is especially significant. The gray matter of the spinal cord is fragmented into segments. A segment is a fragment of the spinal cord, anatomically and functionally connected to one pair of spinal nerves. The anterior, posterior and lateral horns can be considered as fragments of vertically located columns - anterior, posterior and lateral, separated from each other by the spinal cord cords consisting of white matter.
The following circumstance plays an important role in the implementation of reflex activity of the spinal cord: almost all axons of the cells of the spinal ganglia entering the spinal cord as part of the dorsal roots have branches - collaterals. Collaterals of sensory fibers contact directly with peripheral motor neurons located in the anterior horns, or with interneurons, the axons of which also reach the same motor cells. Collaterals of axons extending from the cells of the intervertebral ganglia not only reach the corresponding peripheral motor neurons located in the anterior horns of the nearest segments of the spinal cord, but also penetrate into its neighboring segments, forming the so-called spinal-spinal intersegmental connections, ensuring the irradiation of excitation that comes into the spinal cord after irritation of the receptors of deep and superficial sensitivity located on the periphery. This explains the widespread reflex motor reaction in response to local irritation. This kind of phenomenon is especially typical when the inhibitory influence of pyramidal and extrapyramidal structures on peripheral motor neurons that are part of the segmental apparatus of the spinal cord decreases.
The nerve cells that make up the gray matter of the spinal cord can be divided into the following groups according to their function:
1. Sensory cells (T cells of the dorsal horns of the spinal cord) are the bodies of the second neurons of the sensory pathways. Most of the axons of the second neurons of the sensory pathways as part of the white commissure pass to the opposite side, where they participate in the formation of the lateral cords of the spinal cord, forming in them the ascending spinothalamic tracts and the anterior spinocerebellar tract of Govers. The axons of the second neurons that do not pass to the opposite side are directed to the homolateral lateral cord and form the posterior spinocerebellar tract of Flexig in it.
2. Associative (intercalary) cells related to the spinal cord proper apparatus participate in the formation of its segments. Their axons end in the gray matter of the same or closely located spinal segments.
3. Vegetative cells are located in the lateral horns of the spinal cord at the level of C8-L2 segments (sympathetic cells) and in segments S3-S5 (parasympathetic cells). Their axons leave the spinal cord as part of the anterior roots.
4. Motor cells (peripheral motor neurons) make up the anterior horns of the spinal cord. A large number of nerve impulses coming from various parts of the brain along numerous descending pyramidal and extrapyramidal pathways converge to them. In addition, nerve impulses come to them along the collaterals of the axons of pseudounipolar cells, the bodies of which are located in the spinal ganglia, as well as through the collaterals of the axons of sensory cells of the dorsal horns and associative neurons of the same or other segments of the spinal cord, carrying information mainly from deep sensitivity receptors, and along the axons located in the anterior horns of the spinal cord, Renshaw cells, which send impulses that reduce the level of excitation of alpha motor neurons and, therefore, reduce the tension of the striated muscles.
The cells of the anterior horns of the spinal cord serve as a site for the integration of excitatory and inhibitory impulses coming from various sources. The addition of the excitatory and inhibitory biopotentials arriving at the motor neuron determines its total bioelectric charge and, in connection with this, the features of the functional state.
Among the peripheral motor neurons located in the anterior horns of the spinal cord, two types of cells are distinguished: a) alpha motor neurons - large motor cells, the axons of which have a thick myelin sheath (A-alpha fibers) and end in the muscle with end plates; they provide the degree of tension of the extrafusal muscle fibers that make up the bulk of the striated muscles; b) gamma motor neurons - small motor cells, the axons of which have a thin myelin sheath (A-gamma fibers) and, therefore, a lower speed of nerve impulses. Gamma motor neurons make up approximately 30% of all cells in the anterior horn of the spinal cord; their axons are directed to the intrafusal muscle fibers that are part of the proprio receptors - muscle spindles.
The muscle spindle consists of several thin intrafusal muscle fibers enclosed in a fusiform connective tissue capsule. The axons of gamma motor neurons end on the intrafusal fibers, affecting the degree of their tension. Stretching or contraction of intrafusal fibers leads to changes in the shape of the muscle spindle and irritation of the spiral fiber surrounding the equator of the spindle. In this fiber, which is the beginning of the dendrite of a pseudounipolar cell, a nerve impulse arises, which is directed to the body of this cell, located in the spinal ganglion, and then along the axon of the same cell to the corresponding segment of the spinal cord. The terminal branches of this axon directly or through interneurons reach the alpha motor neuron, exerting an excitatory or inhibitory effect on it.
Thus, with the participation of gamma cells and their fibers, a gamma loop is created, which ensures the maintenance of muscle tone and the fixed position of a certain part of the body or the contraction of the corresponding muscles. In addition, the gamma loop ensures the transformation of the reflex arc into a reflex ring and takes part in the formation, in particular, of tendon or myotatic reflexes.
Motor neurons in the anterior horns of the spinal cord form groups, each of which innervates muscles that share a common function. Along the length of the spinal cord there are anterior internal groups of cells of the anterior horns, which provide the function of muscles that influence the position of the spinal column, and anterior external groups of peripheral motor neurons, on which the function of the remaining muscles of the neck and torso depends. In the segments of the spinal cord that provide innervation to the limbs, there are additional groups of cells located mainly behind and outside the already mentioned cellular associations. These additional groups of cells are the main cause of cervical (at the level of C5-Th2 segments) and lumbar (at the level of L2-S2 segments) thickenings of the spinal cord. They provide mainly innervation to the muscles of the upper and lower extremities.
The motor unit of the neuromotor apparatus consists of a neuron, its axon and the group of muscle fibers innervated by it. The sum of peripheral motor neurons participating in the innervation of one muscle is known as its motor pool, while the bodies of motor neurons of one motor pool can be located in several adjacent segments of the spinal cord. The possibility of damage to part of the motor units that are part of the muscle pool is the cause of partial damage to the muscle innervated by it, as happens, for example, with epidemic poliomyelitis. Widespread damage to peripheral motor neurons is characteristic of spinal amyotrophies, which are hereditary forms of neuromuscular pathology.
Among other diseases in which the gray matter in the spinal cord is selectively affected, syringomyelia should be noted. Syringomyelia is characterized by expansion of the usually reduced central canal of the spinal cord and the formation of gliosis in its segments, while the dorsal horns are more often affected, and then a dissociated type of sensitivity disorder occurs in the corresponding dermatomes. If degenerative changes also extend to the anterior and lateral horns, manifestations of peripheral muscle paresis and vegetative-trophic disorders are possible in the body metameres of the same name as the affected segments of the spinal cord.
In cases of hematomyelia (bleeding in the spinal cord), usually resulting from spinal cord injury, the symptoms are similar to syringomyelitic syndrome. The lesion in traumatic hemorrhage in the spinal cord is predominantly of the gray matter due to the peculiarities of its blood supply.
Gray matter is also the site of predominant formation of intramedullary tumors growing from its glial elements. At the onset of the tumor, symptoms may manifest as damage to certain segments of the spinal cord, but subsequently the medial sections of the adjacent cords of the spinal cord are involved in the process. At this stage of intramedullary tumor growth, conduction-type sensory disturbances appear slightly below the level of its localization, which subsequently gradually descend downwards. Over time, at the level of the intramedullary tumor, a clinical picture of damage to the entire diameter of the spinal cord may develop.
Signs of combined damage to peripheral motor neurons and corticospinal pathways are characteristic of amyotrophic lateral sclerosis (ALS syndrome). In the clinical picture, various combinations of manifestations of peripheral and central paresis or paralysis arise. In such cases, as more and more peripheral motor neurons die, the symptoms of already developed central paralysis are replaced by manifestations of peripheral paralysis, which over time increasingly dominate the clinical picture of the disease.
Ticket No. 7: “Describe the connections of the piriform neurons of the cerebellar cortex.” - see ticket No. 2.
Ticket No. 8: “Give structural and functional characteristics of the granular and agranular types of the cerebral cortex.”
The cerebellar cortex has a large surface area - when extended, its area is 17x20 cm.
The human cerebellar cortex is represented by three layers: the granular layer (deepest), the Purkinje cell layer and the molecular layer (superficial)
The molecular layer on fresh sections is dotted with small dots (which is where its name comes from). It contains three types of neurons - basket cells, stellate cells and Lugaro cells. The direction of the axons of Lugaro cells is unknown; the axons of basket cells end on the body (soma), and the axons of stellate cells end on the dendrites of Purkinje cells.
Stellate and basket cells of the molecular layer are inhibitory interneurons with endings on Purkinje cells. The projections of basket neurons to Purkinje cells are oriented at right angles to the long axis of the cerebellar layers. These axons are called transverse fibers. The middle layer is formed by Purkinje cells, the number of which in humans is 15 million. These are large neurons, their dendrites branch widely in the molecular layer. The axons of Purkinje cells descend to the cerebellar nuclei, and a small number of them terminate on the vestibular nuclei. These are the only axons that exit the cerebellum. The organization of the cerebellar cortex is usually considered in relation to the Purkinje cells that form its output.
The lower layer of the cerebellar cortex is called granular because it has a granular appearance in sections. This layer is made up of small granule cells (about 1,000-10,000 million), the axons of which go into the molecular layer. There, the axons divide in a T-shape, sending a branch (parallel fiber) 1-2 mm long in each direction along the surface of the cortex. These branches pass through the dendritic branching areas of other types of cerebellar neurons and form synapses on them. The granular layer also contains larger Golgi cells, the dendrites of which extend over relatively long distances in the molecular layer, and the axons go to the granule cells.
The granular layer is adjacent to the white matter of the cerebellum and contains a large number of interneurons (including Golgi cells and granule cells) about half of all neurons in the brain. Mossy fibers form excitatory synaptic endings in the cerebellar cortex on the dendrites of granule cells (granular cells). Many similar fibers converge on each granular cell. Synaptic endings are collected in the so-called cerebellar glomeruli (glomeruli). They receive inhibitory projections from Golgi cells.
The granule cell axons ascend through the Purkinje cell layer to the molecular layer, where they each divide into two parallel fibers. The latter run along the long axis of the leaf and end with excitatory synapses on the dendrites of Purkinje and Golgi cells, as well as on the interneurons of the molecular layer - stellate cells and basket cells. Each parallel fiber makes synaptic contacts with approximately 50 Purkinje cells, and each Purkinje cell receives connections from approximately 200,000 parallel fibers.
The cerebellar cortex contains two types of motor fibers. Climbing fibers pass through the granular layer and end in the molecular layer on the dendrites of Purkinje cells. The processes of liana-like fibers entwine the dendrites of these cells like ivy branches. Each Purkinje cell receives only one fiber, while each liana fiber innervates 10 to 15 Purkinje neurons. All other afferent pathways of the cerebellum are represented by much more numerous (about 50 million) mossy fibers ending on grain cells. Each mossy fiber gives off many collaterals, due to which one such fiber innervates many cells of the cerebellar cortex. At the same time, numerous parallel fibers from granule cells approach each cell of the cortex, and therefore hundreds of mossy fibers converge through these neurons on any cell of the cerebellar cortex.
Segmental structure
A segment of the spinal cord is a piece of a tourniquet along with associated nerves. There is no morphological separation of one segment of the spinal cord from another. It is extremely functional. Each of the segments innervates a certain region. The designation of spinal cord segments is represented by alphanumeric indices, oriented to a part of the spinal cord and containing segment numbers.
The spinal cord consists of about 33 segments. The spinal cord segments have 4 roots, a pair of anterior and posterior. The spinal column is significantly longer than the cord, so it should be remembered that the segments are not numbered in the same way as the vertebrae. Any nerve consists of motor-sensitive roots. They come out in bunches from this bundle to the openings between the vertebrae.
The nerve ending located behind forms a ganglion and merges with the nerve ending in front. In this case, a mixed nerve is formed, which is divided into branches:
- The meningeal branch innervates in accordance with the nature of the spinal cord membrane and the canal wall.
- Dorsal - the skin in the corresponding areas, as well as deep muscle tissue.
- The connective tissue branch is the connecting link between the tourniquet and the ganglia.
- The abdominal branch is responsible for innervation of the limbs, lateral surfaces of the body and tissue of the abdominal part of the body.
What are the segments?
The sections of the spinal cord differ from those used to conventionally divide the areas of the spine. Their length varies; the fewest elements are found in the coccygeal part. The segments are connected to certain areas in the body by nerve conductors. In general, the brain is divided into the following segments:
- Neck – 8.
- Chest – 12.
- Sacral – 5.
- Lumbar – 5.
The main length falls on the thoracic segments of the spinal cord, after which 23.2% is allocated to the neck and only 7.3% to the lower back. They are posterior and anterior nerve roots that alternate regularly. They are located above the vertebrae with the same number. Their main task is to report movements and be responsible for muscle contractions. Therefore, the anterior nerve roots are also called motor, and the posterior - sensitive.
The intervertebral foramen contains the roots of each individual segment. Their direction is not the same, because the spinal column is filled with the brain. In the cervical region they lie horizontally, in the thoracic region they are directed diagonally, and in the lower part they are almost vertical.
The shortest segments are the neck segments, and the longest ones are in the lower back and sacrum. In the lower part they form the so-called “horse tail” - this is a bunch of roots located below the 2nd vertebra.
A visual representation of what a spinal cord segment looks like in cross section
Anatomy of the spinal cord
see Structure of the spinal cord
The spinal cord is located in the spinal canal and in an adult it is a cord 40-45 cm long and weighing 30-40 g. The spinal cord contains more than 13 million nerve cells. The spinal cord is covered by three layers of membranes. The outer layer is represented by hard, middle - arachnoid and inner - soft shells. In the space between the middle and inner membranes there is cerebrospinal fluid.
The upper end of the spinal cord corresponds to the first cervical vertebra and connects to the lower part of the brain - the medulla oblongata, and the lower end, at the level of 1-2 lumbar vertebrae, ends in a cone-shaped formation. Below this place it continues in the form of a terminal filament; in the upper part of this filament there are nerve cells, and its end reaches the coccygeal spine.
If you make a cross-section of the spinal cord, you will see that it consists of two different substances: the outer one is white and the inner one is gray (Fig. 61). Gray matter consists of nerve cells, and white matter consists of nerve fibers that connect nerve cells in different segments of the spinal cord with each other and with nerve cells in the brain. These nerve fibers perform the function of conducting impulses to each other from the spinal and nerve centers of the brain.
Spinal cord segments
The spinal cord consists of 31-33 segments: 8 of them are cervical, 12 - thoracic, 5 - lumbar, 5 - sacral and 1-3 coccygeal segments.
Nerve centers (groups of nerve cells) located in each segment of the spinal cord provide sensitivity and movement of tissues and organs of certain parts of the body (Fig. 63.)
Cervical segments of the spinal cord
Nerve centers located in the cervical segment of the spinal cord provide sensory and motor functions of the skin and muscles, starting from the head to the 5th rib of the chest, the outer surface of the arms, palms and fingers.
Thoracic segments of the spinal cord
Nerve centers located in the thoracic segment of the spinal cord provide sensitive and motor functions of the skin and muscles, starting from the 5th rib of the chest to the bladder and the inner surface of the arms.
Lumbar segments of the spinal cord
Nerve centers located in the lumbar segment of the spinal cord provide sensory and motor functions to tissues and organs in the area, starting from the bladder area to the anterior surface of the legs and toes.
When nerve cells located in any segment of the spinal cord and their processes are damaged, the sensitive and motor functions of tissues and organs that receive innervation from this segment are disrupted - paralysis of these tissues or muscles occurs.
Role and functions in the body
Functionally, the spinal cord performs the following tasks:
- Regulating the functioning of organs and systems through the transmission of nerve impulses to them. In other words, it performs a reflex function.
- Transmission of information to the brain, as well as from it to motor neurons.
The gray matter of this spinal segment contains many pathways that provide motor reactions of the body. The activity of each reflex occurs through a special department of the central nervous system - the nerve center. In the latter, special cells are localized, which occupy a certain section of the organ and ensure the functionality of specific systems in the body. For example, knee reflexes are provided by nerve cells localized in the lumbar region of the spine. The urination process is in the sacrum, dilation of the pupils is in the thoracic.
Important How to take tenoten for adults?
The nervous center processes information sent by skin receptors, as well as other systems and organs in the body. As a response, the brain generates certain impulses, which are subsequently transmitted to the executive organs (for example, skeletal muscles, vascular apparatus, cardiac muscles, etc.). As a result, a change in the functional state of the latter occurs.
Motor neurons carry out the process of contraction of muscles in such parts of the body as limbs, intercostal spaces, etc. Regulation of such a reflex also occurs with the help of higher parts of the central nervous system. Nerve impulses that travel along the spinal cord to the brain transmit information about the dysfunction of any organ or system in the body. Impulses transmitted by various organs to the spinal cord and from there to the region of the dorsal roots of the brain are processed by sensory neurons. From them, information is distributed either to the dorsal horns or to the cerebral hemispheres.
Physiology of the spinal cord
The spinal cord consists of 31-33 segments: 8 cervical, 12 thoracic, 5 lumbar, 5 sacral and 1-3 coccygeal.
A segment is a section of the spinal cord associated with one pair of anterior and a pair of dorsal roots.
The posterior (dorsal) roots of the spinal cord are formed by the central processes of afferent sensory neurons. The bodies of these neurons are localized in the spinal and cranial nerve nodes (ganglia). The anterior (ventral) roots are formed by axons of efferent neurons.
According to the Bell-Magendie law , the anterior roots are efferent - motor or autonomic, and the posterior roots are afferent sensitive.
gray matter is isolated on a cross section of the spinal cord.
, which is formed by a cluster of nerve cells.
It is bordered by white matter
, which is formed by nerve fibers.
The nerve fibers of the white matter form the dorsal (posterior), lateral and ventral (anterior) cords of the spinal cord
, which include the conductive tracts of the spinal cord. In the posterior cords there are ascending cords, in the anterior cords there are descending ones, and in the lateral cords there are both ascending and descending pathways.
In the gray matter, dorsal (posterior) and ventral (anterior) horns
. In addition, there are lateral horns in the thoracic, lumbar and sacral segments.
All gray matter neurons can be divided into three main groups:
1) interneurons located mainly in the dorsal horns of the spinal cord,
2) efferent motor neurons localized in the anterior horns,
3) efferent preganglionic neurons of the autonomic nervous system, located in the lateral and anterior horns of the spinal cord.
A segment of the spinal cord, together with the innervated areas of the body, is called a metamer . A group of muscles innervated by one segment of the spinal cord is called a myotome . The area of skin from which sensory signals travel to a specific segment of the spinal cord is called a dermatome .
There are three main functions of the spinal cord:
1) reflex,
2) trophic,
3) conductor.
The reflex function of the spinal cord can be segmental
and
intersegmental
.
The reflex segmental function of the spinal cord consists in the direct regulatory influence of the efferent neurons of the spinal cord on the effectors innervated by it when irritating the receptors of a certain dermatome.
Reflexes whose arc switches in the spinal cord are called spinal . The simplest spinal reflexes include tendon reflexes , which provide contraction of skeletal muscles when their proprioceptors are irritated due to rapid short-term stretching of the muscle (for example, when a tendon is struck with a neurological hammer). Spinal tendon reflexes are clinically important because... each of them closes in certain segments of the spinal cord. Therefore, by the nature of the reflex reaction one can judge the functional state of the corresponding segments of the spinal cord.
Depending on the location of the receptors and the nerve center in humans, elbow, knee and Achilles tendon spinal reflexes are distinguished.
The ulnar flexion reflex occurs when the biceps brachii tendon is struck (in the area of the cubital fossa) and manifests itself in flexion of the arm at the elbow joint. The nerve center of this reflex is localized in the 5-6 cervical segments of the spinal cord.
The ulnar extensor reflex occurs when the triceps brachii tendon is struck (in the area of the cubital fossa) and manifests itself in the extension of the arm at the elbow joint. The nerve center of this reflex is localized in the 7-8 cervical segments of the spinal cord.
The knee reflex occurs when the quadriceps tendon is struck below the kneecap and is manifested in the extension of the leg at the knee joint. The nerve center of this reflex is localized in the 2-4 lumbar segments of the spinal cord.
The Achilles reflex occurs when the heel tendon is struck and manifests itself in flexion of the foot at the ankle joint. The nerve center of this reflex is localized in 1-2 sacral segments of the spinal cord.
There are two types of fibers in skeletal muscle: extrafusal
and
intrafusal
, which are connected in parallel.
Intrafusal muscle fibers perform a sensory function. They consist of a connective tissue capsule
in which proprioceptors are located, and
peripheral contractile elements
.
A sharp, quick blow to the muscle tendon leads to its tension. As a result, the connective tissue capsule of the intrafusal fiber is stretched and proprioceptors are irritated. Therefore, pulsed electrical activity of motor neurons localized in the anterior horns of the spinal cord occurs. The discharge activity of these neurons is the direct cause of the rapid contraction of extrafusal muscle fibers.
Diagram of the reflex arc of the spinal tendon reflex
1) intrafusal muscle fiber, 2) proprioceptor, 3) afferent sensory neuron, 4) spinal cord motor neuron, 5) extrafusal muscle fibers.
The total time of the spinal tendon reflex is short, because its reflex arc is monosynaptic. It includes rapidly adapting receptors, phasic a-motoneurons, and FF and FR type motor units.
The reflex intersegmental function of the spinal cord consists in the implementation of intersegmental integration of spinal reflexes, which is provided by intraspinal pathways connecting different segments of the spinal cord.
The trophic function of the spinal cord is reduced to the regulation of metabolism and provision of nutrition to those organs and tissues that are innervated by the neurons of the spinal cord. It is associated with the non-pulse activity of neurons capable of synthesizing many trophotropic biologically active substances. These substances slowly move into the nerve endings, from where they are released into the surrounding tissue.
The conductive function of the spinal cord is to provide bilateral connections between the spinal cord and the brain. It is provided by its ascending and descending pathways - groups of nerve fibers.
There are three main groups of ascending pathways:
1) Goll and Burdakh,
2) spinothalamic,
3) spinocerebellar.
The Gaulle and Burdach pathways are conductors of skin-mechanical sensitivity from tactile receptors and proprioceptors to the sensory zones of the posterior central gyrus of the cerebral cortex. The Gaulle pathway carries information from the lower part of the body, and the Burdach pathway carries information from the upper body.
The spinothalamic tract is a conductor of tactile, temperature and pain sensitivity. This pathway ensures the transmission of information about the quality of the stimulus to the posterior central gyrus.
The spinocerebellar tracts carry information from tactile receptors, as well as proprioceptors of muscles, tendons and joints to the cerebellar cortex.
Descending pathways form a pyramidal
and
extrapyramidal
systems.
The pyramidal system includes the pyramidal corticospinal tract
.
It is formed by the axons of large pyramidal neurons ( Betz cells
), which are located in the motor zone of the precentral gyrus of the cerebral cortex.
In humans, the pyramidal tract has a direct triggering activating effect on spinal motor neurons innervating the flexor (flexor) muscles of the distal limbs. Thanks to this tract, voluntary conscious regulation of precise phasic movements is ensured.
The extrapyramidal system includes:
1) rubrospinal tract,
2) reticulospinal tract,
3) vestibulospinal tracts.
The rubrospinal tract is formed by axons of neurons in the red nucleus of the midbrain, activating spinal flexor motor neurons. The reticulospinal tract is formed by the axons of neurons of the reticular formation of the hindbrain, which have both an activating and an inhibitory effect on flexor motor neurons. The vestibulospinal tracts are formed by the axons of the neurons of the vestibular nuclei of Deiters, Schwalbe and Bekhterev, which are located in the hindbrain. These pathways have an activating effect on spinal extensor motor neurons.
An animal in which the spinal cord is separated from the brain is called spinal
.
Immediately after damage or separation of the spinal cord from the brain, spinal shock - the body’s reaction, which manifests itself in a sharp drop in excitability and inhibition of reflex activity or areflexia.
The main mechanisms of spinal shock (according to Sherrington) are:
1) elimination of descending activating influences entering the spinal cord from the upper parts of the central nervous system,
2) activation of intraspinal inhibitory processes.
There are two main factors that determine the severity and duration of spinal shock:
1) level of organization of the body (in a frog, spinal shock lasts 1-2 minutes, and in humans it lasts months and years),
2) level of spinal cord damage (the higher the level of damage, the more severe and prolonged the spinal shock).