general information
It happens that a completely healthy newborn baby begins to cry for no apparent reason, refuse to eat, have trouble falling asleep or sleep restlessly at night. Or older children complain of severe headaches , which may be accompanied by bouts of vomiting against the background of a general loss of strength. In such cases, doctors often diagnose increased intracranial pressure (hereinafter referred to as ICP).
What is ICP and what are its symptoms? What could be the causes and consequences of this ailment for a person’s health and well-being? We will answer this and many other questions on the topic in this material. But first, let's look at some general questions that relate to the physiology and structure of the human brain.
Concept of cranial pressure
What happens to the pressure in the cranium of a healthy person, how does a deviation from the norm manifest itself? You need to understand these issues, because an increase or decrease in such pressure is an alarming sign. Symptoms of the pathology vary, which makes diagnosis more difficult, but treatment depends only on the cause of the disease.
The human brain is immersed in a special fluid called cerebrospinal fluid (CSF). In the brain itself there are peculiar cavity formations - ventricles, which can communicate with each other. The choroid plexus of the ventricles produces cerebrospinal fluid, which is then absorbed into the blood and dissolves in it. Liquor constantly moves through the ventricles and spinal canals, being renewed again and again. One portion is released into the blood, and a new one is formed at this moment. This process does not stop. The most important functions of cerebrospinal fluid: it protects the brain from concussions and impacts on the skull bones, as well as from other mechanical injuries, nourishes it and removes decay products.
During circulation, the cerebrospinal fluid presses with a certain force on the cavities of the ventricles and the spinal canal from the inside. This pressure is called intracranial pressure.
Everyone has it, this is a normal phenomenon, unless the pressure level exceeds the usual levels. Otherwise, it is customary to talk about increased intracranial pressure. Because of this, the ventricles increase in size and, in turn, put pressure directly on the brain tissue.
What is intracranial pressure?
The human brain is located in the cranium and is an incredibly “delicate” substance that can suffer from the slightest impact. Therefore, to protect it, nature has provided our body with three barriers:
- The outer hard shell lines the cranial cavity from the inside; it differs from others in its strong and dense structure, which is dominated by elastic and collagen fibers.
- The middle arachnoid membrane is located behind the dura mater; it is thin and transparent. However, unlike the next soft shell, it does not penetrate into the furrows of the hemispheres and into the cracks between the parts of the brain. The choroid is separated from the arachnoid by the subarachnoid space, which is filled with cerebrospinal fluid ( CSF ).
- The inner choroid or pia mater fits tightly to the surface of the brain and penetrates its grooves and crevices. It consists of connective tissues that nourish the human brain and forms the choroid plexus, which is responsible for the production of cerebrospinal fluid.
Thus, ICP is the pressure on the brain structure of the cerebrospinal fluid (CSF), which protects from injury and damage, which fills the subarachnoid and epidural space, as well as the ventricles of the brain. In simple words, ICP is the difference between atmospheric pressure and pressure inside the cranial cavity.
Impaired circulation of cerebrospinal fluid leads to its deficiency and accumulation in some parts of the skull. An absolutely healthy person produces on average a liter of cerebrospinal fluid per day, which nourishes the venous vessels of the brain. In the presence of any pathologies, the cerebrospinal fluid is not absorbed in full, and its excess mass leads to an increase in intracranial pressure.
The structure and functioning of the brain is so complex that it has not been studied until now. Although it is already reliably known that normal ICP values depend on:
- vascular tone;
- cerebral perfusion pressure (level of blood supply to the brain);
- volumetric cerebral blood flow;
- resorption and production of cerebrospinal fluid, as well as its colloid-osmotic homeostasis;
- the degree of permeability of the blood-brain barrier between the nervous and blood supply systems of the body.
If at least one of the above factors changes, then a protective mechanism is triggered in the form of a compensatory reaction. As a result, blood pressure and cerebral vasoconstriction occurs, which affects the level of ICP and cerebral circulation.
High blood pressure, how much is it? During normal operation of all vital systems of the human body, ICP indicators range from 7.5 to 15 mmHg. It is important to note that pressure surges during the day are a completely normal phenomenon, unless, of course, they affect a person’s well-being and go away on their own without leaving a trace.
This is how our body can react, for example, to physical activity or a stressful situation. It’s another matter if a constantly elevated level of ICP is recorded. In this situation, a person begins to clearly feel the pronounced symptoms of malaise.
Signs of elevated ICP in adults
- severe headaches ;
- blood pressure surges;
- vomiting not associated with food intake , which does not bring relief;
- rapid heartbeat ( tachycardia );
- fast fatiguability;
- increased excitability;
- dyspnea;
- bruises or bruises under the eyes , which, upon closer examination, appear as a cluster of small veins close to the skin of the lower eyelid;
- muscle paresis ;
- decreased joint mobility;
- nervousness;
- weather dependence;
- hyperesthesia (increased sensitivity of the skin);
- excessive sweating or chills ;
- back pain;
- decreased potency or, conversely, increased sexual desire;
- increased intraocular pressure ;
- visual impairment (double vision, photosensitivity, blurring, short-term blindness).
It is important to note that in adults there are virtually no visible signs of intracranial hypertension , with the possible exception of unevenly dilated pupils and protruding eyeballs. In addition, during the day, the level of intracranial, as well as arterial (blood) pressure can change depending on the degree of activity or moral and psychological state of a person.
And this is considered a variant of the norm, since this is how our body “reacts” to external factors. Therefore, you should always listen to your body and not ignore its signals, attributing everything to fatigue or temporary poor health. For example, the very first harbinger of ICP is pain in the head, most often in the morning or at night, which sharply intensifies when tilting or turning the head, sneezing or coughing.
This symptom is directly related to such causes of increased blood pressure at night and after waking up as:
- apnea (snoring);
- stress;
- poor nutrition;
- overweight;
- chronic fatigue syndrome;
- bad habits;
- excess salt in the daily diet;
- disturbance of wakefulness and sleep patterns;
- lack of physical activity.
Symptoms of the disease
Increased intracranial pressure can be recognized by various signs.
- Headache of varying intensity. More often at night, since in a supine position the production of cerebrospinal fluid is activated and its absorption slows down.
- With increased cerebral fluid pressure, a person suffers from nausea and frequent vomiting. Moreover, this is not related to the digestive process. What is typical only for this pathology is that even after vomiting, relief does not come, since the pressure in the brain does not change.
- Nervousness, irritability for no reason, sometimes bordering on aggression, fatigue, even if this condition was not preceded by significant physical activity. This symptomatology is explained by the negative impact of hypertension on a person’s psycho-emotional state.
- Fluctuations in blood pressure, increased sweating, tachycardia, fatigue, chills, short-term fainting, and other symptoms inherent in vegetative-vascular dystonia can also develop when cerebrospinal fluid puts excessive pressure on the brain.
- With chronic intracranial hypertension, a person's sexual desire decreases. This is typical for patients of any gender.
Get diagnosed with intracranial hypertension at Clinic No. 1:
- Fundus examination
- Ultrasound of cerebral vessels
- X-ray of the head
- EEG
- Angiography
For one-time payment for services - 20% discount
Call
Causes and consequences of intracranial hypertension
- congenital pathologies of the venous sinuses, cerebrospinal fluid ducts or hydrocephalus resulting from an unfavorable course of pregnancy or head injury;
- prolonged labor;
- umbilical cord entanglement;
- birth injuries;
- increased intracranial pressure during pregnancy in the mother;
- infections affecting the central nervous system ( encephalitis, meningitis, neurosyphilis );
- hematomas and neoplasms (malignant, benign, cysts , parasitic accumulations , abscesses );
- otitis;
- malaria;
- mastoiditis;
- bronchitis;
- gastroenteritis;
- diseases of the endocrine system ( obesity , hepatic encephalopathy , hyperthyroidism , adrenal insufficiency );
- cerebral edema resulting from trauma (TBI) , stroke or after surgery;
- taking medications (oral contraceptives , Biseptol , retinoids, tetracycline antibiotics, nitrofurans, corticosteroids).
Without timely treatment, intracranial hypertension leads to:
- partial or complete loss of vision;
- respiratory dysfunction;
- mental pathologies;
- pinched cerebellum;
- confusion;
- edema and death ;
- convulsive conditions;
- fainting;
- hemorrhagic or ischemic stroke ;
- coma.
Treatment and prognosis
Therapeutic measures are prescribed based on diagnostic results. First of all, it is important to get rid of the cause that provokes excessive fluid pressure on the skull. If this phenomenon is caused by traumatic brain injury, the patient is advised to rest completely, take gentle nutrition, and take anti-inflammatory drugs. In some cases, surgical intervention is necessary (in the presence of hematomas between the membranes of the brain, as well as in the presence of injuries that require surgical treatment). Surgery is also prescribed when various tumors are detected in brain tissue that is prone to rapid growth.
A separate set of measures is carried out when diagnosing hydrofecal in a child. To remove excess fluid, a shunt is installed, through which it flows into the abdominal cavity, and the pressure is normalized. The operation is repeated as the child grows, and the patient is constantly monitored. In some children, the need for artificial fluid removal gradually disappears.
Drug therapy for ICP pathologies is secondary. However, drugs are prescribed to eliminate symptoms and make the patient feel better. The following medications may be helpful:
- hormonal anti-inflammatory drugs;
- neuroprotectors and substances for stimulating blood circulation in the brain - the effectiveness of this group has not been proven, despite its widespread use;
- loop diuretics (diuretics) - medications that stimulate the excretion of excess fluid;
- osmodiuretics - including reducing the production of cerebrospinal fluid.
The Clinical Brain Institute specializes in the diagnosis and treatment of diseases of the central nervous system. Increased intracranial pressure is not a separate disease, but a symptom that indicates a number of pathologies. Experienced specialists will accurately determine the cause of such a violation, as well as its severity and possible consequences. It is worth understanding that only timely seeking medical help can guarantee successful treatment and a return to your normal lifestyle without headaches.
Clinical Brain Institute Rating: 4/5 — 56 votes
Share article on social networks
How to measure intracranial pressure?
Constantly elevated ICP levels have a detrimental effect on brain function and can lead to the development of many serious pathologies:
- disruption of brain activity and damage to stem structures affects the level of intelligence, and also provokes the development of epileptic syndrome ;
- cessation of cerebral circulation due to increased pressure of cerebrospinal fluid on nerve tissues and blood vessels leads to ischemic stroke ;
- compression of brain tissue is fraught with the death of nerve cells and white matter of the cerebral cortex, which affects a person’s emotions and behavior;
- the accumulation of cerebrospinal fluid around the optic nerve compresses it and leads to visual impairment of varying severity.
Therefore, at the slightest suspicion, you should immediately consult a doctor for medical help. In addition, intracranial pressure, unlike arterial pressure, is simply impossible to measure independently. Unfortunately, for these purposes there is no specialized device, such as a tonometer , which can be used at home.
How is intracranial pressure measured in adults and children?
How to check if intracranial pressure is normal? Experts believe that the only absolutely accurate method of measuring ICP is puncture of the ventricles of the brain and spinal canal. However, this is a last resort measure that is used if the patient has most of the symptoms of intracranial hypertension .
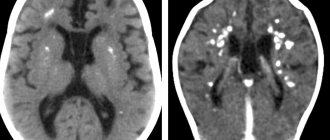
Procedures such as ultrasound, MRI, fundus examination, electroencephalography , x-ray of the skull bones, study of fontanelle pulsation with a Ladd monitor, neurosonography, Dopplerography or CT can reveal only indirect signs of malaise. Therefore, in this case, they all have a place, but still relate only to auxiliary diagnostic tools.
It is precisely because of the difficulty of identifying this pathology that many of our doctors play it safe and diagnose newborns with increased ICP without conducting sufficient diagnostics in the presence of at least a few general symptoms of malaise. In addition, they also prescribe medications to children for symptomatic treatment, although such a serious condition should be treated in the intensive care unit or intensive care unit of a health care facility.
However, if you still suspect that your child has intracranial hypertension , then the first thing you should do is visit a neurologist. The doctor will examine the newborn's fontanel, measure the circumference of the head, and may notice Graefe's syndrome or identify reflex abnormalities. This data, together with information from parents about the baby’s sleep and wakefulness patterns, his appetite or behavioral characteristics, will help the specialist make a diagnosis.
An ophthalmologist can also help identify problems with intracranial pressure by examining your child's eyes. Since in the presence of malaise, visible changes in the fundus of the eye can be noted (bulging or swollen optic nerve, spasms of the arteries, dilated veins).
When it comes to examining a baby whose fontanelle has not yet become overgrown, neurosonography (ultrasound) will help collect data on the size of the ventricles of the brain, its structure and development, and identify the presence of neoplasms or an increase in the size of the interhemispheric fissure. In accordance with the recommendations of the Ministry of Health of the Russian Federation, it is advisable to conduct such an examination at 1, 3 and 6 months.
Help with high intracranial pressure
Treatment aimed only at reducing blood pressure is inappropriate because it will allow the primary disease to worsen and recur.
The underlying disease should be treated based on the identified causes. For example, for bacterial infections, children are prescribed antibiotics. Diuretics are used to remove excess fluid from the body, including to reduce the amount of cerebrospinal fluid. In order to improve cerebral circulation, a course of treatment with nootropic drugs is carried out. Additionally, vascular drugs, neuroprotectors, sedatives and vitamins may be prescribed. In severe cases: with tumors, anatomical defects, aneurysm, surgical intervention is indicated.
Sometimes positive dynamics in treatment can be achieved with the help of physiotherapeutic procedures, massage, physical therapy, swimming, and acupuncture.
In addition to the standard course of treatment with medications, adolescent children are recommended to adjust their drinking regimen, normalize their sleep and rest patterns, spend a long time in the fresh air, include fruits and vegetables in their daily diet, limit salt intake, sleep on high pillows to ensure the outflow cerebrospinal fluid
Intracranial pressure in a child
Let's talk about how to understand that a child has increased intracranial pressure . To begin with, we note that children of different ages may show certain signs of this ailment. This is due to the developmental characteristics of the human brain.
Therefore, the symptoms of ICP in infants, whose fontanelles have not yet fully fused, differ from those in older children or adolescents. As a rule, the doctor notices the first signs of intracranial pressure in a child on an ultrasound of the brain, which is performed approximately a month after birth.
True, the diagnosis is not always confirmed, because During such a procedure, a newborn baby may experience discomfort and cry, which directly affects all of its physical indicators, including blood pressure. Therefore, it is important not to delay consultation with a neurologist if there is even the slightest suspicion of symptoms of cranial pressure in children in the first year of life.
Symptoms of increased intracranial pressure in children
From birth to 3 years:
- Excessive crying, frequent awakenings, trouble sleeping, and restless behavior that occurs in the afternoon or at night. During the day, the child may feel fine, play and eat normally, but everything changes when it gets dark. This is primarily due to the structure of the cerebrospinal fluid and venous system . We sleep in a horizontal position, in which the outflow of venous blood from the brain slows down , which, in the presence of any pathology, provokes the accumulation of cerebrospinal fluid and an increase in ICP.
- Nausea, frequent regurgitation or bouts of vomiting not associated with meals are reflex reactions to intracranial hypertension. Thus, the body tries to alleviate its condition and normalize blood pressure.
- Disproportionately increased size of the head, frontal part, pulsation and protrusion of the fontanelles, divergence of the bones and sutures of the skull. This is one of the obvious and therefore sure signs of pathology ( hydrocephalus ). This condition is caused by an increased amount of cerebrospinal fluid in the spaces of the brain.
- Visible venous network appearing under the skin on the child's head. Hypertension leads to excessive filling of the veins with blood and its stagnation.
- Graefe's syndrome or the "setting sun" symptom. This poetic name hides signs of dysfunction of the optic nerves. This condition may be a consequence of increased ICP, birth trauma, or an underdeveloped nervous system. Most often, this diagnosis is given to premature babies. The syndrome manifests itself as an uncontrolled downward deviation of the eyeballs, while a white stripe (sclera) becomes visible between the upper eyelid and the edge of the iris.
- Convulsions or periodic twitching.
- Refusal to feed. The child does not want to eat because... the sucking reflex increases intracranial pressure and increases pain.
- Dystonia, muscle tone.
- Lag in physical and psycho-emotional development, lack of weight gain is a consequence of the baby’s constant poor health and poor nutrition.
Over 3 years old:
- attacks of nausea and vomiting, which does not bring relief, unlike food poisoning;
- disrupted hormonal levels;
- developmental delay, for example, speech problems in a child who can already speak;
- severe headaches in the evening and at night;
- disproportionately large forehead;
- inattention, drowsiness, irritability, fatigue and frequent apathy towards everything;
- impaired motor coordination, often children 3-4 years old begin to tiptoe;
- vision problems (double vision, flashes before the eyes, etc.);
- pain behind the eyeballs;
- chin tremor;
- dizziness and frequent fainting;
- hyperactivity;
- restless sleep.
Causes of the disease
Symptoms of intracranial pressure in children develop for a number of pathological reasons that contribute to the disruption of the outflow of cerebrospinal fluid from the cerebral ventricles. Due to the excess amount of cerebrospinal fluid in these cisterns and between the meninges, it leads to a significant increase in ICP levels.
This condition is caused by the following reasons:
- Intrauterine hypoxia - manifested by a lack of oxygen during difficult or overly prolonged labor. The condition is also provoked by various pathologies of the placenta.
- Birth injuries - if a Caesarean section is performed or the child is removed from the birth canal using forceps (and sometimes simply squeezed out of the abdomen during weak labor), the cerebral ventricles are damaged. In addition to mechanical damage, there are even ruptures of the tanks containing the cerebrospinal fluid.
- Asphyxia - if a child was in utero for a certain time with an insufficient amount of oxygen or without it at all, the content of carbon dioxide in the newborn’s blood is significantly increased. For this reason, the outflow of cerebrospinal fluid is disrupted and intracranial hypertension develops.
- Infectious diseases - increased intracranial pressure in a child can occur as a result, for example, of meningitis. Pathogenic pathogens (viruses and bacteria) can bypass the blood-brain barrier very easily due to their microscopic size. Therefore, when microbial flora penetrates the meninges, an inflammatory process develops, leading to various complications, including increased pressure.
- Congenital anomalies - for example, with Arnold-Chiari syndrome, the foramen magnum of the medulla oblongata is infringed, as a result of which cerebrospinal fluid cannot fully flow out of the cerebral ventricles.
- Toxic poisoning – toxins entering a child’s body cause significant harm by penetrating the blood-brain barrier and causing problems with the circulation of cerebrospinal fluid.
- Injuries to the cervical spine are subluxations, displacement of discs, the results of birth injuries that disrupt the outflow of cerebrospinal fluid from the brain.
- Neoplasms - often growing tumors in the spinal cord and brain can be identified by a pronounced increase in ICP in a child, since the formations compress the ventricles and membranes of the canals.
- Intracranial hemorrhage - as a result of traumatic brain injury or hemorrhagic vasculitis, consequences arise that are dangerous to the health and life of the child, including hypertensive-hydrocephalic syndrome.
Obesity and diseases of the endocrine system are also considered to be non-main, but indirect causes of increased intracranial pressure in children.
If the functions of the thyroid gland are impaired or the functioning of the adrenal glands suffers, a spasm of the blood vessels that supply the brain parts occurs in the body - as a result, this gradually leads to the development of hypertensive syndrome.
No ads 2
Intracranial pressure in infants
All parents are happy when their newborn baby eats well, sleeps peacefully and cries little. But it happens that the baby refuses to breastfeed, constantly burps and cries bitterly. In such a situation, doctors often record signs of intracranial hypertension .
What is ICP in an infant and how can this condition be dangerous for children in the first year of life? According to modern pediatricians, including the famous Dr. Komarovsky, increased intracranial pressure is not an independent disease, but only a symptom of some serious neurological abnormality.
Moreover, the list of such conditions is actually small and is limited to several dozen reasons that can be triggered by birth trauma, genetic inheritance or acquired diseases. It is really important to diagnose such a pathology and undergo appropriate treatment, because The life and health of the child depends on this.
It is worth noting that the treatment of intracranial pressure in infants must be justified and justified. Unfortunately, according to statistics, many doctors in the CIS diagnose intracranial hypertension and prescribe treatment with serious drugs to newborn children without conducting a sufficient examination.
This is why all mothers are afraid of ICP like fire. But let's soberly assess the situation. In any person, intracranial pressure can fluctuate at any particular time or under certain circumstances.
Remember, ICP is a variable value even in the healthiest and strongest child, its level is constantly changing and depends on many factors (sleeping, playing, running, sitting on the potty, crying, screaming, walking outside, when it’s warm, cold, or raining and so on).
Therefore, from the point of view of evidence-based and civilized medicine, a doctor should not consider ICP as an independent diagnosis, much less treat the signs of this condition. The specialist must find the cause of the constantly elevated level of intracranial pressure , which is associated with other neurological symptoms.
In the vast majority of cases, hydrocephalus (water on the brain) is considered the main cause of intracranial hypertension in newborns. This disease is characterized by the accumulation of excess amounts of cerebrospinal fluid in the ventricles of the brain. Cerebrospinal fluid accumulates because... does not move from the site of secretion to the site of absorption.
Most often, this is a congenital disease caused by heredity, difficult pregnancy, medication taken by the mother, birth injuries, and intrauterine infections. This disease is usually diagnosed immediately after birth. However, hydrocephalus can also be acquired as a result of brain injuries and infectious diseases.
Symptoms of ICP in infants
Parents can be the first to detect signs of intracranial pressure in a baby. True, as we said earlier, in most cases, moms and dads panic in vain. But it’s better to play it safe and see a doctor for a more detailed examination if there is even the slightest suspicion.
The main symptoms of increased intracranial pressure in infants:
- continuous crying at night and restlessness with absolutely normal behavior during the day;
- problems with sleep and falling asleep, frequent awakenings (consequences of the first symptom);
- enlarged head size inappropriate for age, bulging fontanelles, clearly visible venous network on the head, divergence of cranial sutures;
- breast refusal;
- Graefe syndrome;
- convulsive syndrome;
- retardation in physical and mental development due to all of the above reasons.
How to determine intracranial pressure in a newborn? We mentioned above that there is no device for measuring ICP that you can use at home yourself. Reliable information about the level of intracranial pressure can only be provided by puncture of the ventricles of the brain or spinal canal.
This procedure is performed only in a hospital setting and only when there are sufficient indications for it. Since the fontanel of infants has not yet healed, there are other diagnostic methods that really do not give 100% confidence, because They record only indirect signs of malaise. However, at older ages these procedures are considered even less effective.
The first thing a neurologist or pediatrician will pay attention to is the dynamics of an increase in the circumference of the baby’s head. This means that it is not the specific numbers that are important, but the speed at which they increase. For example, at 3 months a child’s head circumference is 43 cm, which is normally considered a critically high indicator.
But then the growth rate slows down and falls within normal limits. Therefore, there is no reason to worry or panic. It’s another matter if, over the next month of life, the child’s head circumference sharply increased by 7 cm. Such a jump is considered negative dynamics and signals the development of a dangerous pathology.
Perhaps the most accessible and at the same time safest diagnostic method can be considered neurosonography of the brain (in simple words, ultrasound). It makes it possible to assess the size of the ventricles, an increase in which is considered a sign of intracranial hypertension.
Computed tomography or magnetic resonance imaging are more expensive and not always justified methods from the point of view of the safety of very young children, which are used after the fontanel has closed. You should resort to their help only if there is a real suspicion of the development of serious pathologies accompanying ICP.
Treatment
What to do if a child has been diagnosed with intracranial hypertension? Follow the doctor’s recommendations and do not think that the signs of pathology will go away on their own. Of course, unexpressed symptoms may fade over time and it will seem that the child has fully recovered. But in the future, untreated pathology will manifest itself as increased nervous irritability, educational lag, hyperactivity, and difficulties in communicating with peers. The child may develop sleep disorders, he will be bothered by causeless headaches, and he will grow up prone to depression.
General principles of condition correction
You need to understand that you should not immediately stuff your child with chemicals, especially if the neurologist believes that the clinical picture of ICP is not clearly expressed and can still be corrected in other ways. Here is a list of recommendations for such cases:
- compliance with the drinking regime (you cannot give your child one and a half liters of liquid per day);
- proper nutrition and taking vitamin complexes;
- moderate physical activity and hardening procedures (children with signs of pathology benefit from swimming);
- prevention of stress and psycho-emotional overload - at school, kindergarten, at home;
- walks in the fresh air, ensuring the flow of oxygen into the living space (frequent ventilation).
Also, a child with symptoms of intracranial hypertension is advised to follow a daily routine - you need to teach him to get up and go to bed at the same time, limit the time he spends at the computer and TV. Sleep should last at least 8 hours; children of preschool age can be given additional daytime rest. If a child has problems with speech, he needs to be shown to a speech therapist and undergo a course of developmental classes to correct speech function.
No ads 3
Drug therapy
If the cause is a neuroinfection, the doctor will prescribe a course of antibacterial drugs. The standard course of therapy includes taking several groups of medications:
- diuretics that expel excess fluid from the body, thereby reducing the symptoms of high blood pressure - Furosemide, Acetazolamide, Triampur;
- nootropic drugs designed to improve the supply of blood, nutrients and oxygen to the brain - Pantogam, Tanakan, Pantocalcin, Piracetam, Cavinton;
- means of calming action and stimulating the work of brain cells - Glycine, Nervohel;
- sedatives according to indications and depending on the age of the child.
To reduce the manifestations of hypertensive syndrome, it is necessary to identify the root cause of the disease and begin treatment from it
A course of injections of vitamin B is required, as it helps normalize the functions of the nervous system. Other medications are recommended by a neurologist, based on the clinical picture and complexity of the disease. In severe cases, when it is not possible to eliminate the signs of high blood pressure conservatively, an operation is performed - bypassing the cerebral ventricles to eliminate excess cerebrospinal fluid.
Additional procedures
In addition to drug therapy, young patients diagnosed with ICP are prescribed a set of additional measures, including:
- sessions of general massage or separately for the collar area;
- heat treatment (paraffin, ozokerite);
- Exercise therapy with moderate loads;
- physiotherapy – SMT, magnetic therapy, electrophoresis with magnesium, calcium;
- microcurrent reflexology – impact on areas of the brain with individual low-intensity electrical impulses;
- homeopathy;
- manual therapy.
Massage is an effective method to reduce the manifestations of increased intracranial pressure in a baby.
During the course of treatment, the child should be provided with a diet with a limited amount of table salt, as it promotes fluid retention in the tissues and increases blood pressure. Do not think that increased intracranial pressure is an incurable diagnosis. With regular courses of therapy (for children with severe symptoms, courses are recommended once every three months, and once every six months as the condition improves), improvements will not take long.
Severe forms of the disease are fraught with dangerous consequences - mental illness, coma, breathing problems, cerebral edema, fainting and convulsions. Such complications are rare, since modern medicine has a lot of drugs and methods for treating increased ICP, but you should not forget about the seriousness of the disease.
How to treat intracranial hypertension in children?
Before talking about methods of therapeutic treatment of ailments, you should understand what pressure children should have at different ages. After all, physiological indicators, which include pressure, in a child of 10 years old may differ slightly from the standards established for 8 years old, due to the small difference in age.
The same can be said about the normal blood pressure in a child at 6 years old and at 5 years old. It’s a different matter when compared with infants or young children. For newborns, normal ICP values are set at 1-2 mmHg, for children aged one year and older - 3-7 mmHg, for teenagers - 5-15 mmHg.
However, this is very conditional data, since they vary not only depending on age, but also, for example, body position (the child is sitting or lying down when measured). In addition, until now, scientists still cannot agree on which maximum permissible limits of ICP values are within the boundaries of normal values, and which are considered a deviation.
Make an appointment with a neurologist
Experienced specialists conduct consultations in the neurological department of the private Multidisciplinary Medical Hospital. Get rid of unpleasant symptoms and prevent complications caused by increased intracranial pressure by completing a course of treatment.
Information on prices for initial and repeated paid appointments with a neurologist is presented on our website. You can make an appointment with a specialist at a convenient time by phone or using the online form on our website.
Moscow, st. Krasnodarskaya, house. 52, bldg. 2
+7
We work on weekdays and weekends from 8.00 to 21.00