Competition “Bio/Mol/Text”-2020/2021
This work was published in the “Own Work” category of the “Bio/Mol/Text” competition - 2020/2021.
The nomination partner is the Russian Science Foundation.
The general partner of the competition is the annual biotechnology conference BiotechClub, organized by the international innovative biotechnology company BIOCAD.
The sponsor of the competition is SkyGen: a leading distributor of life science products on the Russian market.
Competition sponsor: the largest supplier of equipment, reagents and consumables for biological research and production.
"Book" sponsor of the competition - "Alpina Non-Fiction"
More than 5 million people in the world suffer from various forms of paralysis, the main causes of which are stroke (34%) and spinal cord injury (24%).
Stroke is currently one of the main causes of disability in the population. In Russia, more than 450,000 strokes are registered annually, and 70–80% of stroke survivors become disabled, with approximately 20–30% of them requiring constant outside care.
Over the past 70 years, the number of patients with spinal cord injury has increased 200 times, and in Russia more than 8,000 people suffer such injuries every year. Most often, this leads to the patient’s inability to move independently and provide for their basic needs. As a result of using a wheelchair, physical activity decreases, which provokes the development of a number of diseases: heart disease, osteoporosis, bedsores. Therefore, there is an active search for alternative methods of restoring the ability to move. One of the newest developments in this direction is the neural interface.
Neurointerface (also known as brain-computer interface, BCI) is a system that allows you to transmit brain signals directly to an external device (this can be a wheelchair, exoskeleton, computer, etc.), in fact, control the “power of thought” (Fig. 1) .
In “Biomolecule” you can read in more detail about the history of the development of neurocomputer technologies, as well as about Elon Musk’s modern Neuralink project [1], [2].
Figure 1. BCI operation diagram.
adapted from materials from the Tritriwulansari website
Indications for TES therapy
Electrical stimulation of the brain is prescribed for various diseases and conditions of the human body:
- pain of various nature (headache, neuralgia, radiculitis, trauma, phantom pain);
- shock after stress;
- increased blood pressure;
- heart diseases;
- diseases of the gastrointestinal tract;
- ENT pathologies;
- withdrawal symptoms;
- drug addiction and alcoholism;
- toxicosis during pregnancy;
- sleep disturbance;
- consequences of strokes.
Methods for recording brain signals
The first link in the BCI operation scheme is receiving a signal from the brain. The following methods are used for this:
- electroencephalography (EEG), which records electrical signals from the brain;
- magnetoencephalography (MEG), which records magnetic fields resulting from electrical activity in the brain;
- near-infrared spectrometry (NIRS), which measures the saturation of blood with hemoglobin (the more active a group of neurons, the more it uses oxygen carried by oxyhemoglobin);
- functional magnetic resonance imaging (fMRI), based on measuring blood flow to different areas of the brain (the more active a group of neurons, the greater the blood flow to it).
Nowadays, EEG is most often used in BCIs to obtain information about the electrical activity of the brain, since it has a high temporal resolution (electrodes allow one to read the immediate activity of individual parts of the brain), is relatively cheap, portable and does not pose a risk to users. EEG-based BCIs consist of a set of sensors that detect EEG signals from different areas of the brain. However, the quality of EEG signals is degraded because the signal travels through the scalp, skull, and many other layers, which creates noise.
To reduce noise and improve recording quality, they resort to invasive methods - implanting a set of microelectrodes inside the skull [3]. This implies significant health risks, which is why they are rarely used in experimental practice. There are two invasive approaches to BCI research: electrocorticography (ECoG), in which electrodes are placed on the surface of the cerebral cortex, and intracortical recording of neural activity, in which sensors are implanted into the cortex (Fig. 2). Such solutions are currently used extremely rarely, only in exceptional cases: either when the patient is already undergoing brain surgery, or when this is the only chance to regain the ability to interact with the outside world.
Figure 2. Electrode layout for EEG, ECoG and intracortical microelectrodes.
adapted from [3]
How to boost your brain function
Denis Tulinov “Trinity Option” No. 10(79), May 24, 2011
Humanity has long experimented with a variety of ways to temporarily change the way the brain works to gain capabilities that are not available naturally. As a rule, these methods come down to the use of natural or synthesized substances, which, however, immediately affect the entire brain. Scientists have a tool at their disposal that allows them to selectively and locally influence individual areas, enhancing one or another function. This tool is an electric or magnetic field, and its use sometimes leads to amazing results.
X-ray of a minimally conscious patient with deep brain stimulation electrodes implanted in his head. AP Photo
April issue of Nature
talks about the experiments of Vincent Clark, a neuroscientist from the University of New Mexico (USA).
Clark discovered that transcranial direct-current
(tDCS) enhances learning. According to the conditions of the experiment, a group of volunteers had to play the computer game DARWARS Ambush!, developed for training military personnel sent to Iraq.
Its essence lies in developing the ability to notice objects hidden against the backdrop of a complex landscape. Using electrodes placed on the head, subjects received 30 minutes of electrical stimulation on the right side of the brain while playing. Participants who received a current of 2 milliamps performed twice as well as those who were stimulated with a current of only 0.1 mA. "They learned faster, but they didn't have any assumptions or gut feelings about why it was happening," Clark says. The scientist sees tDCS as a way to practically separate the mechanisms of learning and consciousness. This area of research, he said, "will soon experience explosive growth and will provide us with a wealth of new information while at the same time posing new questions."
In the 2000s, understanding began to emerge as to what accounts for the observed effects of tDCS. Direct current creates an electric field in brain tissue that changes the potential difference between the sides of cell membranes. The so-called “anodic” stimulation, in which the current is directed to the electrode, leads to the depolarization of neurons, resulting in an increase in their readiness to respond with a spike to an incoming signal from other cells. Accordingly, “cathodal” stimulation, in which current flows from the electrode, causes the opposite effect, increasing the potential difference between the outer and inner sides of the membranes and thereby reducing the excitability of neurons. More recently, neuroscientists from the California Institute of Technology were able to experimentally show that extracellular electric fields actually change the characteristics of action potentials of nerve cells.
According to pharmacological studies, in the area of synaptic contacts, under the influence of electric current, the production of NMDA receptor increases. This enhances the plasticity of neural tissue, temporarily giving it a state in which neurons tend to rewire their connections in response to an external stimulus, such as learning a new behavior. For example, in 2009, Leonardo Cohen from the National Institute of Neurological Disorders (Maryland, USA) showed that tDCS improved the ability of subjects to learn simple coordination exercises, and this improvement was maintained three months after the experiment.
In addition to accelerating learning processes, brain stimulation affects a number of other mental properties. In particular, this technique is seriously considered as a promising means for the treatment of depression, post-traumatic stress, delayed speech and mental development, and other nervous disorders. In 2007, Felipe Franey from the Center for Non-Invasive Brain Stimulation (Boston, USA) and Paolo Boggio from Mackenzie University (São Paulo, Brazil) discovered the interesting effect of tDCS.
It turned out that direct current exposure to the area located above the temple, the so-called dorsolateral prefrontal area, leads to the fact that a person becomes less ready to make risky decisions. As part of the experiment, scientists asked students to play a simple game where pressing a key filled a balloon depicted on the screen with air. The more the balloon is inflated, the more virtual money the participant gets.
At the same time, if the ball bursts, all savings are lost.
Subjects treated with tDCS behaved more cautiously and stopped earlier than those not exposed. According to Bojo, this result can be used to treat various types of addictions in which people lack “inhibitory control” of their actions.
These and a number of other similar experiments allow us to conclude that even a weak and short-term effect of the field on the brain, as in the case of tDCS, is enough to improve its performance. At the same time, at least two questions inevitably arise: 1) why the more effective mode in natural conditions is turned off and 2) how great is the potential of stimulation in terms of enhancing human cognitive abilities. In general, it is too early to talk about answers, but the experiments of neuroscientist Allan Snyder provide some food for thought in this regard.
Professor Allan Snyder will bring out the genius in you. Photo from the site www.zrobtosam.com
Professor Snyder directs the Center for the Study of Consciousness in Sydney, Australia. He claims that everyone
of us has the capabilities that are demonstrated by the so-called
savants
, people with extraordinary abilities. In the normal brain, these capabilities are present, but are suppressed by high-level information processing that organizes holistic semantic perception. For savants, access to raw, unprocessed data is not blocked, and they use directly what the brain contains. Unfortunately, most often such open access is accompanied by autism, but there are exceptions. For example, the mentally healthy Orlando Serell began remembering details of every day of his life after he was hit in the head by a baseball at the age of 10.
In the average person, high-level blocking can be temporarily relieved by low-frequency transcranial magnetic stimulation. In Snyder's experiments, magnetic pulses were sent to subjects' left anterior temporal lobe (LATL), after which they showed marked improvements in drawing, reading, and counting abilities. The LATL area is involved in semantic processing and category formation, and magnetic stimulation is somewhat analogous to the temporary suppression of this area. As a result, Snyder suggests, the activity of the right hemisphere is released, and the person begins to perceive a stream of low-level data coming from there.
The professor suggests that photographic memory, multiplying numbers in the mind, the ability to draw well and other abilities of savants are all properties characteristic of any brain. Except that savants have access to them, while for others it is blocked by the activity of the left hemisphere. But hypothetically, you can learn to influence the brain in such a way as to remove artificial inhibition and gain these amazing capabilities. If Snyder is right, we will see a time when people will have a cognitive enhancer at their disposal and use it in their activities.
The use of magnetic stimulation, as well as transcranial direct current stimulation (tDCS), are non-invasive methods of influence, which, in addition to the obvious advantages, have one drawback. Due to the fact that the field source is located on the surface of the skull, only a small layer of the cortex is affected, beyond which stimulation has no effect. However, there are structures in the brain that are located quite deep, and applying electric current to them also leads to surprising and beneficial results for humans. To reach these structures, scientists use a method of deep implantation of electrodes into brain tissue.
In some cases, if an electrode is inserted into the brain and voltage is applied to it, unexpected memories are awakened in a person. Wilder Penfield was the first to document this in the 1950s. He treated patients with epilepsy using Deep Brain Stimulation
, DBS). During the procedure, people remained conscious and described their sensations in detail. When the current was applied, various scenes from their lives appeared before their eyes. The past literally burst into the present: patients saw what was happening, heard voices, sounds, smells. They recognized their friends, relatives, their surroundings, and could name the exact place in the city where they “were” at that moment. At the same time, they were aware that in reality they were lying on the operating table in Montreal, simultaneously existing in two worlds. Memories were not static. They unfolded at a natural speed, as if the somatic experience was being relived. Music was often recalled - patients heard a song that developed from phrase to phrase, from chorus to verse, so that they could sing along. The same fragment of a work could be recalled from memory by again applying current to the electrode. Remarkably, the neurons involved fired more easily the second time, responding to less voltage.
From time to time, researchers repeat the results described by Penfield. For obvious reasons, they can only be a side effect of the experiment, since deep electrical stimulation requires surgery and is used only for therapeutic purposes. In 2008, the Annals of Neurology
reported the case of a 50-year-old patient who was being treated for obesity using DBS. Suddenly this caused him to vividly experience an episode 30 years earlier. He found himself in the park with his friends. Among the people he also saw his girlfriend from that period of his life. The clothes of those around them corresponded to the past time, people in the park were talking. The memory was colorful. Interestingly, increasing the voltage from 3 to 5 volts caused the scene to become more vibrant and detailed. Apparently, a huge number of fragments of our lives are stored somewhere deep in neurons and remain forever hidden from our attention.
The technique of transcranial direct current brain stimulation (tDCS) is alarmingly accessible. Photo from 2.bp.blogspot.com
In addition to reviving memories, deep stimulation can sometimes literally revive something more important - a person's consciousness. It is worth noting the successful experiment of a whole team of doctors and neurologists who were able to restore key brain functions in a man who had been in a state of minimal consciousness for six and a half years. As a result of a robbery in 1999, he suffered extensive head injuries and lost the ability to communicate and behave purposefully.
As tomographic studies later showed, some important areas of the cortex remained intact, but did not function. This circumstance interested scientists. They hypothesized that the mechanism that activates the cortex was switched off as a result of the injuries. The key role here belongs to the thalamus - the structure in which the processing and integration of almost all signals going to the cerebral cortex from the spinal cord, midbrain, cerebellum and basal ganglia occurs. According to doctors, if the nuclei of the thalamus are subjected to electrical stimulation, this can lead to the awakening of preserved areas of the cortex. However, the thalamus is located deep in the brain, so no non-invasive technique can reach it. The only option is to insert electrodes surgically.
After long discussions, mainly related to ethical conflicts that arose in connection with operating on a person without his consent, the procedure was performed. Almost immediately, in the first two days of operation of the electrodes, the patient’s condition noticeably improved. He began to keep his eyes open for a long time and respond to voices by turning his head. The scientists, however, were forced to pause for 50 days to ensure that the improvement was not an unknown effect of the surgery. Then, over the course of 18 weeks, the thalamus was stimulated with different combinations of frequency and duration of excitations in order to find the best option.
The patient actually returned to life. He began to answer questions, could hold objects in his hands and move his limbs. He began to swallow food, but before that he had been fed through a gastronomic tube for six years. His mother, in an interview with the press, could barely hold back tears: “Now my son can talk, eat and watch movies. He can drink from a mug. He can express pain. He can laugh and cry...” This was the first time that deep brain stimulation (DBS) was able to pull a patient out of a state of minimal consciousness.
As can be seen from the above, the brain can be stimulated in different ways, by bringing an electric or magnetic field closer to it, or by placing the source directly inside the head. However, another option worth mentioning is that the brain receives stimulation even when the electrical current is applied to another, correctly selected, part of the body. And this part of the body is the tongue. Electrotactile stimulation of the tongue has been experimentally shown to markedly improve motor coordination, balance, and speech in people experiencing difficulties as a result of brain injury or illness.
Research in this direction is being carried out by our compatriot Yuri Danilov, who heads the Laboratory of Tactile Communication and Neurorehabilitation at the University of Wisconsin (USA). According to him, this technology will allow the development of new clinical applications of non-invasive neuromodulation for brain injury, multiple sclerosis, stroke, Parkinson's disease and, in addition, enhancing the capabilities of human sensory systems.
Most of the described brain stimulation methods still require special equipment and do not go beyond medical centers and scientific laboratories. At the same time, there are serious concerns about tDCS: to reproduce the experience at home, all you need is a couple of wires, a resistor and a regular 9-volt battery. If ordinary people (for example, students before an exam) begin to use such brain pumping, this will give them an advantage and, more importantly, will create conditions in society that push citizens to use such devices. Scientific progress, as usual, brings with it various consequences, and the task of Homo sapiens is to adequately understand them.
Literature:
Fox D. (2011).
Neuroscience: Brain buzz - Nature
.
C. A. Anastassiou, R. Perin, H. Markram, C. Koch (2011). Ephaptic communication in cortical neurons
–
Nature Neuroscience
.
Snyder A. W. (2009). Explaining and inducing savant skills: privileged access to lower levels, less-processed information
—
Phil.
Trans. R. Soc. B. _
Chi R. P., Snyder A. W. (2011). Facilitate Insight by Non-Invasive Brain Stimulation
-
PLoS ONE
.
Hamani, C et.
al (2008).
Memory enhancement induced by hypothalamic/fornix deep brain stimulation
–
Annals of Neurology
.
N. D. Schiff et al.
(2007).
Behavioral improvements with thalamic stimulation after severe traumatic brain injury
-
Nature
.
Sensorimotor rhythm and motor cortex
As we have already said, the purpose of a BCI is to capture the user's intention by recording their brain activity. When recording brain activity using EEG, we get a graphical representation of a complex oscillatory electrical process, in which we can identify a number of specific rhythms that differ in amplitude and frequency: alpha, beta, delta, mu and others. Now we are interested in the mu rhythm, since it is on its basis that the neural interfaces used in neurorehabilitation of movements work.
The mu rhythm, or sensorimotor rhythm (SMR), has a frequency of 8–13 Hz and is recorded over the motor area of the cerebral cortex, located in the posterior part of the precentral gyrus (Fig. 3). Suppression of the mu rhythm occurs when a person performs a movement or imagines performing a movement—this is called event-related desynchronization (ERD). This occurs because neurons that previously fired synchronously acquire individual firing patterns that are different from each other. In this case, a person can train in imagining movements, and over time, the suppression of the mu rhythm becomes more and more pronounced, which is used when learning to control a BCI.
The motor cortex is characterized by a topical organization. This means that each section of the cortex corresponds to a specific area of the body that it controls. Figure 3 shows Penfield's homunculus, whose body parts are proportional to the brain areas in which they are represented. As can be seen from the figure, the representations of the upper and lower extremities are located far enough from each other, making it possible for the neural interface to separately recognize the movements of the arms and legs.
Figure 3. Somatosensory and motor homunculus.
adapted from materials from the BioNinja website
Note that the representation of the lower extremities in the motor cortex is much smaller than that of the upper extremities. This is easily explained by the presence of fine motor skills of the hands: the brain needs to control many individual muscles of the fingers. The legs, on the other hand, have fewer muscles to control and are larger. In addition, it is clear that the representation of the lower extremities falls into the interhemispheric fissure, which makes it difficult to recognize EEG signals generated by imagining the movements of different groups of leg muscles. Therefore, the use of BCIs for the legs causes certain difficulties, and most of the existing scientific works on neurorehabilitation using BCIs are devoted specifically to the upper extremities, since it is easier to work with their imagination. In the laboratory of movement physiology of the Institute of Physiology named after. I.P. Pavlov RAS, where the author works, conducts research aimed at studying the processes of rehabilitation of the lower extremities, as well as the possibility of using transcutaneous electrical stimulation of the spinal cord (TESCS) and special practices that help increase the efficiency of BCI control [4].
Design and operation of a beckoning stimulator
Transcranial magnetic stimulator Neuro MS/D
1 - main unit; 2 - cooling module; 3 — replenishment module; 4 — bracket for the inductor; 5 - software
TMS device
consists of three main parts: a system of high voltage (more than 3.5 kV) and high current capacitors, a coil (coil) and a control unit. 1718 There are additional technical elements that ensure a comfortable procedure and proper operation of the magnetic stimulator: a cooling module for the device, a handle (bracket) for fixing the coil, software.
- The main block is the basis of the system. Its front panel contains controls and indicators that reflect the operating parameters of the stimulator. Can be connected to a computer via a USB cable. The main unit can operate at frequencies up to 30 Hz; maximum induction is carried out at a frequency of up to 5–7 Hz;
- The cooling module is a liquid cooling system. With the help of the cooling module, the session is carried out much faster, without the need for breaks to exchange or cool the coil during the session or between patients. The coolant does not fill the inductor, but moves along the winding, removing thermal energy from the place of its formation;
Cooling module operation
- Replenishment module - an additional power supply increases the maximum stimulation frequency to 100 Hz, and the maximum induction frequency to 20-25 Hz. Using the replenishment module makes it possible to conduct theta-burst stimulation (TBS), in which the session is significantly shorter than conventional TMS;
- Bracket for the inductor – allows you to hold the inductor in the same position relative to the patient’s head throughout the entire session;
- Software – “neuro-MS.NET” program. Using a computer, the software provides control of the patient database, management of courses and sessions, conducting stimulation according to existing programs and creating your own programs for TMS.
Types of inductors:
Ring inductor –
has a coil diameter of 150 mm. Used for peripheral muscle stimulation and cortical bilateral stimulation. Suitable for peripheral stimulation in urology and coloproctology;
Ring inductor
Inductor – figure eight –
has a coil diameter of 100 mm. Compared to a ring inductor, it provides stimulation of deeper tissues.
Figure-of-eight inductor
Distribution of the magnetic field of the field in a ring inductor and a figure-of-eight inductor
Angular figure-of-eight inductor
– has a coil diameter of 100 mm. It has an anatomical shape that matches the shape of the head. Used for deep cortical stimulation.
Angular figure-eight inductor
Double conical inductor
– has a coil diameter of 125 mm. Provides the deepest stimulation. Suitable for stimulating the cortical representations of the muscles of the lower limbs and pelvic floor, cerebellum and DMPFC.
Double conical inductor
Each inductor has a device readiness indicator on the side surface (lights up green) and a magnetic stimulus supply button.1920
The principle of operation of a magnetic stimulator
consists in generating a current by a system of capacitors, transmitted to the coils, with the subsequent formation of a magnetic field in them (up to 2.2 Tesla). As a result, the nerve tissues form their own electrical impulse, passing through the pathways from the stimulated cortical structures to the tissues and muscles that have representation in them.21
It is worth noting that magnetic stimulators, depending on the purpose of TMS, are capable of generating different types of stimuli: 222324
- Monophasic stimulus
- the current in the inductor with this stimulus flows in one direction, increasing according to a sinusoidal law and decreasing exponentially;
Monophasic stimulus
- Biphasic stimulus
- the current in the inductor with this stimulus is characterized by one period of a damped sinusoid;
Biphasic stimulus
- Biphasic burst stimulus
- stimulation in which a series of biphasic stimuli with a high frequency (up to 100 Hz) and decreasing amplitude is issued;
Burst stimulus
- Paired monophasic stimulus
- two stimuli with a specified inter-stimulus interval and amplitude set independently for each stimulus.
Paired monophasic stimulus
Thus, today a number of magnetic stimulators have been created that meet different requirements and purposes of TMS.25
Line of magnetic stimulators from the Neurosoft company
In addition to magnetic stimulators from the Neurosoft company, stimulators from the MagVenture company are widely used: MagPro R100, MagPro R30, MagPro x100.262728 Magnetic stimulators of this line differ in terms of maximum stimulation frequency and pulse shapes, depending on the purposes of TMS. The principle of operation and structure of the devices is the same as in the description above. These devices operate without specific software based on a built-in computer, which has everything necessary to track indicators and store results during TMS.
How to Imagine Movement Effectively
The following features of movement imagination are known that increase its effectiveness:
- Kinesthetic (paying attention to sensations from muscles and joints) representation, rather than visual [5];
- First person presentation rather than third person [6];
- Imagination of movements after an actual action [7];
- Using feedback (when a person is shown how well he is doing a task) [8]. Feedback in the form of virtual reality showed high efficiency: when imagining leg movements, the avatar controlled by the subject goes forward, and when imagining stops, it stops. The subject’s task is to go forward and stop at certain points in virtual space [9–12];
- Simultaneous viewing of a video in which the corresponding movement is performed helps to enhance desynchronization of the mu rhythm due to the work of mirror neurons [13];
- The use of meditative practices, in particular, mindfulness meditation [14].
In addition, we have shown that the effectiveness of motor imagery depends on a person’s personal characteristics [15].
For the experiment, 44 people with a dominant right hand were recruited. All of them were tested using the Cattell questionnaire, which identifies 16 basic individual characteristics. Next, the subjects controlled the BCI based on the imagination of hand movements. It turned out that when imagining the movements of the right hand, expressive, sensitive extroverts were more successful, while when imagining the movements of the left hand, practical, reserved, skeptical and not very sociable people were more successful.
We hypothesize that this can be explained by different levels of dopamine in the right and left hemispheres, as well as differences in the way information about movements is encoded [16]. You can read more about this in the article published by the author and colleagues in the journal “Proceedings of the Academy of Sciences” [15]. Knowledge of the personal psychological parameters of a BCI user can help in the development of individual training and preparation methods before operating neural interfaces.
Why is it necessary to imagine movements and work with neural interfaces? How can this help people with movement disorders? Let's look at these questions using the example of the two most common causes of movement disorders - stroke and spinal cord injury.
Mechanisms of neuroplasticity
During a stroke, an acute disruption of the blood supply to the brain occurs (either as a result of blockage of a vessel by a blood clot - ischemic stroke, or as a result of hemorrhage - hemorrhagic). Since, along with the blood, everything that they need for life ceases to flow to the neurons, the areas of the brain where blood circulation has stopped die off. And if these are areas responsible for motor activity - for example, the motor cortex, then the patient experiences hemiparesis, decreased muscle strength on one side of the body, or hemiplegia, complete paralysis of half the body.
The restoration of motor function is carried out mainly due to the mechanisms of neuroplasticity - the ability of the brain to change under the influence of experience: to establish new connections between neurons, destroy old and unnecessary ones, and restore those lost after damage. These processes involve not only neurons, but also neuroglial cells, as well as the vascular system [17]. The activity of synapses and their number also change [18]. To activate these mechanisms, motor rehabilitation is used in medicine. However, in patients with paralysis or a high degree of paresis, the implementation of real movements is impossible, so they resort to training with a BCI based on the imagination of movements. When imagining movements, the same areas of the brain are activated that are also involved in preparing a real action and in its execution, as a result of which such neurorehabilitation becomes real [19].
Thanks to such rehabilitation training, neurons around the damaged area undergo restructuring: the volume of gray matter in the motor zone of the brain increases, and neighboring areas take on lost functions [20]. The motor areas of the undamaged hemisphere are also involved in this process.
The effectiveness of these exercises can be increased through the use of biofeedback - visual or tactile - when the patient sees on a monitor screen how well he is completing a task (imagining the movement of a limb), or when he feels vibration from a special device when he successfully completes a task.
There are also systems that provide motor feedback: for example, when a person imagines moving his right leg, setting it in motion with a special mechanism. The Biokin system (Kosima LLC), developed under the leadership of Yu.P. Gerasimenko, works on this principle. (Institute of Physiology named after I.P. Pavlov RAS) (Fig. 4) [21]. It includes feedback, functional electrical stimulation (FES) and transcutaneous electrical stimulation of the spinal cord (TESCS), which makes it a highly effective tool in the field of neurorehabilitation of the lower extremities [22].
Figure 4. Biokine. A complex for neurorehabilitation of the lower extremities, based on the use of a BCI with feedback, FES (functional electrical stimulation) and tESCS (transcutaneous electrical stimulation of the spinal cord).
Biokin website
Such systems make it possible to close the sensorimotor loop: from the efferent (outgoing) signal of motor activity sent by the brain to the afferent (incoming) signal of sensory feedback (Fig. 5) [23].
Figure 5. Neuroplasticity induced by motor imagery-based BCI use. When the motor areas of the cortex are damaged, real movement becomes impossible, so to activate the processes of neuroplasticity, only the possibility of imagining movements remains. The use of a BCI with visual and tactile feedback enhances these processes.
adapted from [23]
This rehabilitation mechanism can be explained by the concept of Hebbian plasticity: with the simultaneous activation of two neurons connected to each other, their synaptic interaction increases, which leads to more reliable contact between them (Fig. 6). If we assume that signal transmission from the motor cortex to the limb muscles has been disrupted due to stroke or injury, then simultaneous activation of the sensory and motor cortices may enhance previously inactive connections between neurons through plasticity and thus lead to restoration of motor function of the limbs [ 24].
Figure 6. Hebbian plasticity mechanism. Strengthening the synaptic interaction between two neurons occurs due to repeated stimulation of the postsynaptic cell by the presynaptic cell.
adapted from ""
Figure 7. Formation of new neural connections in the area of spinal cord injury (SCI).
adapted from [25]
When restoring motor function after spinal cord injury, the same mechanisms of neuroplasticity are involved. With such damage, some of the nerve fibers, including motor ones, are interrupted, which causes paralysis of the limbs, while some retain their integrity. Due to this, during neurorehabilitation, it is possible to activate neuroplasticity processes: intact fibers form synaptic connections with motor neurons (motoneurons), which, in turn, transmit a signal to the muscles (Fig. 7) [25].
To increase the effectiveness of neurorehabilitation using BCIs, functional electrical muscle stimulation (FES) is often additionally used. It provides contraction of a muscle at the moment when the user imagines a movement involving this muscle (Fig. [26]. This leads to increased neuroplasticity via the Hebbian mechanism: there is a simultaneous activation of the motor areas of the brain, which transmit signals to the motor neurons of the spinal cord, and sensory neurons, activated by a muscle contracting under the influence of FES, which closes the sensorimotor loop.
It provides contraction of a muscle at the moment when the user imagines a movement involving this muscle (Fig. [26]. This leads to increased neuroplasticity via the Hebbian mechanism: there is a simultaneous activation of the motor areas of the brain, which transmit signals to the motor neurons of the spinal cord, and sensory neurons, activated by a muscle contracting under the influence of FES, which closes the sensorimotor loop.
Figure 8. IMC-FES system. When imagining movements, a signal from the motor cortex is processed by a computer (PC) and transmitted to a functional electrical stimulation (FES) device, which causes contraction of the corresponding muscle. The signal from the muscle is then transmitted to the sensory cortex, providing feedback.
adapted from [26]
Electrostimulation of the spinal cord
In recent years, electrical stimulation (ESS) has shown great effectiveness in neurorehabilitation after spinal cord injury. The spinal cord has two thickenings: in the neck and lumbar region, which corresponds to the place where the roots of motor neurons of the upper and lower extremities exit from them. In the lumbar enlargement of the spinal cord there are specialized neural networks that ensure the automatic process of stepping (stepping movement generators, GSM). In other words, if you apply electrodes that deliver a current of a certain amplitude and frequency to the dura mater of the spinal cord at the site of the lumbar enlargement, you can induce involuntary walking movements even in people with paraplegia [27]. However, this method requires surgery, so there is a risk of developing postoperative complications.
Currently, transcutaneous electrical stimulation of the spinal cord (TESCS) is considered the safest and most painless. In video 1 (Edgerton Lab, University of California) you can see how involuntary stepping movements of the legs are caused when the patient is in a relaxed position, with his legs suspended on a swing frame [28].
Video 1. Involuntary walking during transcutaneous electrical stimulation of the spinal cord.
Edgerton Lab, University of California
When using TECS, the question of the correct location of the stimulating electrodes arises. If, when installing invasive electrodes during surgery, the segments and roots of the spinal cord are clearly visible, then when installing cutaneous electrodes, it may be difficult to find the desired area. This problem is solved by applying single impulses to the electrode and recording reflex muscle responses - after all, each segment of the spinal cord corresponds to strictly defined muscle groups.
There is also the problem of insufficient amplitude of the impulses sent - due to degenerative processes in the case of spinal cord damage, a large amplitude of stimulation is required to obtain the desired response. However, this can result in burns. Our laboratory has created an optimal device for non-invasive electrical stimulation of the spinal cord [29].
In addition, a system was developed that detects the phases of the walking cycle online and stimulates the spinal cord according to these phases [30]. While walking, different muscles tense at different moments, and joints bend at certain angles, which can be recorded with special devices - accelerometers and gyroscopes. Both legs move in a coordinated manner, and based on the position of one leg, the position of the other can be predicted. The principle of operation of the system is as follows: for a patient with hemiparesis, motion sensors are applied to the healthy leg, which transmit a signal to the TECS device. It, in turn, stimulates at certain points in time groups of spinal cord motor neurons responsible for the movement of the flexor and extensor muscles of the leg, which helps normalize walking and restore movement of the affected limb.
Application
TMS is used in three main areas: 2930
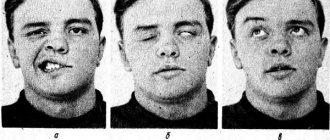
- neurorehabilitation after traumatic brain injury, stroke and brain surgery, in particular for the correction of residual neurological disorders (aphasia, apraxia, dysarthria, agraphia, alexia)
- treatment of neurological and mental diseases
- diagnosis of neuromuscular conduction disorders
TMS is often used to correct neurodevelopmental disorders in children:
- childhood aphasia, alalia, dysarthria, logoneurosis, delayed speech development
- impaired mental function
- autism spectrum disorder
- cerebral palsy
Advances in modern neurorehabilitation
The largest study in the field of neurorehabilitation using a BCI based on motor imagery is the work of Donati et al., published in Nature in 2021 [31]. This study involved eight people with paraplegia caused by spinal cord injury. A special rehabilitation system was developed for them, including six stages of increasing complexity, and about 255 (!) sessions were conducted with each patient during the year.
The first stage included a deep immersion in a virtual reality environment, during which the subject controlled the movement of his avatar (computer character), imagining the movement of the lower limbs in a sitting position. Then the patient did the same, only in a standing position, leaning on a special table. During the third stage, training took place on a treadmill: the subject walked using a device that supports body weight (Lokomat). At the fourth stage, the legs moved in the air, and not on the treadmill. In the fifth stage, the patient trained on a treadmill using a robotic limb support system controlled by a BCI. And at the final stage, the subject walked in an exoskeleton controlled by a BCI: the exoskeleton took a step when the person imagined the movement of the corresponding leg. During all trainings, subjects received tactile feedback - a vibration that was applied to the forearm when a virtual or robotic leg on the same side touched the ground. You can see the experiment diagram in Figure 9, and the rehabilitation process itself in Video 2.
Figure 9. Scheme of the experiment, which includes six stages: 1 - BCI + virtual reality (VR) in a sitting position; 2 — BCI + VR in a standing position; 3 — walking on a treadmill while supporting body weight; 4 - movement of legs in the air; 5 — walking on a treadmill using a robotic system controlled by a BCI; 6 — walking in an exoskeleton controlled by a BCI. Designations: EEG - electroencephalography; EMG - electromyography, which records muscle activity; Tact. - tactile feedback.
[31]
Video 2. The process of conducting the experiment.
[31]
After 12 months of training using this system, all eight patients had improved tactile sensation scores and regained free control of key muscles of the lower extremities. As a result, noticeable progress was seen in their ability to walk. Many patients were able to walk with the help of assistive devices. In addition, all patients showed a significant increase in emotional stability and assessment of quality of life, as well as a decrease in the level of depression and an increase in self-esteem. The condition of the skin and the function of the digestive system have improved, which is apparently associated with the normalization of the activity of the sympathetic and parasympathetic systems. The fact is that along the spine there are nodes of the autonomic nervous system, which regulates the functioning of the internal organs. They are damaged when the spinal cord is injured, which causes disruption of the digestive system, which in turn affects the condition of the skin through the release of signaling molecules, including pro-inflammatory ones [32], [33].
Neurological recovery was associated with plasticity mechanisms at both the spinal cord and sensorimotor cortical levels. Cortical and spinal plasticity alters neural connections in the surviving region of the spinal cord through motor and sensory connections (Figure 10).
Figure 10. Plasticity of the spinal cord (SC) and cerebral cortex through motor (red) and sensory (blue) connections.
adapted from [31]
Carrying out TKES therapy
No preparation is required before performing TCES. Before starting the procedure, the patient must remove piercings and other jewelry. Electrotherapy is usually carried out in a lying position, but in some cases it is allowed to sit.
The doctor will attach the electrodes to the head, adjust the current parameters and duration of the procedure. The first session is carried out at minimal electric current values. On the second visit, the tension increases. If the patient feels discomfort, the procedure is stopped and the parameters are selected again. After completing the session, it is not recommended to eat for two hours.
One session lasts up to 20 minutes, but the time can be increased in cases where severe pain needs to be relieved. The course of electrotherapy is usually 15 sessions.
Transcranial electrical brain stimulation is often prescribed in conjunction with other treatments to increase their effectiveness.