Hypertension - causes and mechanism of development
Hypertension is a chronic disease in which there is a frequent increase in blood pressure. If normally it is 120/80 mm. rt. Art., then at 140/90 mm. rt. Art. The initial stage of the disease has already been diagnosed. In some patients, only the systolic (upper) pressure increases, but the lower (diastolic) pressure may also increase along with it. The diagnosis is made based on the results of measuring blood pressure in different physiological states: during rest and after exercise.
Blood pressure increases due to dysregulation, vascular spasms and other factors. In most patients, hypertension is primary - it manifests itself as an independent disease, and a hereditary predisposition can also be observed. In other cases, the disease is caused by long-term use of certain groups of drugs, including hormonal drugs, kidney disease and metabolic disorders. Thus, secondary (symptomatic) hypertension is diagnosed, which also often causes headaches and high blood pressure.
Doctors identify risk factors that can provoke attacks of hypertension, as well as aggravate the course of the disease in the early stages. These include:
- overweight – up to 85% of patients diagnosed with chronic hypertension suffer from obesity;
- smoking - this bad habit reduces the ability of blood vessels to respond to changes in blood pressure, and also provokes ischemia (oxygen starvation) of the myocardium;
- insufficient physical activity, sedentary lifestyle, working behind a monitor;
- stressful situations that activate the sympathetic nervous system and lead to a persistent increase in blood pressure;
- patient's age.
According to statistics, in young people hypertension is secondary and is associated with a person’s lifestyle. High blood pressure and headaches are often triggered by bad habits, stress and poor diet. At the age of 40 years and older, sclerotization of the arteries is diagnosed - a decrease in their strength and elasticity as a result of the growth of connective tissue. This process is irreversible, but can be reversed by taking medications, adequate exercise and a therapeutic diet.
Expert opinion
Alexander Yuryevich Shishonin notes: in order to relieve headaches due to hypertension, it is first necessary to correct the pressure. It is best to do this non-medically.
Information on how to lower blood pressure is presented on the website
of the Club of Former Hypertensives
. Those who have not yet become a member of the club can do so completely free of charge. The site provides a lot of useful and interesting information from the field of cardiology and orthopedics.
Shishonin also draws attention to the fact that headaches occur in only 50% of hypertensive patients. In the other half, high blood pressure is not accompanied by headaches. Why does cephalalgia occur? The answer is simple. The fact is that with high pressure, the blood flow to the head increases, and the outflow, in turn, weakens. This is most likely due to pinched veins that carry blood away from the brain.
Important.
If a person has increased intracranial pressure, then no painkillers will help him.
If a hypertensive person has a tonometer, for example, shows 180/100 mm. rt. Art., then you need to keep in mind that intracranial pressure can be 1.5-2 times higher than blood pressure. This is due to impaired outflow of venous blood from the head.
Note.
It is worth noting that headache with arterial hypertension is not the only sign of the disease. During its course, other symptoms of malaise are observed. Having identified signs of hypertension, you should not delay a visit to the doctor. Only an experienced specialist will be able to find out the true reason for their appearance.
What should you do if a headache occurs due to hypertension?
Dr. Shishonin recommends that hypertensive patients apply a cold compress to the back of the head if cephalgia occurs. In addition, the occipital-cervical area can be wiped with pieces of ice for 1.5-2 minutes. Then the treatment area must be wiped dry with a towel.
The above procedures lead to a reflex expansion of blood vessels and blood outflow from the brain. Thus, intracranial pressure returns to normal.
Note.
It is very important not to overdo the use of ice, since with short-term exposure to tissue, cold (ice) dilates blood vessels. But if ice is used for more than 5 minutes, it will lead to vasoconstriction. This should not be allowed, as the patient’s condition will only worsen.
Can I get a headache when taking antihypertensive pills?
The specialists at Doctor Shishonin’s Clinic are vehement opponents of the use of pills for hypertension. The head physician of a medical institution notes that if a patient, while using antihypertensive drugs, somehow copes with blood pressure and still has a headache, then this is a direct confirmation that he has problems with the venous outflow of blood.
To normalize arterial and intracranial pressure, as well as improve venous outflow, you can use cold compresses on the occipital region and perform a simple set of exercises for the neck, developed by Dr. Shishonin.
Advice.
If you take pills for blood pressure, and it has returned to normal, but your head continues to hurt, it means they are not helping you. Give up this method of treatment and look for another, more qualified doctor.
Features of headaches in hypertension
Pressure headaches are the result of impaired vascular ability to adapt to external and internal changes. Blood presses on the inner walls of blood vessels, irritating the receptors. These signals travel to the brain, where they are converted and cause pain. In advanced stages of the disease, this condition is accompanied by increased fluid pressure inside the skull, which also causes severe headaches.
Chronic hypertension manifests itself as alternating periods of rest and increased blood pressure. During attacks, the patient has a very headache, the pressure in the arteries rises sharply. This can be caused by a number of factors:
- physical or mental fatigue - in this case, to normalize blood pressure indicators, it is enough to pay attention to proper rest;
- changes in weather conditions - a sharp increase in atmospheric pressure often provokes attacks of hypertension, which can be eliminated with rest and medications;
- abnormal physical activity – causes acceleration of blood flow and heart rate, which is dangerous if the elasticity of the blood vessels is insufficient;
- pregnancy – hormonal changes cause attacks of hypertension;
- unhealthy diet – consuming excess amounts of salt and spices leads to impaired removal of fluid from the body, swelling and an increase in the volume of circulating blood.
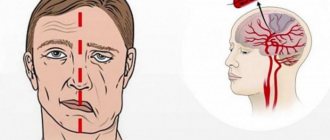
Headache with high blood pressure has its own characteristics. It can be caused by various reasons, so it is usually classified into vascular, liquor, ischemic and neuralgic. In most patients, it spreads to the temples and back of the head. It is sharp, pressing, and leads to impaired concentration. With a sharp increase in pressure, hearing and vision deterioration and fainting may occur.
Vascular pain
The main cause of vascular syndrome is a violation of the outflow of fluid from the brain. Arteries and veins fill with blood, tissue swelling is observed. This leads to irritation of nerve receptors and an increase in pain. The pain in the head with pressure is pressing, the pulsation of blood vessels is felt. It intensifies if you lower your head down, as well as with sudden movements, coughing and sneezing.
Liquor syndrome
Another reason why headaches occur with pressure is a violation of the movement of cerebrospinal fluid. This is a special fluid that is found in the brain and spinal cord. It performs a shock-absorbing function, protects soft tissues from compression and regulates pressure in the skull. Normally, it circulates constantly, but in case of vascular pathologies, heart disease and chronic hypertension, it is retained in the brain. This process is accompanied by aching, bursting pain, which intensifies during sudden movements of the head. The process is dangerous because the cerebrospinal fluid also contains nutrients for nerve cells. If fluid circulation is not stimulated, this can lead to cerebral ischemia and trigger a stroke.
Ischemic pain syndrome
The cause of headaches and pressure can be spasm of blood vessels. This leads to insufficient oxygen and nutrients reaching certain areas of the brain. The patient also experiences hearing and vision impairment, dizziness, a sharp increase in blood pressure and weakness. Attacks are relieved by using antispasmodics; rest and means to normalize the functioning of the nervous system are also useful.
Neuralgic pain
Increased pressure inside the skull affects all nerve structures. Excess cerebrospinal fluid leads to compression of the trigeminal nerve, which is responsible for the innervation of the skin and muscles of the face. The pain in this case is sharp, throbbing, concentrated in the facial part. It worsens during movement, bending and turning the head.
Additional symptoms
It is important for a patient with chronic hypertension to know how a headache occurs with high blood pressure. It has several features that indicate a simultaneous increase in blood pressure:
- headache spreads to the back of the head and temporal parts of the head;
- the nature of the pain is pressing, there is a feeling of expansion of the contents of the skull;
- filling of blood vessels leads to redness of the skin and mucous membranes, minor hemorrhages are possible due to damage to the walls of the capillaries;
- ringing or noise in the ears is a typical sign of high blood pressure;
- blurred vision, the appearance of various hallucinations in the form of black dots or circles before the eyes;
- weakness, fatigue, decreased performance;
- dizziness, nausea;
- a sharp increase in blood pressure is the cause of fainting.
If your head starts to hurt severely, you need to measure your blood pressure. The procedure can be carried out independently, using a tonometer. This device should be in every home medicine cabinet, even if there are no patients with chronic hypertension in the family. Headaches go away after blood flow is restored and pressure is normalized, including with individually selected medications.
Dizziness due to hypertension
Professor Olga Dmitrievna Ostroumova gave a lecture “Dizziness with arterial hypertension: is antihypertensive therapy sufficient?”
00:00
Drapkina Oksana Mikhailovna , executive director of the Internet Session, secretary of the interdepartmental council on therapy of the Russian Academy of Medical Sciences:
— Now we are moving on to a new, very interesting section “Dizziness in the practice of a therapist.”
Section consisting of one lecturer and discussion. Professor Ostroumova Olga Dmitrievna. The lecture is called “Dizziness with arterial hypertension: is antihypertensive therapy sufficient?”
Olga Dmitrievna Ostroumova , professor:
— Good afternoon, dear colleagues.
We will talk to you about dizziness. Dizziness is at least one of the most common complaints that patients present (if not the most common complaint).
If you look at any manuals on internal medicine (and not only internal medicine), the description of the clinical picture of almost every disease will contain dizziness. It turns out that the number of diseases that cause dizziness runs into the thousands, if not tens of thousands.
But dizziness is not always correctly diagnosed. It is very difficult to treat it. This is the kind of complaint that almost always remains the last. Other complaints are already going away, but the patient keeps complaining and complaining about dizziness. It feels like this is a saving straw.
Issues of polypharmacy. In order to relieve dizziness, doctors use many medications off-label. In general, the problem, at first glance, is simple, but it turns out to be very complex.
The main problem is that what the patient understands by dizziness, what the doctor understands by dizziness and the formal definition of dizziness are completely different things.
In fact, the patient uses the word “dizziness” most often where it does not exist. He has “lightheadedness”, weakness, darkening of the eyes, and a faint state. The complex of sensations preceding fainting is called the beautiful word “lipothymia”. This is either a decrease in cerebral blood flow or a change in the direction of reducing its supply of oxygen and glucose.
This happens with orthostatic hypotension, with hypoglycemia and a number of diseases of the cardiovascular system (CVS): aortic stenosis, sick sinus syndrome, tachyatrythmia.
02:41
By dizziness, the patient very often understands instability, unsteadiness. When walking, he staggers and throws, especially when turning, changing the pace of walking, or when initiating walking. In particular, this happens with damage to the cerebellum, with peripheral neuropathy, and with a number of diseases of the spinal cord.
Vague sensations that are difficult for the patient to describe: a feeling of heaviness, intoxication, discomfort inside the head. The patient also uses the word “dizziness” very often. In such a situation, most often we will talk about psychogenic dizziness (depression, phobia, anxiety). But not only this, of course. These are the most common options.
The first moment when the patient utters this word, you must try very carefully, with leading questions, to understand what complex of sensations is bothering him. Is it really dizziness?
True dizziness is the illusion of movement of surrounding people or objects around a person. Or, conversely, a person around people or objects. This is understood as true dizziness.
Accordingly, all diagnostic search algorithms, which are described in various manuals and monographs, relate to true dizziness. Once again, as taught in propaedeutics. Very thorough history taking. Try to understand, I emphasize again, with leading questions, what kind of complex of sensations the patient has, whether this is really true dizziness.
Believe me, most likely it will not be true dizziness. Further, based on the complex of sensations, the diagnostic search will go in completely different directions, completely inconsistent with the algorithm for true dizziness.
Our task is to talk about true vertigo. If this is really dizziness, if we completely simplify it without harming the patient, then we distinguish between vestibular dizziness (true, which is associated with the vestibular apparatus) and non-vestibular, that is, beyond it.
Vestibular vertigo. Vestibular apparatus. What is it, what are the options. The first is peripheral (damage to the labyrinth). The second is intermediate (vestibular nerve, transmission of impulses from receptors to the brain). Finally, the central one is where impulses about the position of our body in space come (this is the central nervous system).
05:54
Arterial hypertension is almost the most common complaint of dizziness among patients. Moreover, both before the start of antihypertensive therapy and during it. Including with formal stabilization of blood pressure, when we reach target numbers. It seems that this complaint haunts both patients and doctors.
If you look at whether these are really interconnected things, it turns out that, most likely, according to available data, arterial hypertension itself is not the cause of dizziness. We need to look for other reasons. For now, examine not the disease, but the patient, then treat.
We have already agreed that dizziness is a strictly defined thing - the illusion of the movement of objects around a person or, conversely, a person around objects or other people. The most common cause of true present dizziness in patients with arterial hypertension coincides with that in the population.
Relatively speaking, since hypertension occurs often in older people (more than 80%), the most common cause of true dizziness that exists in the population is involuntarily transferred to this population of patients with hypertension. This is benign paroxysmal positional vertigo. We will return to it later.
The most common cause of non-systemic (non-vestibular) dizziness is psychogenic dizziness. We will not comment on this.
Much more often, it is not hypertension that leads to dizziness, but, on the contrary, an excessive decrease in pressure. I would say, not even so much in terms of numbers (although this also occurs, they reduced the millimeters of mercury too much), but rather would focus your attention on the excessively rapid decrease in blood pressure. Pace, pace and more pace. Even in a state of hypertensive crisis.
Of course, if there is concomitant diabetes mellitus, this is hypoglycemia, rhythm and conduction disturbances, which are partly associated with hypertension, if there is myocardial hypertrophy. But very often with concomitant cardiovascular diseases (CVD) in the patient.
Of course, orthostatic reactions. They generally occur with arterial hypertension. But much more often in elderly hypertensive patients and when arterial hypertension is combined with diabetes mellitus. They happen without treatment. One of the features of hypertension in the elderly is an increase in orthostatic reactions.
Some antihypertensive drugs cause orthostatic hypotension and collapse as side effects. These are β-blockers. We rarely use these drugs to treat hypertension. But now these drugs are gaining popularity among urologists. Very often we began to encounter this indirectly.
09:29
In my opinion, extremely indicative and one of the fundamental works is the work carried out under the guidance of Professor V. A. Parfenov. This is a professor at the Department of Nervous Diseases of the First Moscow Medical University. The department is headed by Academician Yakhno. He deals with this problem a lot.
A very interesting, carefully executed study. 60 hypertensive patients were taken with a complaint of dizziness. The vast majority of situations (80%, four out of five patients) – nothing was found in the patients at all during the most thorough examination. There are no somatic or neurological disorders.
Thus, the first assumption that needs to be confirmed is psychogenic dizziness (anxiety, depression, phobias, and so on).
17% – diseases of the peripheral part of the vestibular apparatus (benign paroxysmal positional vertigo or vestibular neuronitis). We'll talk about it a little.
A most thorough examination revealed a tumor of the cerebellar angle in one patient, and migraine in one patient. One patient had AV block. He was given a pacemaker, after which the dizziness disappeared.
11:03
None of the patients showed a connection between dizziness and increased blood pressure.
Let’s just say a few words about this peripheral dizziness. True dizziness is a defeat of the labyrinth. Peripheral cause, vestibulatory apparatus.
There are also several reasons for dizziness. But we are internists, not specialists in ENT diseases and not neurologists. A few words about benign paroxysmal positional vertigo (the most common cause of dizziness, in the general population, or in a patient with arterial hypertension. After psychogenic).
How does this dizziness manifest itself? Survey, survey and survey again. I won’t tell you anything new since you completed the propaedeutics course. 50% of the success of a diagnosis is a correctly collected analysis and complaints.
Benign paroxysmal positional vertigo (BPPV) is a short, no more than a minute, attack of systemic vertigo that occurs only with a certain position of the head. Most often in a lying position.
A single attack or a series of attacks at the slightest movement of the head. When you interview, the patient paints approximately this picture for you. Despite the extreme lack of time, do not forget to ask leading questions.
There are no neurological or any other symptoms; with repeated provocation of attacks, their severity decreases.
The presence of freely moving particles in the semicircular canals is the most common cause of dizziness.
There are the simplest tests for diagnosing it, which every internist can master. Treatment consists of special exercises, the effectiveness of which is up to 90%. Usually, drug treatment is not even required.
How to be. Of course, the main treatment should be aimed at eliminating the causes that caused dizziness. Treatment of dizziness is a complex treatment. No matter how safe it may seem (when almost everyone has a symptom, it is involuntarily easy to relate to it), we know how difficult it is to treat. The drugs must be used as a complex.
13:59
We have the drug “Betahistine” - an analogue of histamine. Histamine receptors are found in different organs. I want to pay particular attention to the H3 receptors that have been found in the cerebral cortex of rats. Accordingly, high histamine levels cause negative feedback and decreased histamine release.
Histamine receptors are located not only in the central nervous system (CNS), but also in the vestibular apparatus. The vestibular nuclei are very rich in histamine receptors.
Histamine is a very effective remedy in the treatment of dizziness and Meniere's disease, for example. But it is administered intravenously. It has a number of side effects. I think you represent them perfectly. I won't repeat myself. It is obviously unrealistic to treat patients with dizziness with histamine.
The corresponding searches were underway. Betahistine was created. A major study has begun. The drug has been used for quite a long time.
How it affects different types of receptors. Basically, it acts on the third type of receptors (H3 receptors). A powerful antagonist. Doesn't work on H2 at all. On H1 it is a very weak agonist. This action can also be neglected.
This immediately results in a very good safety profile. Low incidence of side effects. It has no effect on other types of receptors (non-histamine).
The drug that I think you know, Betaserc, shows a complex mechanism of action. It improves regional blood flow in the inner ear area. Normalizes the excitation of peripheral receptors. Normalizes the process of excitation in the area of the vestibular nuclei of the brain stem. Quite a wide range of mechanisms of action.
16:10
Appropriate placebo-controlled studies were conducted, where it was shown that Betaserc was significantly different from placebo. It reduces the frequency of dizziness attacks. It also differs from placebo in reducing dizziness severity and duration.
I think that you all have your own experience with this drug. For the sake of order, we talked about how it differs from placebo. Patients of this kind are very susceptible to placebo effects. We have no doubt about the effectiveness of Betaserk.
Let me very briefly recall the indications: treatment and prevention of vestibular vertigo of various origins, as well as a syndrome including dizziness and headache, tinnitus, progressive hearing loss, nausea and vomiting, Meniere's disease and syndrome.
The only contraindication is hypersensitivity to any of the components of the drug.
Like the vast majority of drugs, Betaserc has a dose-dependent effect, including in the treatment of dizziness. The most effective dose is 48 mg/day.
The drug is very good for the speed of onset of effect. Maybe not completely until the dizziness completely disappears, but it is noticeable. Almost 80% (that's four out of five patients) feel either a complete disappearance of dizziness (depending on the severity) or a decrease in the severity and frequency of attacks. Almost everyone else feels the effect on the second or third day. It is extremely rare that the effect develops during the first week. Basically, the drug works on the first day or in the first days.
Recently a new dosage has appeared - 24 mg. Taken twice a day. There is no need to take the daily dose. The lower the frequency of administration, the better the patient’s adherence to therapy. Accordingly, the effectiveness of treatment is higher. There are economic benefits.
We weren’t lazy, we did the math. It turned out that the new dosage of 24 mg is 13% more economical than the dosage of 16 mg. In the old dosage of 8 mg, almost 50%.
The age-old and very difficult question: brand or generic. We will not go deeper into this painful topic. You understand that price should not come at the expense of quality.
In pharmacoeconomic studies there is such an indicator as “price-effectiveness” (the ratio of quality and price). Do we really gain something by paying less money? Or it will turn out to be “money down the drain.”
There was such a pharmacoeconomic study of a number of generics of the drug Betaserc. In short, the drugs Betaver, Vestibo, and so on have significant differences in clinical effectiveness.
Thus, in pharmacoeconomic terms, the drug “Betaserc” wins. It has proven to be most effective in relieving dizziness. There was better tolerance. Costs also indicate that among the three drugs studied, the original drug Betaserc turned out to be the most cost-effective due to its effectiveness. But, unfortunately, this is a very common reason.
This is what I wanted to discuss with you within the allotted time frame. I wish you to feel dizzy only from success.
20:29
First aid for high blood pressure
If you don't have medications on hand, and before consulting your doctor, there are a few steps you can take to lower your blood pressure. Also, these methods help relieve vascular spasm and restore cerebral blood flow. Doctors at the Clinical Brain Institute recommend following a number of simple steps:
- provide the patient with rest in a cool room;
- sufficient oxygen access - simple ventilation often helps to relieve pain, nausea and dizziness;
- massage of the neck and head is a way to relax the muscles and reduce their pressure on the blood vessels; you can do it yourself;
- a cool compress applied to the temples and soles of the feet.
Doctors advise limiting yourself to only those drugs that are indicated in the prescription. If they do not help, you should contact for a second consultation and adjust the list of medications. In addition, the patient should not independently increase the dosage of drugs to increase blood pressure and take additional drugs for a quick effect.
If there is no tonometer, what signs indicate high blood pressure?
Blood pressure may rise or fall during the day, returning to normal values. This is how our body reacts to various life circumstances: stress, anxiety, sports or relaxation. However, there are situations when the pressure rises sharply.
How can you tell if it has jumped if you don’t have a tonometer at hand? Is it just a headache that speaks to this?
Characteristic signs of high blood pressure
Let us immediately note that all of the following signs can be both a symptom of high blood pressure and other diseases. If you have encountered them more than once, they grow stronger and do not go away, you should definitely consult a doctor!
Headache
You can often hear that the main sign of high blood pressure is a sharp headache, usually in the back of the head (sometimes in the temples). However, it may not always occur. Hypertension is not just called the “silent killer.” The disease is asymptomatic for a very long time, which means that a person, without knowing it (unless, of course, he uses a tonometer from time to time), walks with high blood pressure. As a result, the body gradually adapts, and even consistently high values do not cause discomfort, including headaches.
- A person reacts with headaches only to changes in pressure, both in the case of a strong increase or decrease,
- If a person has consistently high values, for example, 160/100 mmHg. pillar, he doesn’t feel them. However, with an even greater increase in indicators and even with a decrease to standard values of 120/80 mm Hg. the person will feel bad.
Headache may also be a symptom of low blood pressure.
Memory impairment
High blood pressure affects memory and mental performance. Such people quickly get tired and tired. Due to high pressure, the small arteries of the brain suffer, and the blood supply to the brain is worse. This, in turn, alters normal brain function, leading to memory loss and other problems (such as stroke).
Deterioration of vision and the appearance of “floaters” before the eyes
With a sharp jump in blood pressure, vision can decrease and so-called black spots appear in the eyes. Many people attribute these symptoms to age-related changes or manifestations of other diseases.
When the pressure rises sharply, vascular spasm occurs, in which certain areas of the eye experience a lack of oxygen, which leads to the appearance of flickering “floaters”. When the indicators normalize, these symptoms disappear.
Increased heart rate
The heart rate changes (sometimes people describe the sensation as “heart pounding” or “heart pounding”). A rapid pulse, which can be easily felt when pressed lightly, indicates increased blood pressure.
Excessive sweating
If you do not suffer from hyperhidrosis, severe sweating may indicate a sudden increase in blood pressure. It is often accompanied by symptoms such as numbness of the hands, face, tongue, rapid pulse, shortness of breath, and pain in the heart. As a rule, when the pressure decreases to normal values, increased sweating goes away.
In addition, symptoms may appear associated with the reaction of the human vegetative-vascular system to a sharp rise in pressure:
- redness/pallor of the skin;
- frequent urination (every 5 minutes);
- acute diarrhea;
- feeling of temperature;
- nausea;
- hand trembling;
- wet and cold hands;
- noise in ears.
What to do if you don’t have a tonometer
Of course, only a tonometer can show exact values. However, in emergency cases, you can use the following method. You need to take a comfortable position, lean your back on the back of the chair, and relax. Then feel the pulse on your wrist and count the number of beats in 30 seconds. The result obtained must be multiplied by two. If the heart rate is less than or equal to 60, blood pressure is low, 60-80 beats per minute is normal, more than 80 is increased. In addition, if during the measurement you feel that the pulse is well felt, its rhythm is quite rapid, most likely your blood pressure is increased. The heart rate cannot be heard well, it is interrupted - it is below normal.
IMPORTANT! Without accurately measuring blood pressure with a tonometer, you should not take any medications or antihypertensive drugs.
Cardiologist V.M. Kravtsov
Contraindications for hypertension
Headache with hypertension has its own characteristics. To get rid of it, it is necessary to relax the vascular walls and cause their expansion, as well as stimulate the outflow of excess fluid. At home, it is prohibited to take the following measures to treat pain caused by increased blood pressure:
- be in a stuffy room;
- take a hot bath, visit a bathhouse or sauna;
- drink coffee or natural strong tea, which also contains high concentrations of caffeine;
- buy or drink alcoholic beverages.
It is important to understand that treatment tactics and first aid differ for high and low blood pressure. Before taking medications, you must use a tonometer, and then periodically monitor the readings. It is especially important to monitor them in case of vegetative-vascular dystonia, a chronic disease in which blood pressure periodically changes both up and down.
How to properly treat hypertension
The main task of treating arterial hypertension is to reduce the risk of developing vascular accidents as much as possible. To achieve this goal, existing negative factors should be eliminated and blood pressure stabilized within optimal values. The optimal blood pressure for most people with hypertension is less than 140/90 mmHg. Art. There is an exception to this rule: for elderly patients, the desired blood pressure is 140-150/90-95 mm Hg. Art. It should also be taken into account that achieving too low blood pressure values (less than 110\70 mm Hg) is not recommended, since hypotension increases the risk of vascular accidents. The treatment strategy for hypertension is determined by the degree of blood pressure increase and the level of risk of cardiovascular complications. It is believed that in case of arterial hypertension of the 1st degree and the absence of negative factors, treatment should begin with lifestyle correction and only if after several months the increase in blood pressure persists, drug therapy should be prescribed.
Corrective actions include :
- limiting the consumption of alcoholic beverages and quitting smoking;
- balanced diet (eating foods rich in potassium and magnesium, limiting table salt to 5 g/day, excluding fatty foods and marinades);
- normalization of weight (optimal body mass index – 25 kg/m2);
- rational physical activity (daily walking, running or swimming for at least half an hour a day).
For arterial hypertension of 2 and 3 degrees, drug therapy is prescribed immediately at any level of risk of complications. Also, drug therapy is mandatory in the presence of three or more risk factors for cardiovascular complications, regardless of the degree of hypertension.
Basic drugs for the treatment
include the following.
- Angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers are considered among the most effective antihypertensive drugs. They significantly improve the prognosis of patients with heart failure, prevent the formation of left ventricular hypertrophy and the development of chronic kidney pathology. These medications are contraindicated in pregnant women (they provoke the development of fetal defects), as well as in cases of stenosis (narrowing) of both renal arteries. Their significant drawback is the ability to provoke an obsessive dry cough, which makes patients unwilling to continue therapy.
- Calcium antagonists cause selective dilatation of peripheral vessels and significantly reduce the risk of stroke, thrombus formation and left ventricular hypertrophy. They have also been shown to reduce the bronchoconstrictor effect of histamine, which is why calcium antagonists are the preferred antihypertensive drugs for people with asthma or chronic obstructive pulmonary disease. However, some of them (with a predominant effect on the heart muscle) are contraindicated in cases of impaired intracardiac conduction such as 2-3 degree AV block, severe heart failure, and decreased myocardial contractility.
The use of beta-blockers, which reduce the frequency of contractions of the heart muscle, is most desirable when hypertension is combined with coronary heart disease and arrhythmias. Due to the specific effect on adrenergic receptors of the bronchi and heart, these medications are not recommended for patients with diabetes mellitus, bronchial asthma and intracardiac conduction disorders such as 2-3 degree AV block.
Other medications for the treatment of hypertension also include direct renin inhibitors, imidazoline receptor agonists, and alpha-blockers.
In accordance with federal recommendations for the treatment of arterial hypertension, if the risk of cardiovascular complications is low, treatment with one drug should be started, and only in the absence of the effect of single-component therapy, antihypertensive drugs of other groups should be added. People with blood pressure above 180\100 mm Hg. Art. and/or a high risk of complications, dual-component therapy should be initially recommended. The following combinations are rational: an ACE inhibitor or an aldosterone receptor antagonist with a diuretic or calcium antagonist (in older people); dihydroperidine calcium antagonist with a diuretic or -blocker (for ischemic heart disease, previous heart attack); - blocker with diuretic. Inappropriate combinations that increase the likelihood of undesirable effects include combinations of an adrenoblocker with verapamil or diltiazem, an ACE inhibitor and spironolactone, an adrenoblocker and an adrenoblocker. In some cases, when stabilization of blood pressure cannot be achieved using two drugs, a third one should be added. The following schemes are recommended:
- ACE inhibitor + dihydropyridine calcium channel blocker + -adrenergic blocker;
- ACE inhibitor + diuretic + -adrenoblocker;
- aldosterone receptor antagonist + diuretic + -adrenergic blocker.
Often people are unwilling to take a large number of tablets daily to treat hypertension, as a result of which they often stop the therapy they have started on their own, causing damage to their health.
To solve this problem, combination drugs were invented, combining two antihypertensive drugs in one tablet. These include “Enap N” (ACE inhibitor and diuretic), “Equator” (ACE inhibitor and calcium channel blocker), “Valz N” (diuretic and aldosterone receptor antagonist), “Lodoz” (adrenergic blocker and diuretic) etc.
Diagnostic methods
You can diagnose hypertension at home, if you have a working tonometer. However, the disease may have its own characteristics and occurs for various reasons. It is important to undergo a full examination to determine why your blood pressure is rising. This information will help you choose an effective treatment regimen, as well as prevent further development of the disease. After examining and measuring blood pressure, the doctor may prescribe the following diagnostic methods:
- MRI of the head is one of the most effective methods, which is used when there is a suspicion of increased intracranial pressure, the presence of neoplasms and foci of ischemia;
- Dopplerography of the vessels of the neck and head is an informative technique that involves studying blood flow using a contrast agent;
- clinical and biochemical blood tests - allow you to evaluate the chemical composition of the fluid and determine protein metabolism disorders;
- X-ray of the cervical spine - spondylosis, osteochondrosis and other diseases that lead to compression of blood vessels and increased blood pressure in them will be visible in the pictures.
The Clinical Brain Institute has all the conditions to undergo a complete examination for headaches and high blood pressure. To confirm the diagnosis, the patient will be offered consultations with specialists of a narrow and broad profile. This will allow you to comprehensively consider the disease and select treatment that will affect not only the symptoms, but also the cause of the disease.
Symptoms of hypertension and its treatment
There are 3 degrees of arterial hypertension:
- blood pressure value 140-159/90-99 mm Hg. – 1st degree;
- blood pressure value 160-179/100-109 mm Hg. – 2nd degree;
- blood pressure value from 180/110 and above mmHg. – 3rd degree.
The degree of hypertension determines other symptoms and methods of treatment. Frequent manifestations of hypertension include : dizziness, headache (in the temporal and occipital regions, pressing or pulsating), rapid heartbeat, nausea, flashing “spots” and dark circles before the eyes, tinnitus. These symptoms usually appear when blood pressure rises, but there are often cases when the disease is completely asymptomatic.
A long-term uncontrolled increase in blood pressure negatively affects the functioning of the body as a whole, but some organs are particularly susceptible to changes and are affected earlier than others. These are “target organs”, which include the heart, brain, kidneys, peripheral vessels and fundus vessels. Markers of their damage are: hypertrophy (thickening) of the left ventricle of the heart and impairment of its diastolic function (ability to relax), chronic heart failure, myocardial infarction; progression of the atherosclerotic process; stroke, hypertensive encephalopathy; angiopathy of the fundus vessels, accompanied by visual impairment; glomerulosclerosis of the kidneys.
The involvement of “target organs” in the pathological process determines the stages of hypertension:
- Stage I – there is no damage to “target organs”;
- Stage II - single or multiple target organ damage was diagnosed, but there was no myocardial infarction (AMI), stroke and there was no chronic kidney disease.
- Stage III – signs of chronic kidney disease, previous AMI and/or stroke.
There are some risk factors, in the presence of which the possibility of vascular accidents increases significantly, in particular:
- male gender;
- age (over 55 years for men and over 65 years for women);
- smoking;
- metabolic disorders of cholesterol and its derivative fractions;
- disorders of carbohydrate metabolism (diabetes mellitus, impaired carbohydrate tolerance);
- violation of fat metabolism (body mass index above 30 kg/m2);
- complicated heredity (cardiological and vascular diseases in blood relatives);
- detection of left ventricular hypertrophy;
- generalized atherosclerosis;
- presence of chronic kidney disease;
- coronary heart disease and severe chronic heart failure;
- previous heart attacks and/or strokes.
The higher the blood pressure numbers and the more negative factors the patient has, the higher the risk of vascular accidents. If blood pressure remains at 159\99 mm Hg. or less, and there are no negative factors, the risk of complications is considered low. With the above blood pressure values in combination with one or two negative factors, and also if blood pressure remains at the level of 160-179\100-109 mm Hg. Art. and there are no negative factors - the risk is average. With grade 3 hypertension, the risk of complications is considered high without taking into account the presence of negative factors. If a person suffers from stage 4 chronic kidney disease, or has been diagnosed with target organ involvement, or has already suffered a heart attack or stroke, then the risk of cardiovascular complications is regarded as extremely high, regardless of the degree of hypertension.
Treatment of headaches with high blood pressure
An acute attack of headache can be relieved with analgesic drugs. These include Citramon, Analgin and other products that are in the simplest home medicine cabinet. However, to control blood pressure levels, an individual treatment regimen is prescribed. It depends on the cause and stage of hypertension, the patient’s age, the presence of concomitant diseases and other factors. It may include drugs from different groups.
- Selective beta blockers are drugs that reduce the heart rate, which leads to a decrease in pressure on the internal walls of blood vessels. This group includes Bisoprolol, Metoprolol and their analogues.
- Calcium channel blockers (Cordafen, Felodipine) are often prescribed for the complex treatment of hypertension because they have no side effects. They prevent the penetration of excess calcium ions into the walls of blood vessels. This causes them to expand and relax, as well as slowing down the rapid heartbeat.
- Medicines from the nitrate group (Nitrong, Kardiket) are used for significant increases in blood pressure. They will help reduce it in the short term, but are not suitable for long-term use.
- Alpha blockers (Phentolamine) are drugs that quickly relieve vascular spasms and restore blood movement through the arteries.
- Diuretics (Furosemide, Lazex) are diuretics. They are suitable for taking in a course and are used in the treatment of chronic hypertension. These drugs stimulate the removal of excess fluid and control the volume of circulating blood.
- Antispasmodics are a group of drugs that quickly relieve vascular spasms. This group includes No-Shpa, Spazmalgon and other drugs that are suitable for eliminating headaches of any origin.
If your blood pressure often rises and your head hurts, this requires complex treatment. Doctors at the Clinical Institute of the Brain will select the optimal regimen, which will include only the necessary drugs. They should be taken at home and blood pressure should be measured periodically. In addition, doctors will prescribe a therapeutic diet with a reduced amount of salt, fatty foods and processed foods. To treat hypertension, it is also necessary to give up bad habits, smoking and drinking alcohol.
Diagnosis and treatment of headaches in patients with arterial hypertension
G
tin pain (cephalalgia) in patients with arterial hypertension is usually regarded as an increase in blood pressure (BP). However, the role of arterial hypertension in the genesis of headaches has been proven only in some clinical situations [5,6].
In these cases, antihypertensive therapy is of key importance in treatment, which, as a rule, leads to the disappearance of headaches.
If there are repeated attacks of headache against the background of a significant increase in blood pressure, it is necessary to exclude pheochromocytoma
, which is characterized by:
- short-term (10–15 minutes) attacks of bilateral headache,
- sweating, nausea, trembling during an attack,
- high levels of catecholamines in the urine during an attack.
In most patients with arterial hypertension, headache is caused by concomitant diseases [5,6].
In total, about 50 diseases are known in which headache can be the main and even the only symptom. In 1988, a group of international experts [6] proposed a classification of headaches, in which headache due to increased blood pressure was classified as pain of vascular origin. Classification of headaches
1. Migraine.
1. Migraine.
2. Tension headaches.
3. Beam (cluster) headache and chronic paroxysmal hemicrania.
4. Headaches not associated with structural damage.
5. Headache due to head injury.
6. Headache due to vascular diseases.
7. Headache due to intracranial non-vascular diseases.
8. Headache due to taking medications or their withdrawal.
9. Headache due to extracerebral infections.
10. Headache due to metabolic disorders.
11. Headache or facial pain due to pathology of the skull, neck, eyes, ears, nose, paranasal sinuses, teeth of the mouth or other facial or cranial structures.
12. Cranial neuralgia, pain due to pathology of nerve trunks and referred pain.
13. Unclassifiable headache.
Patients with arterial hypertension and headaches that cannot be explained by increased blood pressure require examination to determine the causes of headaches and adequate treatment.
Correctly constructed active questioning largely solves the problem of diagnosis in a patient with headache [1,5,6].
It is necessary to clarify the characteristics of the headache:
1) How long does the headache last: hours, days or weeks (acute headache), months or years (chronic headache).
2) Duration of headache: is it constant or is it periodic? is it the duration and frequency of attacks?
3) Localization of headache: is it bilateral (diffuse), is it unilateral, is it frontal, parietal, temporal or occipital?
4) Character of the headache: is it throbbing, squeezing, bursting or dull?
5) Headache intensity: mild, moderate or severe?
6) Associated symptoms: nausea, vomiting, sound or photophobia, any other disorders?
7) Does the headache occur (or get worse): at night, in the morning, during the day or in the evening?
 What factors provoke or intensify headaches?
What factors provoke or intensify headaches?
9) What makes it easier (if taking medications, which ones)?
10) Are headache attacks preceded by: changes in emotional state, neurological disorders (changes in vision, numbness or weakness in the limbs, etc.)?
11) Did any of the patient’s relatives suffer from headaches? If so, what are the characteristics of their headaches?
12) Does the patient have conflict or stressful situations and is the appearance (or worsening) of headaches associated with them?
In most patients with arterial hypertension and headache, somatic and neurological examinations do not reveal signs of the disease causing cephalalgia, and the results of questioning indicate tension-type headache or migraine, so additional instrumental examination methods are not required. If, however, based on the history and/or examination results, doubts arise regarding the possibility of another neurological or somatic disease, then additional examination of the patient is necessary.
Subarachnoid hemorrhage must be excluded in case of sudden development of intense headache in patients with arterial hypertension. According to our data [2], in 3% of patients hospitalized by emergency medical care with a preliminary diagnosis of “hypertensive crisis”, subarachnoid hemorrhage is detected.
Before the widespread introduction of CT and MRI of the head into clinical practice, electroencephalography and echoencephaloscopy were the leading methods for examining a patient with headache, but now these methods have lost their former significance and do not completely exclude a neurological disease that can be detected with CT or MRI of the head [1,5 ,6]. Non-invasive examination of extra- and intracranial arteries (ultrasound Dopplerography, duplex scanning, transcranial Dopplerography) is of great importance in the diagnosis of stenosis and occlusion of the arteries, but in most cases they also do not allow us to clarify the cause of headache in a patient with arterial hypertension.
When a headache is suspected to be associated with a lesion of the cervical spine, a thorough manual and neuro-orthopedic examination is necessary, which can reveal the cervical nature of the headache. CT and MRI of the cervical spinal cord in such patients can identify intervertebral hernias or other pathology of the craniospinal region.
The majority of patients with mild to moderate arterial hypertension and suffering from persistent or recurrent headaches experience tension-type headaches [3].
Characteristic signs of tension headaches [1,5,6]:
- mild or moderate pain intensity,
- squeezing or squeezing (non-pulsating) nature of the pain,
- bilateral (diffuse) localization,
- absence or slight increase in pain during physical activity, walking up stairs,
- absence of nausea and vomiting,
- absence of a combination of fear of light and sound (only light or sound fear is possible).
Tension headaches (TTH) include episodic TTH (less than 15 days per month) and chronic TTH (15 days or more per month).
In some patients, tension headaches occur relatively rarely, for example, during a stressful situation or intense mental work, last several hours and go away on their own or after taking simple analgesics. In other patients, tension headaches are more frequent, their duration varies from hours to several days, but long “light” intervals without pain are characteristic. Finally, some patients experience headaches almost daily and in many cases for many years. When examining patients suffering from tension-type headache, no neurological disorders are detected unless there are concomitant neurological diseases. The diagnosis is based on anamnestic data and the exclusion of other possible diseases manifested by headache [1,5,6].
As antidepressants for TTH, amitriptyline at a dose of 12.5–50 mg/day, imipramine at a dose of 100–200 mg/day, anafranil (clomipramine) at 25–150 mg/day, fluoxetine at 20 mg are taken for one to two months. /day, tianeptine at a dose of 25–37.5 mg/day or others. Alprazolam 0.75–1.5 mg/day or others are used as tranquilizers. Muscle relaxants are especially effective as additional agents. Physical exercises, massage, thermal procedures, electrotherapy and other physiotherapeutic procedures, acupuncture promote muscle relaxation and often have a positive psychotherapeutic effect on the patient.
The cause of periodic attacks of intense headaches in patients with arterial hypertension, especially young people, may be migraine attacks.
Characteristic signs of migraine [1,5,6]:
- moderate or severe pain intensity,
- pulsating nature of the pain,
- unilateral localization of pain (hemicrania),
- increased pain during physical activity, walking up stairs,
- nausea and/or vomiting,
- combination of light and sound sensitivity
The first migraine attacks usually occur in childhood, adolescence or young adulthood, less often in adulthood and extremely rarely in the elderly. The duration of the attack is from an hour to three days, most often 8–12 hours. In many cases of migraine, its hereditary nature can be traced, which is more pronounced on the maternal side. Neurological examination of patients with migraine in the interictal period does not reveal neurological disorders, unless there is a concomitant neurological disease. The diagnosis of migraine is based on anamnestic data and the exclusion of other diseases manifested by headache attacks [1,5,6].
Treatment of a migraine attack
symptomatic therapy pathogenetic therapy
symptomatic therapy pathogenetic therapy
- non-narcotic
- digidergot analgesics (nasal spray)
- non-steroidal anti-
- sumatriptan sedatives
- zolmitriptan
- antiemetics
- naratriptan
Various medications are used to relieve a migraine attack.
Drugs with symptomatic (nonspecific) action include non-narcotic analgesics (acetylsalicylic acid and paracetamol alone or in the form of combination drugs) and non-steroidal anti-inflammatory drugs (naproxen, diclofenac). For severe nausea and vomiting, the use of metoclopramide 10 mg orally or in the form of rectal suppositories, domperidone 10–20 mg orally helps. Pathogenetic (specific) antimigraine drugs include dihydroergotamine mesylate and serotonin receptor agonists: sumatriptan in a dose of 25 to 100 mg orally or 6 mg subcutaneously, zolmitriptan in a dose of 2.5–5 mg, naratriptan in a dose of 2.5 mg orally or 1, 5 mg subcutaneously. Dihydergot is not recommended for coronary heart disease, atherosclerotic lesions of peripheral and cerebral arteries, which is often observed in patients with arterial hypertension, especially in old age. Experience with the use of serotonin agonists in patients over 65 years of age is limited; they are contraindicated in patients with coronary heart disease or previous myocardial infarction. Preventing migraine attacks
- elimination or weakening of the action of provoking factors;
- rational organization of work and rest regime (for frequent (more than twice a month) and severe attacks);
- b-blockers;
- antidepressants (for depressive disorders);
- tranquilizers (for anxiety disorders without depression);
- calcium channel antagonists.
Since various factors can provoke migraine attacks, it is necessary to identify such factors (if any) in each patient and discuss the possibilities of eliminating or reducing their effect. Of great importance are the rational organization of work and rest, sufficient but not excessive sleep, and psychotherapy for increased anxiety. The use of medications to prevent migraine attacks is indicated only for frequent (two or more per month) and severe migraine attacks. The duration of treatment is at least one month. Such drugs can be used as b-blockers (propronalol 20–80 mg/day, atenolol 50–100 mg/day, metoprolol 50–100 mg/day), tricyclic antidepressants (amitriptyline 12.5–75 mg/day). day, and others), tranquilizers and calcium channel blockers (verapamil 120–240 mg/day, nimodipine 60–120 mg/day).
Isolated antihypertensive therapy in patients with migraine and tension-type headache
often a decrease in blood pressure while headache persists
patient dissatisfaction with treatment results
often refusal of antihypertensive therapy
Combination of antihypertensive therapy and treatment of tension-type headache or migraine
improved well-being and sustained reduction in blood pressure
continuation of antihypertensive therapy under blood pressure control
Antihypertensive therapy in patients with arterial hypertension, suffering from migraine or tension-type headache, causing a persistent decrease in blood pressure, is often not accompanied by a reduction in headaches and an improvement in well-being, so many patients stop further treatment [4]. In such cases, the combination of antihypertensive drugs with antidepressants (or other drugs for the treatment of migraine or tension headaches) can improve the patient’s well-being and achieve a long-term and persistent reduction in blood pressure [4], which forms the basis for the prevention of stroke and other cardiovascular diseases.
In a simplified form, the diagnosis and treatment of headaches in patients with arterial hypertension can be presented as follows:
Literature:
1. Vein A.M., Kolosova O.A., Yakovlev N.A., Karimov T.K. Headache. – M., 1994. – 286 p.
2. Parfenov V.A., Zamergrad M.V. // Neurological journal. – 1998. – No. 5. – P. 41–43.
3. Parfenov V.A., Alekseev V.V., Shvareva I.S., Ryzhak A.A. // Wedge. Gerontology – 2001. – No. 5–6.– P. 3–9.
4. Parfenov V.A., Ryzhak A.A. // Neurological journal. – 2003. – No. 3. (in print).
5. Yakhno N.N., Parfenov V.A., Alekseev V.V. Headache. – M., 2000 – 150 p.
6. Headache Classification Committee of the International Headache Society // Cephalalgia. – 1988. – V. 8, (Suppl. 7) – 96 p.
Prevention methods
Most patients are diagnosed with acquired hypertension. This means that timely prevention will help avoid its occurrence and strengthen blood vessels. At home you need to follow simple rules:
- provide daily moderate exercise;
- spend time outdoors;
- control weight, prevent the development of obesity;
- follow the principles of proper nutrition;
- to refuse from bad habits.
The Clinical Brain Institute offers individual programs for diagnosing and treating headaches caused by high blood pressure. Here you can get competent advice from doctors, undergo a full examination and monitor the dynamics of the development of the disease. Hypertension is not dangerous if you follow the recommendations, take medications on time and avoid situations that provoke increased blood pressure.
Clinical Brain Institute Rating: 5/5 — 5 votes
Share article on social networks
Which number is more important?
Typically, more attention is paid to systolic blood pressure (the first number) as the main risk factor for cardiovascular disease for people over 50 years of age. For most people, systolic blood pressure rises steadily with age due to the loss of elasticity of the large arteries, an increase in heart rate, and the development of vascular disease.
However, an elevated systolic or elevated diastolic blood pressure value can be used to diagnose high blood pressure. The risk of death from coronary heart disease and stroke doubles with a 20 mmHg increase in systolic blood pressure. Art. or diastolic by 10 mm Hg. Art. among people aged 40 to 89 years.
Treatment of headaches with low blood pressure
Headache with low blood pressure is typical for hypotensive people - people who experience a chronic decrease in blood pressure. This condition can be caused by overeating, alcohol, stress, and changes in weather conditions. A typical clinical picture of this condition is the appearance of dull, throbbing pains that are pressing and paroxysmal in nature.
Vascular headaches are often caused by:
- decreased venous tone, manifested by bursting pain in the back of the head;
- decreased tone of the cerebral arteries, which is characterized by aching pain in the temples, crown of the head and lasting for a long time.
In hypotensive patients, headaches often develop as a result of reasons such as:
- physical fatigue;
- daytime sleep;
- intellectual overstrain;
- first trimester of pregnancy;
- starvation;
- stay in transport;
- being indoors.
Sometimes cephalalgia becomes a precursor to a migraine attack in hypotensive patients. Shortly before the attack, the patient becomes nervous and irritable, after which an attack of pain begins in the forehead and temples, it is pulsating and very intense. Treatment of headaches and pressure should begin as early as possible, since the result depends on this. In this case the following is used:
- Baralgin;
- Vitamins (B12, C);
- Antispasmodics;
- Citramon;
- Paracetamol;
- Tincture of ginseng or eleutherococcus;
- Caffeine.
Please note: It is impossible to treat headaches during pregnancy and lactation without consulting a doctor, since many drugs are prohibited during this period.