Unfortunately, there are a great many reasons that can lead a person to disability. For the convenience of conducting MSE (medical and social examination), they are classified by combining similar intellectual, mental and physical health disorders into separate categories consisting of smaller subgroups. One of them includes polyneuropathies, or as they are also called polyradiculoneuropathies.
This is a large group of diseases, heterogeneous in their etiology and some symptoms, that arose as a result of the influence of negative exogenous or endogenous factors.
The pathologies are united by extensive, usually distal, symmetrical damage to the peripheral nerves, leading to sensory, motor, autonomic-vascular and trophic disorders. All this often significantly reduces the patient’s quality of life, thereby leading to loss of ability to work to one degree or another.
What is lower extremity neuropathy?
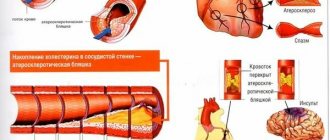
Neuropathy is damage to peripheral nerves and the vessels that supply them. Initially, this disease is not inflammatory in nature, but later it can be layered with neuritis - inflammation of nerve fibers. Neuropathy of the lower extremities is included in the group of polyneuropathies, the basis of which is metabolic disorders, tissue ischemia, mechanical damage, and allergic reactions.
Neuropathy is classified according to the type of course:
- spicy;
- chronic;
- I'll sharpen it up.
Depending on the type of pathological process in nerve fibers, neuropathy can be axonal (encompasses the processes of neurons - axons) and demyelinating (extends to the sheaths of nerve fibers). According to the symptoms, the pathology is:
- Touch
. Symptoms of sensory impairment and pain predominate. - Motor
. It manifests itself mainly as movement disorders. - Vegetative
. Signs of vegetative and trophic disorders are noted.
Advertising:
The causes of the pathology are varied. Thus, the diabetic form is characteristic of metabolic disorders in neurons in diabetes mellitus. Toxic, alcoholic is caused by poisoning, intoxication. Other possible causes are tumors, deficiency of vitamins B, hypothyroidism, HIV, trauma, family history.
With sciatica, a person experiences pinching of the nerve trunk in the lumbar region. This leads to severe pain, so treatment must be timely and correct. Read more in the article: “drug treatment of sciatica, main symptoms.”
Treatment
Treatment of polyneuropathy includes the maximum possible elimination of the cause that led to its development.
- So, if there is diabetic polyneuropathy, then it is necessary to strictly and constantly monitor blood sugar and be under the supervision of an endocrinologist in order to prevent decompensation of the underlying disease.
- If polyneuropathy has developed due to alcoholism, you must completely stop drinking alcohol. It is necessary to adjust your diet and treat with vitamins if a deficiency has developed.
- Treatment of polyneuropathies, which are based on autoimmune processes, is called pathogenetic therapy. At the same time, treatment is also individualized and selected depending on the type of disease, taking into account all the nuances of the disease mechanism and the individual characteristics of the patient. This includes treatment with high doses of glucocorticoid hormones, the use of cytostatics and monoclonal antibody drugs in the treatment, high-dose intravenous immunotherapy with human class G immunoglobulin drugs and high-volume programmed plasmapheresis.
Sensory disorders - the main group of symptoms
Manifestations of pathology in the leg area can be varied, often depending on the cause of neuropathy. If the disease is caused by injury, symptoms affect one limb. In diabetes mellitus and autoimmune diseases, symptoms spread to both legs.
Sensory disturbances can be so unpleasant that they cause depression in the patient.
Sensory disturbances occur in all cases of lower extremity neuropathy. Symptoms are usually observed constantly, do not depend on body position, daily routine, rest, and often cause insomnia.
- numbness of the legs;
- crawling sensation;
- sensation of the presence of foreign objects under the skin.
Advertising:
In addition to the described signs, there are often sensory disturbances - slow recognition of cold and hot, changes in the pain threshold, regular loss of balance due to decreased sensitivity of the feet. Pains also often appear - aching or cutting, weak or literally unbearable, they are localized in the area of the affected area of the nerve.
[media=
https://youtu.be/svHRBJ9gOgU
]
Causes of disability due to polyneuropathy
Diseases in this group, as already mentioned, can develop against the background of exposure to a variety of factors, therefore the following are considered to be the causes of disability:
- General disease.
- Childhood disability.
- Disability that occurred due to an illness received during military service, or that arose within 3 months after dismissal from the Armed Forces.
- Occupational disease: polyneuropathy arose under the influence of toxic substances in industrial conditions, under the influence of physical factors (cold polyneuropathy, vibration disease, autonomic polyneuropathy of overexertion of the hands).
Reference! During the assignment of a disability group resulting from the specific nature of work activity, the degree of loss of professional ability to work is simultaneously determined, expressed as a percentage.
Other signs of the disease
As the pathology of the extremities develops, the motor nerve fibers are damaged, and therefore other disorders occur. These include muscle spasms, frequent cramps in the legs, especially in the calves. If the patient visits a neurologist at this stage, the doctor notes a decrease in reflexes - knee and Achilles. The lower the reflex strength, the further the disease has progressed. In the final stages, tendon reflexes may be completely absent.
The main task of Magnelis B6 is to prevent magnesium deficiency in the body. Vitamin B6, which is also included in its composition, helps the body absorb magnesium from a synthetic preparation. Read more in the article: “What is Magnelis b6 taken for?”
Muscle weakness is an important sign of leg neuropathy, but it is characteristic of the later stages of the disease. At first, the feeling of muscle weakening is transient, then it becomes permanent. In advanced stages this leads to:
- decreased activity of the limbs;
- difficulty moving without support;
- muscle thinning and atrophy.
Advertising:
Vegetative-trophic disorders are another group of symptoms of neuropathy. When the autonomic part of the peripheral nerves is affected, the following symptoms occur:
- hair falls out on the legs;
- the skin becomes thin, pale, dry;
- areas of excessive pigmentation appear;
- the work of the sweat and sebaceous glands changes.
In patients with neuropathy, cuts and abrasions on the legs do not heal well; they almost always fester. Thus, with diabetic neuropathy, changes in trophism are so severe that ulcers appear, and sometimes the process is complicated by gangrene.
O.S. Levin
Department of Neurology RMAPO, Moscow
Polyneuropathy is a disease of the peripheral nervous system, characterized by diffuse, relatively symmetrical damage to nerve fibers and manifested by motor, sensory and autonomic symptoms. Pain, along with paresis, amyotrophy, loss of tendon reflexes, changes in sensitivity, dysfunction of the cardiovascular system, and trophic disorders, are among the most common manifestations of polyneuropathies [1]. Often, pain is the main complaint of patients with polyneuropathies and the decisive factor that reduces their quality of life. Pain in polyneuropathies is a classic example of neuropathic pain, which, unlike the most common - nociceptive pain - is associated not with irritation of pain receptors transmitted to the central nervous system, but with changes in the properties of somatosensory nerve fibers [2]. The high intensity and persistence of neuropathic pain, its special, often painful nature, and resistance to traditional methods of pain relief make this problem of exceptional relevance [2, 6, 7].
Peculiarities of pain syndrome in polyneuropathies The nature of pain in polyneuropathies can be different, but the most typical is constant burning, itching, cerebral or cold, less often there is a more acute piercing, shooting, cutting, tearing, stabbing [1, 3, 6]. The pain is usually accompanied by a change in sensitivity and is usually localized in the same area. In most cases, pain begins from the most distal parts - the plantar surface of the feet, which is explained by the advanced damage to the longest nerve fibers, and then, like other symptoms of polyneuropathy, it can spread in the proximal direction (i.e., it has a polyneuropathic type of distribution) [6] . Pain can be spontaneous or caused. Induced pain includes hyperalgesia and allodynia. Hyperalgesia is characterized by increased pain sensitivity, as a result of which relatively intense pain can be induced by relatively weak painful stimulation. Allodynia is characterized by the occurrence of pain with non-painful irritation - touch, light pressure, line irritation or kneading (mechanical allodynia), exposure to a weak thermal stimulus that normally does not cause pain (cold or heat allodynia), movement. Due to hyperalgesia and allodynia, the skin becomes extremely painful. In typical cases, the patient cannot even bear the touch of a woolen blanket, and then sometimes even ordinary bed linen. As hypoesthesia progresses and deepens, pain may be replaced by numbness, and the painful area may move proximally. The pain is often observed at rest and intensifies at night, disturbing sleep. Constant, painful, difficult to treat pain often leads to emotional depression, which, in turn, increases pain [16]. In chronic polyneuropathies, in a significant number of cases, pain tends to spontaneously improve over several months, but sometimes it steadily increases along with other manifestations of polyneuropathy. Regression of pain may indicate not only restoration of function, but also further progression of the pathological process (in the latter case, pain decreases against the background of an expansion of the zone of decreased surface sensitivity). The nature of pain in polyneuropathy depends on the severity of the process, the type and caliber of the affected fibers. Severe pain more often occurs with axonal neuropathies that predominantly affect thin fibers [1, 2, 6]. In this regard, pain often accompanies disorders of pain and temperature sensitivity, as well as vegetative-trophic disorders. Possible causes of polyneuropathy with severe pain are presented in Table. 1. In clinical practice, the most common cause of painful polyneuropathy is diabetes mellitus (diabetic polyneuropathy) [7, 16].
Pathogenesis of pain in polyneuropathy The direct cause of pain and accompanying phenomena such as hyperalgesia, allodynia or dysesthesia is most often damage to Aδ- and C-fibers [2, 16]. The phenomena of loss and irritation are intricately intertwined. The details of this process remain unclear, but, apparently, some role is played by sensitization of nociceptors and associated C-fibers, which is associated with the phenomena of neurogenic inflammation, ectopic spontaneous activity of partially damaged areas of nerve fibers and regenerating axonal processes, ephaptic (without the participation of a mediator ) transmission of impulses from one axon to another (for example, between somatosensory and pain fibers) upon their contact. Of importance, apparently, is also the secondary functional reorganization of central neurons under the influence of enhanced peripheral afferentation, in particular, central sensitization at the level of the dorsal horns of the spinal cord. One of the universal mechanisms of neuropathic pain is an increase in the excitability of nerve fiber membranes, associated with an increase in the expression of voltage-gated sodium channels [9].
Principles of treating pain in polyneuropathies Treatment of pain in polyneuropathies involves influencing, first of all, etiological and pathogenetic processes (Table 2), as well as all possible factors contributing to the development or intensification of pain. For example, in diabetic polyneuropathy, the most common form of painful polyneuropathy, hyperglycemia plays an important role in the pathogenesis of pain, which can lower the pain threshold and reduce the effect of analgesics, so normalizing blood glucose levels can lead to a significant reduction in pain [1, 16]. Neuropathic pain, unlike nociceptive pain, is difficult to treat with conventional analgesics and NSAIDs, but it can be controlled using several groups of neurotropic drugs that affect certain mechanisms of neuropathic pain. These include antidepressants, anticonvulsants, local anesthetics, tramadol, opioid analgesics and some other drugs [9, 12, 13]. The mechanism of action of drugs for the treatment of neuropathic pain is presented in Table. 3. Antidepressants have a moderate effect in chronic pain of any origin, but they occupy a particularly important place in the treatment of neuropathic pain. The therapeutic efficacy of antidepressants prescribed for the relief of neuropathic pain has been convincingly demonstrated in a meta-analysis of a number of placebo-controlled studies. The analgesic effect of antidepressants is not directly related to their antidepressant effect, as evidenced by the fact that it often occurs at significantly lower doses and occurs more quickly. It is assumed that the analgesic effect is associated with increased activity of noradrenergic and serotonergic systems, which have an inhibitory effect on the transmission of pain impulses along nociceptive pathways in the central nervous system [6]. Tricyclic antidepressants have the highest analgesic activity and are considered the drugs of choice for neuropathic pain. Additional mechanisms of their action are blockade of sodium channels and antagonism of NMDA-glutamate receptors, which mediate hyperalgesia and allodynia [3, 8, 9]. The most widely used is amitriptyline. The initial dose of the drug is 10-12.5 mg at night, then the dose is gradually increased by 10-25 mg every 7 days until the effect is achieved (maximum 150 mg/day). The daily dose is taken once at night or divided into 2-3 doses. In some patients, the analgesic effect is achieved when administered in small or medium doses, in others - only when used in high doses. With concomitant depression, higher doses of the drug are usually required. If amitriptyline is intolerant, other tricyclic antidepressants, such as imipramine or clomipramine, may be prescribed. The trial of antidepressant treatment should last for at least 6-8 weeks, with the patient taking the maximum tolerated dose for at least one to two weeks. Although amitriptyline is effective in approximately 70% of patients with neuropathic pain, excessive sedation, pronounced anticholinergic effects (dry mouth, constipation, urinary retention, etc.), and adverse effects on the cardiovascular system limit its use. It should be noted that in patients with damage to autonomic fibers (autonomic neuropathy) and clinically obvious or hidden autonomic failure developing as a result, sensitivity to the side effects of tricyclic antidepressants (on the cardiovascular system, urinary system, etc.) is especially high. Before prescribing any tricyclic antidepressant, a preliminary ECG is mandatory, especially in people over 40 years of age. The use of tricyclic antidepressants should be limited in patients with urinary retention, angle-closure glaucoma, cognitive impairment, balance and gait disorders. If tricyclic antidepressants are poorly tolerated, it is possible to use tetracyclic antidepressants (for example, maprotiline, 25-100 mg/day) or serotonin and norepinephrine reuptake inhibitors (venlafaxine, 150-225 mg/day, or duloxetine, 60 mg/day) [8]. Selective serotonin reuptake inhibitors (citalopram, paroxetine) cause fewer side effects, but have a less clear analgesic effect, which may be explained by the lack of a direct effect on noradrenergic transmission. They are indicated mainly in cases where pain is associated with depression, and the patient does not tolerate other antidepressants [6, 8, 13]. Anticonvulsants, according to controlled studies, reduce the intensity of pain by at least half in an average of more than 50% of patients with neuropathic pain. The effectiveness of anticonvulsants, like antidepressants, is very variable, and it is almost impossible to predict in advance whether a particular patient will experience pain relief with the help of a particular drug. Currently, in patients with painful polyneuropathies, controlled clinical trials have proven the effectiveness of two drugs: gabapentin and pregabalin [8]. Gabapentin is a structural analogue of GABA, but its mechanism of action is explained by the interaction of the drug with alpha2-delta (α2δ), a subunit of voltage-dependent calcium channels. This leads to a decrease in the release of mediators such as glutamate and substance P, and inhibition of the passage of nociceptive impulses at the level of the spinal cord. The initial dose of gabapentin is 100-300 mg at night. Then the daily dose is gradually increased every 3-5 days by 100-300 mg, moving to a three-time dose. The average effective dose is 1800 mg/day (600 mg 3 times a day), the maximum is 3600 mg/day. Gabapentin dosage titration may take 2 to 8 weeks. Before concluding that the drug is ineffective, its maximum tolerated dose should be taken for one to two weeks. In addition to reducing pain, the drug can help normalize the affective state of patients and night sleep, however, some patients may develop unwanted drowsiness. To avoid this, it is recommended to take most of the dose at night. Other side effects: dizziness, gastrointestinal disorders, peripheral edema, weight gain - are usually mild and rarely require discontinuation of the drug. In elderly people, as well as in the presence of deep sensory impairment, the drug should be used with caution, as it may aggravate balance and gait disorders. The dose of gabapentin should also be limited in case of renal failure. In general, gabapentin has a moderate analgesic effect in polyneuropathies, but its relative safety makes it the drug of choice in cases where patients cannot take tricyclic antidepressants. Pregabalin, like gabapentin, is a ligand for the α2δ subunit of calcium channels. It is approximately equivalent to gabapentin in terms of efficacy and safety, but has some pharmacokinetic advantages that eliminate the need for lengthy titration and create the conditions for a more rapid effect. Controlled studies have shown the effectiveness of pregabalin in painful diabetic polyneuropathy (at a dose of 150-600 mg/day) [6, 8]. The effectiveness of anticonvulsants that block sodium channels in polyneuropathies has been less studied. The most prominent member of this group of drugs, carbamazepine, has long been used in the treatment of neuropathic pain and remains the drug of first choice for trigeminal neuralgia. Carbamazepine is initially prescribed at a dose of 100 mg twice a day, then it is increased to 200 mg 3-4 times a day. The maximum dose is 1200 mg/day. Side effects (dizziness, ataxia, blurred vision, nausea, drowsiness, headache) are less likely with a slow increase in dose. It is preferable to use slow-release carbamazepine preparations, which can be taken twice a day. They provide a more stable concentration of the drug throughout the day, which reduces the likelihood of side effects. If carbamazepine is insufficiently effective or intolerable, oxcarbazepine (300-1200 mg/day) may be used. Data on the effectiveness of phenytoin, topiramate, lamotrigine, valproic acid, and levetiracetam in the treatment of pain in polyneuropathies are contradictory, however, their use may be justified in resistant cases [3, 4, 13]. Local anesthetics, such as lidocaine or its oral analog mexiletine, along with anticonvulsants, are drugs that stabilize cell membranes. The mechanism of action of drugs of this class is associated with the blockade of sodium channels in nerve fibers and the suppression of ectopic spontaneous generation of impulses in them. Lidocaine is prescribed intravenously at a dose of 5 mg/kg in 100-200 ml of isotonic solution over 40-60 minutes for one to three weeks. In some cases, a short course of IV lidocaine infusion can lead to surprisingly durable relief of intense pain, but the risk of numerous side effects, primarily on the cardiovascular system, limits the practical value of this method. In recent years, a new dosage form of lidocaine has been developed - plates for transdermal administration of the drug (transdermal therapeutic system - TTS). TTC with lidocaine (Versatis) is attached to the area of maximum pain (for example, the lower leg area), especially if hyperalgesia and allodynia are detected in this area. The main advantage of this dosage form is the absence of side effects associated with the systemic action of lidocaine [5]. In addition, the plate covers the area of altered sensitivity from additional mechanical irritation. Due to its long-lasting effect, TTC with lidocaine often helps to successfully control pain at night, which can be especially painful for the patient. In a placebo-controlled study in patients with painful diabetic polyneuropathy, the use of TTC with lidocaine led to a persistent reduction in pain intensity by more than a third and a significant improvement in quality of life due to increased general activity, mood, ability to move, ability to work, and improved sleep [5]. By the end of the study, about a quarter of patients who had particularly good effects were able to stop other pain medications, switching to monotherapy, or at least significantly reducing their dose. Similar results were obtained in patients with idiopathic sensory polyneuropathy [11]. When using TTS with lidocaine, from one to three plates are attached simultaneously for no more than 12 hours a day. The trial treatment should last at least two weeks. When a therapeutic effect is obtained, plates with lidocaine can, if necessary, be used for a long time without weakening the analgesic effect. Tramadol (Tramal) has an analgesic effect based on a dual mechanism. In addition to its effect on mu-opioid receptors (its affinity for them is approximately 10 times weaker than that of codeine), it is also able to inhibit the reuptake of serotonin and norepinephrine, which, apparently, significantly potentiates the moderate analgesic effect that is achieved relatively weak opioid effect. The therapeutic effect of tramadol in painful polyneuropathy has been proven in at least two placebo-controlled studies [10]. Treatment begins with a dose of 50 mg at night (or 25 mg 2 times a day), after 5-7 days the dose is increased to 100 mg/day. If necessary, the dose is increased to 100 mg 2-4 times a day. The trial of tramadol should last for at least 4 weeks [9]. Effectiveness can be maintained with long-term use for 6 months or more. The risk of drug dependence with tramadol is significantly lower than with other opioids and can be considered minimal. Moreover, according to EH Adams et al. (2006), when using tramadol for a year, signs of drug dependence or abuse did not occur more often than when using NSAIDs [4]. However, caution should be exercised when prescribing tramadol to persons prone to drug dependence. The likelihood of side effects (dizziness, nausea, constipation, drowsiness, orthostatic hypotension) is lower with slow dose titration. Tramadol should be prescribed with caution to elderly people, in whom the dose of the drug should not exceed 300 mg/day [4, 9]. The combination of tramadol with paracetamol (Zaldiar) allows you to reduce the dose of tramadol and thereby the risk of side effects without sacrificing the analgesic effect [14]. When combining two of these drugs, which have different mechanisms of action (the mechanism of the analgesic effect of paracetamol may be associated with an inhibitory effect on the central synthesis of prostaglandins, possibly due to inhibition of COX-3), a synergistic effect occurs. Adequate pain relief when taking a complex of drugs is observed 1.5-3 times more often than when using each of the compounds in appropriate doses. In addition, paracetamol and tramadol are characterized by a complementary pharmacokinetic profile, due to which the drug quickly begins to act - within 15-20 minutes (due to paracetamol) and maintains an analgesic effect for a long time (due to tramadol) [14, 15]. Due to the fact that Zaldiar contains a low dose of tramadol (one tablet contains 37.5 mg of tramadol and 325 mg of paracetamol), side effects when using it (especially nausea, vomiting and dizziness) occur less frequently than when using tramadol at the minimum recommended level. single dose (50 mg). Moreover, to date, experience has been accumulated in long-term therapy with Zaldiar, in particular in patients with neuropathic pain, back pain, osteoarthritis, etc. It indicates the long-term preservation of the effect of the drug, the absence of a tendency to develop tolerance and drug dependence. Thus, during a 23-month open study in patients with chronic back pain there was no need to increase the dose of Zaldiar, which indicates the absence of tolerance. Prescribing the drug does not require long-term dose titration; treatment can be started with a dose of one or two tablets per day, and subsequently the dose can be increased to 4 tablets per day [15].
Use of other drugs for neuropathic pain To enhance the analgesic effect, alpha2-adrenergic receptor agonists (clonidine, tizanidine), GABAergic drugs (baclofen, clonazepam), and NMDA-glutamate receptor blockers can be used. For more or less localized pain, external use of capsicum preparations is advisable. The capsaicin they contain, stimulating capsaicin receptors, promotes the depletion of substance P and other neurotransmitters in peripheral tissues, the release of which is associated with the development of hyperesthesia and burning pain. It is preferable to use 0.025-0.075% capsaicin cream. The drug is applied to the skin 2 to 4 times a day for no more than 6 weeks [4, 6, 9].
Sequence of use of drugs for the treatment of neuropathic pain Today, the choice of drug for the treatment of pain in polyneuropathy can not be based either on its nature or on its intended mechanism, and must be carried out empirically, taking into account the effectiveness and safety of individual drugs, the individual sensitivity of the patient, and economic accessibility , the presence of concomitant diseases [6, 8]. For example, in case of serious cardiovascular pathology, angle-closure glaucoma, severe autonomic disorders, in particular with a tendency to orthostatic hypotension or urinary retention, the use of tricyclic antidepressants should be avoided. Due to the lack of direct comparative studies that would compare the effectiveness of various drugs for the treatment of neuropathic pain, their effectiveness is usually measured indirectly - by the NNT indicator (“the number of patients who need to be treated to achieve 50% pain relief in one patient”) [6, 8]. This indicator is calculated based on data from specific studies; the lower it is (closer to unity), the higher the average effectiveness of the drug. This indicator is complemented by another indicator that assesses the safety of the drug - NNH (“the number of patients who need to be treated in order to experience a side effect that forces the drug to be discontinued (“cause harm”).” The higher the NNH, the safer the drug. Table 4 the indicated indicators are presented in relation to the main drugs used in the treatment of neuropathic pain. The practical usefulness of the drug is most accurately evidenced by the NNT/NNH ratio, which is lower, the more favorable. The optimal balance of effectiveness and safety for painful polyneuropathies was noted in tricyclic antidepressants, gabapentin (pregabalin) and tramadol, which are usually considered first-line drugs in patients with painful polyneuropathy.6,8,9 When the prevalence of pain is limited, TTC with lidocaine can be added to the first-line drugs.6 In any case, each drug prescribed to a patient with neuropathic pain, it is necessary to give a full chance to “prove itself,” which presupposes its administration in an adequate dose (subject to good tolerance) for a sufficiently long period, indicated above in the description of each individual drug [7]. To assess the effectiveness of pain treatment, it is useful to use a visual analogue scale. Typically, the effect of a drug can be considered clinically significant if the score on this scale is reduced by at least 50%.
Combining medications in the treatment of neuropathic pain None of the drugs provides a guaranteed effect for neuropathic pain. Therefore, although, as a general rule, efforts should be made to limit the number of medications a patient takes simultaneously, in most cases, neuropathic pain can be adequately controlled only with the help of a combination of two or more drugs. It is irrational to immediately prescribe a combination of several drugs: initially one should try one drug, and only after making sure that in doses tolerated by a given patient it has only a partial effect, the next drug should be added to it, which, as a rule, has a different mechanism of action. In clinical practice, an antidepressant is often combined with an anticonvulsant, an anticonvulsant with tramadol or Zaldiar. A combination of two anticonvulsants acting on different ion channels, for example gabapentin and carbamazepine, is also possible, but the combination of carbamazepine and lamotrigine is irrational. TTC with lidocaine can be added to any of these combinations. It is recommended to avoid combining tramadol (especially large doses) with MAO inhibitors, selective serotonin reuptake inhibitors or serotonin and norepinephrine, as such a combination can provoke serotonin syndrome. Tramadol should be prescribed with caution in combination with tricyclic antidepressants (given the risk of serotonin syndrome) [5]. When treating pain, it is necessary to widely use the possibilities of non-drug treatment methods (psychotherapy, psychophysiological relaxation, reflexology, balneotherapy, transcutaneous electrical neurostimulation, magnetic therapy and other physiotherapeutic procedures). We must not forget about the powerful resource of psychotherapeutic influence, as well as the fact that many patients with neuropathic pain are extremely sensitive to placebo, the therapeutic potential of which must also be exploited.
Literature 1. Levin O.S. Polyneuropathy. M.: MIA, 2006. 496 p. 2. Strokov I.A., Barinov A.N. Clinic, pathogenesis and treatment of pain syndrome in diabetic polyneuropathy // Neurological Journal. 2001. No. 6. P. 47-54. 3. Shtulman D.R., Levin O.S. Neurology. Handbook of a practicing physician. M.: MEDpress-inform, 2005. 944 p. 4. Adams EH, Brenier S, Cicero TJ et al. A comparison of the abuse liability of tramadol, NSAIDs and hydrocodone in patients with chronic pain // J. Pain Symptom Manage, 2006. V. 31(5). P. 465-476. 5. Barbano RL, Herrmann DN, Hart-Gouleau S, et al. Effectiveness, tolerability, and impact on quality of life of the 5% lidocaine patch in diabetic polyneuropathy // Arch. Neurol., 2004. V. 61. P. 914-918. 6. Bennet M. (ed). Neuropathic pain. Oxford University Press, 2006. 176 p. 7. Berger A., Dukes EM, Oster G. Clinical characteristics and economic costs of patients with painful neuropathic disorders // Pain. 2004. V. 5. P. 143-149. 8. Fennerup NB, Otto M., McQuay NJ Algorithm of neuropathic pain treatment // Pain. 2005. V. 118. P. 289-305. 9. Dworkin RH Advances in neuropathic pain // Arch. Neurol. 2003. V. 60. P. 1524-1534. 10. Harati Y., Gooch C., Swenson M. et al. Double-blind randomized trial of tramadol for the treatment of the pain of diabetic neuropathy // Neurology, 1998. V. 50. P. 250-257. 11. Herrmann DN, Barbano RL, Hart-Gouleau S. et al. An Open-Label Study of the Lidocaine Patch 5% in Painful Idiopathic Sensory Polyneuropathy // Pain Medicine, 2005. V. 6. P. 379. 12. Irving GA Contemporary assessment and management of neuropathic pain // Neurology, 2005. V. 64 (S.3). S. 21-27. 13. Leo RJ Treatment considerations in neuropathic pain // Curr. Treatment in Neurology, 2006. V. 8. P. 389-400. 14. Medve R., Wang J., Karim S. Tramadol and acetaminophen tablets for dental pain // Anesthesia Progress, 2001. V. 23. P. 34-37. 15. Raffa RB Pharmacology of oral combination analgetics: rational therapy for pain // J. Clin. Pharmac. Therapeutics, 2001. V. 26. P. 257-264. 16. Vinik AI, Mehrabyan A. Diabetic neuropathies // Med Clin North Am., 2004. V. 88. P. 947-999.
The procedure for diagnosing pathology
An experienced neurologist will easily make a presumptive diagnosis based on the symptoms described in the patient’s words and on existing objective signs - skin changes, impaired reflexes, etc.
Diagnostic methods are very diverse, here are some of them:
| Methodology | What does it show |
| Electroneuromyography | Determination of the source of damage to the nervous system - roots, nerve processes, neuron bodies, membranes, etc. |
| General, biochemical blood test | Inflammatory, infectious process, presence of autoimmune changes |
| Blood sugar test | Development of diabetes mellitus |
| X-ray of the spine | Pathologies of the spinal column |
| Spinal tap | Presence of antibodies to own nerve fibers in the spinal cord |
The main method for diagnosing problems with nerve fibers remains the simple technique of electroneuromyography - it helps to clarify the diagnosis.
How does the disease manifest?
Alcoholic polyneuropathy has a set of characteristic symptoms that gradually become more pronounced:
- the muscles of the arms and legs become weak. At first, mild weakness is felt in the palms and feet, and then spreads and becomes more noticeable;
- decrease in sensitivity, its gradual decrease until disappearance;
- decrease in the severity of reflexes up to their absence;
- pain syndrome. The pain may increase gradually or be immediate and severe. Usually pain is not associated with any “external” causes (injuries, stress);
- swelling of the legs, arms;
- the appearance of goosebumps, burning, and other sensations in the limbs;
- tremors, tics, muscle twitching, finger trembling;
- problems with the cardiovascular and respiratory systems (shortness of breath, breathing problems, rapid pulse, arrhythmia);
- sweating (appears unexpectedly and is not associated with exercise, body temperature or heat);
- impaired coordination of movements, dizziness, problems with balance.
Symptoms can increase sharply after severe alcohol intoxication or binge drinking; they often manifest themselves acutely after hypothermia. In other cases, they intensify gradually, against the background of a general deterioration in health due to chronic alcohol dependence. More often, the disease develops subacutely over several weeks or months: the sensitivity of the arms or legs is impaired, and the calf muscles become painful. When squeezed, the pain intensifies. Without treatment, muscle weakness appears - up to paralysis and atrophy.
Order alcoholism treatment
We work around the clock, experienced doctors, 100% anonymous.
Neuropathy Treatment Basics
This disease must be treated comprehensively, always with correction of the underlying pathology. For autoimmune diseases, hormones and cytostatics are prescribed; for diabetes, glucose-lowering medications or insulin; for the toxic type of disease, cleansing techniques (hemosorption, plasmapheresis).
The goals of treatment for lower extremity neuropathy are:
- restoration of nervous tissue;
- resumption of conductivity;
- correction of disorders in the circulatory system;
Advertising: - improvement of well-being;
- reduction of pain and other disorders;
- optimization of motor function of the legs;
- increasing metabolic rate.
There are many treatment methods, the main one being medication.
Surgical treatment is practiced only in the presence of tumors, hernias, and after injuries. To prevent muscle atrophy, all patients are recommended to exercise from a special exercise therapy complex; at first, they are performed under the supervision of a rehabilitation physician.
If you have neuropathy, you should follow a diet with an increase in the content of vitamins B, and you should also exclude alcohol, foods with chemical additives, marinades, fried, and smoked foods.
The disease is successfully treated with physiotherapy. Massage, magnetic therapy, therapeutic mud, reflexology, and electrical muscle stimulation have proven themselves to be excellent. To prevent the formation of ulcers, you should wear special shoes and use orthoses.
Basic drugs for the treatment of pathology
In the treatment of neuropathy, drugs play a leading role. Since the basis is degeneration of nerve tissue, the structure of the nerve roots should be replenished with medication. This is achieved by using the following medications:
Advertising:
- Neuroprotectors
, metabolism accelerators in nerve cells - Piracetam, Mildronate. They improve the trophism of nervous tissue, helping to improve its structure. - Anticholinesterase drugs
- Ipidacrine, Prozerin. They optimize the sensory functioning of nerves and help in the transmission of nerve impulses. - Antioxidants
— Mexidol, Cytoflavin. They help to “quench” the action of free radicals, which aggravate the destruction of peripheral nerves. - Alpha lipoic acid preparations
. They enhance metabolism, enhance the restoration of neurocytes, especially indicated for diabetic neuropathy.
B vitamins are mandatory in the course of therapy, especially B12, B6, B1. Most often, combined drugs are prescribed - Neuromultivit, Milgamma in tablets, injections. After taking them, sensitivity disorders are eliminated, all symptoms are reduced in severity.
What else is used to treat neuropathy?
Advertising:
Vitamins that are powerful antioxidants are very useful for the body in any form of neuropathy of the lower extremities - ascorbic acid, vitamins E, A. They are necessarily used in complex therapy of the disease to reduce the destructive effects of free radicals.
In case of severe muscle spasms, the patient will be helped by muscle relaxants - Sirdalud, Baclofen, which are used only with a doctor's prescription - if abused, they can increase muscle weakness.
There are other medications against this pathology. They are selected individually. These are:
- hormonal agents to suppress pain and inflammation - Prednisolone, Dexamethasone
; - vascular medications to improve blood circulation in tissues - Pentoxifylline, Trental
; - antidepressants, sedatives, drugs against excessive anxiety - Amitriptyline, Duloxetine
; - analgesics, including narcotics for severe pain - Tramadol, Analgin, as well as non-steroidal anti-inflammatory drugs - Ketoprofen, Ketonal Duo
.
Locally it is recommended to use ointments with novocaine, lidocaine, non-steroidal anti-inflammatory drugs, as well as warming ointments with red pepper and animal poisons. In case of bacterial infection of the skin of the feet and legs, bandages with antibiotics are applied (Tetracycline ointment, Oxacillin).
Traditional treatment of neuropathy
Treatment with folk remedies is used with caution, especially for diabetes. Recipes can be like this:
- Combine the yolk of a raw egg and 2 tablespoons of olive oil. Add 100 ml of carrot juice, a tablespoon of honey. Drink 50 ml three times a day after meals. Course - 14 days.
- Pour 2/3 cup of 9% vinegar into a bucket of warm water, add a glass of salt. Soak your feet in the water for 15 minutes. The course is once a day for a month.
- Mix 3 tablespoons of fenugreek seeds, a tablespoon of bay leaf, chop everything. Brew a liter of boiling water in a thermos for an hour, then drink in small portions throughout the day. Course - 10 days.
- Dilute blue clay with water to a paste and apply to feet. Let it dry, then rinse off. Repeat every day for 2 weeks.
With timely treatment, the disease has a good prognosis. Even if the cause of neuropathy is very severe, it can slow or stop its progression and improve a person's quality of life.
Causes
A number of factors can lead to the development of neuropathy, including:
- Alcoholism. A poor diet can lead to vitamin deficiencies.
- Autoimmune diseases. These include diseases such as Sjögren's syndrome, systemic lupus erythematosus, rheumatoid arthritis, Guillain-Barré syndrome, chronic inflammatory demyelinating polyneuropathy and necrotizing vasculitis.
- Diabetes. More than half of people with diabetes develop some type of neuropathy.
- Exposure to poisons. Toxic substances include heavy metals or chemicals.
- Medicines. Some medications, especially those used to treat cancer (chemotherapy), can cause peripheral neuropathy.
- Infections. These include some viral or bacterial infections, including Lyme disease, shingles, Epstein-Barr virus, hepatitis C, leprosy, diphtheria, and HIV.
- Hereditary diseases. For example, a disease such as Charcot-Marie disease is a hereditary type of neuropathy.
- Injury or compression on a nerve. Injuries such as car accidents, falls, or sports injuries can damage or even sever peripheral nerves. Nerve compression can occur when peripheral nerves are continuously impacted.
- Tumors. Malignant and benign tumors can damage or put pressure on nerves.
- Vitamin deficiency. B vitamins, including B-1, B-6 and B-12, vitamin E and niacin are important for nerves.
- Bone marrow diseases. These include the presence of an abnormal protein in the blood (monoclonal gammopathies), multiple myeloma, lymphoma and amyloidosis.
- Other diseases. These include kidney disease, liver disease, connective tissue disease and thyroid disease (hypothyroidism).
Complications of polyneuropathy may include
- Burns and skin injuries. If there is numbness in parts of the body, the patient may not feel temperature changes or pain.
- Infections. The legs and other areas of the body with reduced sensation may become unnoticed. It is necessary to monitor the integrity of the skin, especially if you have diabetes, since even minor damage to the skin can lead to tissue infection.