Polyneuropathy, or peripheral neuropathy, occurs as a result of damage to the peripheral nerves and often results in symptoms such as weakness, numbness and pain, usually in the arms and legs. But polyneuropathy can also affect other areas of the body. Peripheral neuropathy may develop in one nerve (mononeuropathy), two or more nerves in different areas, or may involve many nerves (polyneuropathy).
The peripheral nervous system transmits information from the brain and spinal cord (central nervous system) to the rest of the body. Peripheral neuropathy can result from traumatic injuries, infections, metabolic disorders, hereditary causes, and exposure to toxins. One of the most common causes of polyneuropathy is diabetes mellitus.
Patients with peripheral neuropathy typically describe pain as a tingling or burning sensation. In many cases, symptoms decrease if compensation occurs for the underlying disease.
Each nerve in the peripheral nervous system has a specific function, so symptoms depend on the type of nerve that is damaged. Nerves are divided into:
- Sensory nerves that receive sensations from the skin, such as temperature, pain, vibration, or pressure
- Motor (motor) nerves that control muscle movement
- Autonomic nerves that control functions such as blood pressure, heart rate, digestion, and bladder function
Symptoms
Symptoms of polyneuropathy may include:
- Gradual onset of numbness and tingling in the legs or arms that may spread up the arms and legs
- Sharp stabbing or burning pain
- Increased sensitivity to touch
- Lack of coordination and falling
- Muscle weakness or paralysis if motor nerves are damaged
If autonomic nerves are involved, symptoms may include:
- Heat intolerance, as well as changes in sweating
- Digestive, bladder, or bowel problems
- Changes in blood pressure, which may cause dizziness
Causes
A number of factors can lead to the development of neuropathy, including:
- Alcoholism. A poor diet can lead to vitamin deficiencies.
- Autoimmune diseases. These include diseases such as Sjögren's syndrome, systemic lupus erythematosus, rheumatoid arthritis, Guillain-Barré syndrome, chronic inflammatory demyelinating polyneuropathy and necrotizing vasculitis.
- Diabetes. More than half of people with diabetes develop some type of neuropathy.
- Exposure to poisons. Toxic substances include heavy metals or chemicals.
- Medicines. Some medications, especially those used to treat cancer (chemotherapy), can cause peripheral neuropathy.
- Infections. These include some viral or bacterial infections, including Lyme disease, shingles, Epstein-Barr virus, hepatitis C, leprosy, diphtheria, and HIV.
- Hereditary diseases. For example, a disease such as Charcot-Marie disease is a hereditary type of neuropathy.
- Injury or compression on a nerve. Injuries such as car accidents, falls, or sports injuries can damage or even sever peripheral nerves. Nerve compression can occur when peripheral nerves are continuously impacted.
- Tumors. Malignant and benign tumors can damage or put pressure on nerves.
- Vitamin deficiency. B vitamins, including B-1, B-6 and B-12, vitamin E and niacin are important for nerves.
- Bone marrow diseases. These include the presence of an abnormal protein in the blood (monoclonal gammopathies), multiple myeloma, lymphoma and amyloidosis.
- Other diseases. These include kidney disease, liver disease, connective tissue disease and thyroid disease (hypothyroidism).
Complications of polyneuropathy may include
- Burns and skin injuries. If there is numbness in parts of the body, the patient may not feel temperature changes or pain.
- Infections. The legs and other areas of the body with reduced sensation may become unnoticed. It is necessary to monitor the integrity of the skin, especially if you have diabetes, since even minor damage to the skin can lead to tissue infection.
The prevalence of polyneuropathies (PN) in the population is 2–8%, which is not inferior to the prevalence of stroke [1, 2]. Reasons P.N. are very diverse, often caused by somatic diseases [3]. Diseases of the gastrointestinal tract (GIT) in approximately 10% of cases lead to neurological disorders in both the central and peripheral parts of the nervous system (including in the form of PN) [4-8]; psychoneurological disorders are detected in 25% of patients with PN [9].
Neurological disorders associated with gastrointestinal diseases are based on malabsorption (leading to a deficiency of a number of substances extremely important for maintaining normal cell metabolism), pathology of the gastrointestinal mucosa, and increased sensitivity to the plant protein gluten [6, 8, 10-12]. The occurrence of inflammatory bowel diseases is facilitated by hereditary predisposition [10, 13]. In children, lesions of the nervous system due to gastrointestinal diseases are rare; in adults they occur in 10–36% of cases [5, 6].
Vitamin B12 deficiency
Vitamin B12 (cyanocobalamin) deficiency can lead to a number of neurological disorders, with myelopathy and PN most often observed in patients with pernicious anemia [6]. Vitamin B12 is found mainly in products of animal origin - meat, milk, eggs. Even a strict vegetarian diet does not lead to its deficiency, since the daily dose required for a person is only 5 mcg, which can be obtained by eating legumes. For the absorption of vitamin B12, intrinsic factor is required - a protein that is synthesized by the parietal cells of the stomach. Malabsorption due to intrinsic factor deficiency is the most common cause of vitamin B12 deficiency [14].
Neurological disorders in B12 deficiency include dementia, mental disorders, funicular myelosis and PN; they are observed in approximately 15% of patients and can occur without characteristic hematological changes (megaloblastic anemia) [6, 15, 16]. There is no correlation between the severity of anemia and the severity of neurological disorders. Early manifestations of PN can be paresthesia in the feet, or in the lower and upper extremities. The presence of paresthesia in the upper extremities is rare [6]. The second most common symptom is sensory ataxia. These disorders progress over weeks and months. During a neurological examination, a decrease in vibration sensitivity is most often noted in the legs; similar disorders are observed less frequently in the arms. A decrease in surface sensitivity is also rarely detected. In approximately 20% of cases, a positive Lhermitte sign is detected [6]. Sensitive ataxia may be accompanied by muscle weakness in the legs. Motor impairments are caused by damage to the pyramidal tracts, are more pronounced in the legs and range from mild weakness to spastic lower paraplegia. Deep reflexes in the lower extremities are often reduced or absent, which is associated with the development of PN. PN is mixed in nature - both the axial cylinder and the myelin sheath of the nerves are affected. Patients may also exhibit decreased visual acuity, scotomas, and optic nerve atrophy; Dyspepsia is often noted. Some patients may develop autonomic dysfunction (frequent urination, urinary and fecal incontinence, impotence) [6].
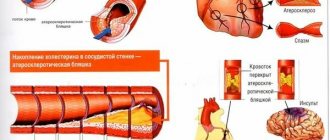
Electromyography (EMG) reveals predominantly axonal neuropathy. Diagnosis is aided by identifying megaloblastic anemia and determining the level of vitamin B12 in the blood serum. More than 90% of patients with cyanocobalamin deficiency have increased levels of homocysteine and methylmalonic acid. 60-90% of patients have antibodies to gastric parietal cells and intrinsic factor in their blood serum. An increase in homocysteine levels is one of the cardiovascular risk factors; against the background of hyperhomocysteinemia, the risk of thrombosis and occlusive lesions of the arteries increases.
Vitamin B1 deficiency
A decrease in the concentration of vitamin B1 (thiamine) in the blood serum is detected in 30-80% of patients with alcoholism [17]. Alcohol impairs the absorption of thiamine in the intestine and reduces its reserves in the liver [18]. In addition, the processes of thiamine phosphorylation are disrupted [18]. Vitamin B1 deficiency can occur not only with alcoholism, but also with a number of gastrointestinal diseases - gastric ulcers, chronic gastritis, acute pancreatitis, metastatic lesions of the esophagus, primary tumors of the stomach and esophagus [6, 14]. At the same time, in addition to those characteristic of Wernicke-Korsakoff syndrome and other central nervous system disorders, PN is also observed, including damage to peripheral autonomic fibers [19, 20]. As a result of thiamine deficiency, neuronal metabolism is disrupted, transsynaptic transmission of excitation suffers, and DNA synthesis is reduced. It should be noted that with alcoholism, in addition to thiamine, there is a deficiency of other vitamins - folate (in 60-80% of patients), riboflavin (in 17%), pyridoxine (in 50%), as well as cyanocobalamin, nicotinic and ascorbic acids, vitamin D [17]. PN in alcoholism can also occur with a normal level of thiamine in the blood serum [18, 21], and no dependence of the severity of damage to somatic and autonomic peripheral fibers on the concentration of thiamine has been noted [20]. Development of P.N. associated with the direct toxic effect of ethanol and its metabolites (primarily acetaldehyde) on peripheral nerves [18, 21].
In terms of its clinical manifestations, alcoholic PN is predominantly sensory [18, 21]. The onset of the disease is usually gradual, affecting the lower extremities to a greater extent. Using EMG, signs of axonal damage can be detected before clinical manifestations of the disease occur. With progression, which can last for months, symptoms spread symmetrically from the feet in a proximal direction [18]. In rare cases, the onset of alcoholic PN can be acute or subacute, which requires differential diagnosis with Guillain-Barré syndrome [19].
Most often, patients complain of paresthesia and a burning sensation in the legs [22]. In approximately 25% of patients, the severity of pain can be very significant. Dysesthesia can periodically, especially at night, significantly intensify. Often pain occurs even from slight contact of the skin with clothing.
A neurological examination reveals signs of distal symmetrical PN [22]. Superficial and deep sensitivity suffers to approximately the same extent, but in some patients a predominance of other disorders can be identified. Achilles and often knee reflexes are absent [22]. In moderate cases, flaccid paresis of the muscles of the feet is noted; in more severe cases, paresis of the distal parts of the upper limbs may be detected. During an external examination, patients are noted to have trophic changes in the skin in the distal parts of the lower extremities (hyperpigmentation, ulcerations), and during an X-ray examination, pronounced changes in the joints (neuropathic arthropathy).
Diagnosis of alcoholic PN is based on medical history, relevant clinical features and EMG results. The results of electrophysiological research methods and nerve biopsy confirm the predominant damage to axons [18, 19]. An EMG study of sensory nerves reveals a significant decrease in the amplitude of responses with a minimal decrease in the speed of propagation of excitation. In addition, signs of denervation/reinnervation may be detected in the distal parts of the extremities (especially the lower ones).
Other causes of PN in gastrointestinal diseases leading to vitamin deficiency are deficiency of vitamins P (nicotinamide) and E [6, 8, 12].
Intestinal diseases
With enteropathies, the development of both demyelinating and axonal PN is possible [5, 8]. The reasons that can lead to damage to peripheral nerves are very diverse.
Celiac disease (gluten-sensitive enteropathy) is an inflammatory autoimmune disease that has a certain genetic predisposition (HLA DQ2+ or DQ8+), the clinical manifestations of which occur when eating gluten (gliadin, glutenin) contained in grains (wheat, rye, barley) [10 , 23-25]. Celiac disease occurs in 0.5-1% of Caucasians, and its frequency is highly variable among representatives of different races [10, 24, 26, 27]. In women, the disease occurs twice as often [28]. Classic manifestations of celiac disease, including chronic diarrhea, malabsorption syndrome, vitamin deficiency, and weight loss, are observed in both children and adults [23, 24, 29]. Even in the presence of positive serological tests and biopsy results of the intestinal mucosa, clinical manifestations of the disease may be absent.
Some variants of the course of hypersensitivity to gluten are classified as atypical; in such patients, in addition to endocrine and other disorders, neurological disorders (in particular, gluten ataxia) are detected [28]. This term itself is controversial; such patients still have clinically obvious variants of celiac disease [25]. Neurological disorders in children with celiac disease are rare; the disease is mainly observed in adults [6, 28]. It is believed that neurological and/or mental disorders are present in almost 22% of patients with celiac disease [23, 24], although lower figures are reported in the literature - from 6-8 to 10% [28, 30, 31].
Among the neurological disorders that can occur in such patients, the most frequently mentioned are gluten ataxia (according to some data, it is caused by a decrease in the number of Purkinje cells in the cerebellum in combination with its atrophy and gliosis) and sensorimotor axonal PN [10, 23, 24, 29, 32-35]. It is estimated that gluten ataxia accounts for 15% of all ataxias and 40% of idiopathic sporadic forms [34]. Ataxia is predominantly observed in the lower extremities and during walking [33, 34, 36]. Ataxic phenomena in the upper extremities and dysarthria may also be observed [24]. In rare cases, it is combined with focal myoclonus, palatal tremor or opsoclonus [36]. The disease is characterized by a gradual onset, usually around age 50, and a slowly progressive course. According to MRI, 60% of such patients exhibit cerebellar atrophy [23, 34] and in almost all cases, changes, according to MR spectroscopy, in the region of the cerebellar vermis [34]. In this regard, it should be noted that damage to the cerebellar vermis itself in approximately 40% of cases manifests itself only as trunk ataxia and is not accompanied by ataxia in the limbs, dysarthria or nystagmus.
With increased sensitivity to gluten, rapid progression of ataxia is also possible, reminiscent of the paraneoplastic process. It should be emphasized that this is not the only variant of nervous system disorders in this category of patients, which is largely due to methodological difficulties in assessing neurological disorders with hypersensitivity to gluten [10, 24]. It is believed that various neurological disorders occur in 6-10% of people with gastrointestinal pathology [5, 33, 35]. Considering the significance of increased sensitivity to gluten in multiple system atrophy, it should be noted that there may be another explanation for this fact that is not related to the pathogenetic significance of increased sensitivity to gluten - the phenotypic similarity of multiple system atrophy with disorders that occur with increased sensitivity to gluten [31]. The condition of patients with a long course of the disease and severe malabsorption can significantly worsen when a deficiency of vitamins, especially B vitamins, is added [28].
Increased sensitivity to gluten is considered to be one of the causes of PN [10, 29, 30, 32, 35, 37], although this relationship does not seem to be as clear as with gluten ataxia [38]. PN in patients with gluten intolerance is more often caused by axonal damage, and less often by pathology of the myelin sheath of peripheral nerves [39]. Signs of axonal PN are observed in 40-50% of patients with celiac disease; sometimes oligoclonal antibodies are found in the cerebrospinal fluid of patients [28, 33]. Less common are multiple motor mononeuropathies, small fiber PN, motor PN and PN caused by both axono- and myelinopathy. Pathogenesis P.N. in case of gluten intolerance, it is probably caused by autoimmune disorders, and damage to peripheral nerves occurs regardless of the activity of the main process [40].
It is believed that gluten intolerance as a cause of damage to the nervous system (ataxia, PN) should be considered even in the absence of clinically obvious signs of gastrointestinal disease [30]. In patients with initially diagnosed “idiopathic PN,” gluten intolerance is detected in 1.4% of cases [3].
The course of PN is chronic or slowly progressive [6]. Motor P.N. as they progress, they acquire the features of mixed motor and sensory PN [33]. Sensory P.N. manifests itself as symmetrical pain and paresthesia in the arms and legs, decreased sensitivity in the distal extremities, as well as paresthesia involving the face, trunk or lumbosacral region [28, 30]. Hypersensitivity to gluten is characterized by the development of sensory PN of small fibers, which is confirmed by biopsy results [41]. It often occurs with the appearance of paresthesia and pain in the face or is multifocal in nature [41]. In itself, PN of small fibers is manifested mainly by autonomic and sensory disorders. Typical for these patients are episodes of postural dizziness, photopsia when standing up, and syncope may be observed [42]. Patients often complain of occasional diarrhea that occurs at night and a feeling of fullness in the stomach. Gastroparesis and impotence are characteristic, often in combination with urinary incontinence. Patients are bothered by pain in the distal parts of the legs, less often in the arms. A neurological examination reveals a decrease in pain and temperature sensitivity while maintaining vibration sensitivity and muscle-articular sensation, as well as deep reflexes.
As a rule, excluding gluten from the diet does not significantly affect the severity of PN [6]; in patients, against the background of a decrease in cramps and muscle weakness, paresthesia and sensory disturbances persist [37], although earlier [7, 29], and more recently [3 , 24] researchers report the opposite—a decrease in the severity of gluten ataxia on the background of a gluten-free diet. It is emphasized that early administration of a special diet can lead either to the complete disappearance of symptoms or to the prevention of disease progression. PN caused by hypersensitivity to gluten accounts for 2.5% of all cases of PN [28]. In the absence of other signs of gluten hypersensitivity in a patient, it is unlikely that existing chronic sensorimotor axonal PN is associated with this disease [38]. This statement does not apply to small fiber PN, in which the likelihood of hypersensitivity to gluten is significantly higher [38].
Recently, increased sensitivity to gluten, not associated with gastrointestinal pathology, has attracted increasing attention [43, 44]. It is believed that in the population this syndrome occurs in 0.63–6% of cases [44]. The pathogenesis of this condition remains unclear; clinical manifestations may resemble irritable bowel syndrome or manifest as non-gastrointestinal disorders, including nervous system disorders (fatigue, headache, drowsiness, fibromyalgia-like pain, depression, anxiety) [43, 44]. Schizophrenia and cerebellar ataxia have also been associated with the presence of this condition [43]. However, the available data must be treated with caution, since this problem requires more detailed study.
One of the causes of PN is Crohn's disease, while PN is an axonopathy and is sensory in nature [6]. Upon in-depth examination, Crohn's disease is detected in 0.3% of patients with initially diagnosed “idiopathic PN” [3]. Nonspecific ulcerative colitis is characterized by both acute and chronic inflammatory demyelinating PN [6]. Damage to the peripheral nervous system is more common in ulcerative colitis than in Crohn's disease [8]. It should be noted that the latter is more characterized by disorders not of the peripheral, but of the central nervous system, caused by both a hypercoagulable state and thrombosis, and secondary cerebral vasculitis [8]. The development of predominantly sensory PN may precede other clinical manifestations of Crohn's disease; Folate deficiency is likely responsible for some cases [8]. In addition, in Crohn's disease, in addition to predominantly sensory and sensorimotor PN, damage to the autonomic nervous system is possible [8]. Possible iatrogenic cause of P.N. A case of the development of PN in a patient with Crohn's disease treated with the antitumor necrosis factor-alpha (infliximab) is described [45].
With nonspecific ulcerative colitis, as with Crohn's disease, damage to cerebral arteries and veins is possible, leading to stroke [8]. However, in this category of patients, lesions of the peripheral nervous system are described in the form of acute and chronic inflammatory demyelinating PN [8].
Demyelinating PN has also been described in Whipple's disease, but its cause-and-effect relationship with this disease is questionable [8]. Damage to peripheral nerves is probably not typical for this disease [46–49].
Thus, PN, varying in pathogenesis, clinical manifestations and prognosis, often occurs with a deficiency of B vitamins and gastrointestinal diseases. Their occurrence may be based on damage to the myelin sheath and the axons of peripheral nerves. A thorough history taking, correct assessment of the patient’s complaints and physical examination results, as well as EMG data help in diagnosing such disorders. In some cases, a peripheral nerve biopsy is required to confirm the diagnosis. Timely diagnosis and adequate treatment of these disorders significantly improves the prognosis.
The authors declare no conflict of interest.
Diagnostics
When diagnosing polyneuropathy, a doctor may be primarily interested in answers to the following questions:
- Does the patient have any medical conditions such as diabetes or kidney disease?
- When did the symptoms begin?
- Were the symptoms constant or sporadic?
- How severe are the symptoms?
- What causes symptoms to increase or decrease?
- Did anyone in the patient's family have similar symptoms?
- The doctor needs a complete medical history. The doctor will review the patient's medical history, including symptoms, lifestyle, exposure to toxins, bad habits, and family history of neurological diseases.
- During a neurological examination, the doctor can check tendon reflexes, muscle strength and tone, the ability to feel certain sensations, and coordination.
The doctor may order an examination
- Imaging or MRI tests can detect various diseases (including tumors).
- Neurophysiology. Electromyography records electrical activity in muscles, which can help determine whether symptoms, including weakness, are caused by muscle tissue damage or nerve damage. ENMG checks the conduction of impulses along the nerves and allows you to determine the degree of damage to the nerve fibers. Neurophysiological studies of the autonomic nervous system may also be performed - sensory tests that record how the patient feels touch, vibration, cold and heat.
- Nerve biopsy. A doctor may recommend removing a small portion of a nerve, usually a sensory nerve, to examine morphological changes in the nerve to determine the cause of the nerve damage.
- Skin biopsy. In this test, a small portion of skin is removed to examine the number of nerve endings. A decrease in the number of nerve endings indicates neuropathy.
- Laboratory research methods are necessary to exclude various diseases, such as diabetes mellitus, autoimmune diseases, kidney disease, etc.
Hereditary polyneuropathy of the lower extremities
Neurologists distinguish polyneuropathies with a known metabolic basis (hereditary amyloidoses, lipid metabolism diseases, porphyrias, diseases accompanied by impaired DNA repair) and polyneuropathies in which the cause of the defect is unknown (hereditary motor-sensory, hereditary sensory and autonomic polyneuropathies, neuropathy with hereditary ataxias and mixed forms of the disease). Polyneuropathy can be inherited in a dominant or recessive manner.
Hereditary polyneuropathies are considered systemic diseases, which are characterized by damage to several organ systems. Metabolic disorders occur in the following hereditary polyneuropathies:
- metachromatic leukodystrophy (impaired cellular metabolism of sulfatides in oligodendroglial cells of the central nervous system and in Schwann cells of peripheral nerves;
- Fabry disease (glycosphingolipidosis);
- atactic polyneuritis-like heredopathy;
- Bassen-Kornzweig disease.
A group of peroneal muscular atrophies (Charcot-Marie-Tooth syndrome) also develops due to family history. Hereditary polyneuropathy of the lower extremities is characterized by the presence of the following symptoms: distal hypotrophy of the legs (in this case, the legs take the shape of “bottles”, turned upside down), as well as bone deformities of the feet with the formation of a high arch and contracture of the Achilles tendons. Patients' legs tremble and sensitivity is impaired.
There is no specific treatment for hereditary polyneuropathies of the lower extremities. Foot weakness can be corrected with bracing or orthopedic surgery. A medical psychologist prepares young patients for the progression of the disease. You can undergo diagnostics and treatment for chronic, autoimmune and hereditary polyneuropathy at the neurology clinic by making an appointment with a neurologist by calling the Yusupov Hospital.
Treatment
The goal of treatment for polyneuropathy is to treat the underlying disease and minimize symptoms. If laboratory tests and other examinations indicate that there is no underlying disease, the doctor may recommend watchful waiting to see if the symptoms of neuropathy improve on their own. If there is exposure to toxins or alcohol, your doctor will recommend avoiding these substances.
Drug treatment
Medicines used to relieve pain from polyneuropathy include:
- Painkillers such as paracetamol or NSAIDs reduce pain
- Medicines containing opioids, such as tramadol (Conzip, Ultram ER and others) or oxycodone (Oxycontin, Roxicodone and others), can lead to dependence and addiction, so these drugs are generally prescribed only when other treatments have no effect.
- Anticonvulsants. Medications such as gabapentin (Gralise, Neurontin) and pregabalin (Lyrica), developed to treat epilepsy, can significantly reduce the pain of neuropathy. Side effects of these drugs may include drowsiness and dizziness.
- Capsaicin. A cream containing this substance (found naturally in hot peppers) can be used to provide some relief from the symptoms of neuropathy. But given the irritating effect of capsaicin on the skin, not all patients can tolerate the effects of capsaicin creams.
- Antidepressants. Some tricyclic antidepressants, such as amitriptyline, doxepin, and nortriptyline (Pamelor), can be used to reduce neuropathy pain through their actions on the central nervous system.
- The serotonin and norepinephrine reuptake inhibitor duloxetine (Cymbalta) and the antidepressant venlafaxine (Effexor XR) may also relieve pain from peripheral neuropathy caused by diabetes. Side effects may include dry mouth, nausea, drowsiness, dizziness, decreased appetite, and constipation.
- Intravenous immunoglobulin is the mainstay of treatment for chronic inflammatory demyelinating polyneuropathy and other inflammatory neuropathies.
- Alpha lipoic acid. Used to treat peripheral neuropathy in Europe for many years. This antioxidant helps reduce symptoms. You should discuss taking alpha lipoic acid with your doctor because it may affect your blood sugar levels. Other side effects may include stomach upset and skin rash.
- Herbs. Some herbs, such as evening primrose oils, may help reduce neuropathic pain in patients with diabetes.
- Amino acids. Amino acids such as acetyl-L-carnitine may help improve symptoms of peripheral neuropathy in patients undergoing chemotherapy and in patients with diabetes. Side effects may include nausea and vomiting.
In addition to drug treatment, other treatment methods may be used.
- Myostimulation allows, to a certain extent, to restore the conduction of nerve impulses through the muscles.
- Plasmapheresis and intravenous administration of immunoglobulin.
- Exercise therapy. If you have muscle weakness, physical activity can improve muscle strength and tone. Regular exercise, such as walking three times a week, can reduce neuropathy pain, improve muscle strength, and help control blood sugar levels. Exercises such as yoga and tai chi can also be quite effective.
- Acupuncture. Impact on biologically active points improves the sensitivity of nerve receptors and reduces pain.
Recommendations for patients with polyneuropathy
- It is necessary to take care of your feet, especially if you have diabetes. You should check your feet daily for blisters, cuts, or calluses. Soft, loose cotton socks and soft boots should be worn.
- You need to quit smoking. Smoking can affect circulation in the extremities, increasing the risk of foot problems and other neuropathy complications.
- Eat healthy. A healthy diet is especially important to ensure that the patient receives the necessary vitamins and minerals.
- We must avoid drinking alcohol. Alcohol can worsen the symptoms of polyneuropathy.
- Monitoring blood glucose levels in the presence of diabetes will help keep blood glucose levels under control and may help improve neuropathy.