Pathogenesis
The factor provoking the development of the disease is:
- bacterial (campylobacter), viral (Epstein-Barr virus, cytomegalovirus, influenza virus) or mycoplasma infection;
- HIV infection, SLE, malignant neoplasms that trigger an autoimmune process, as a result of which the inflammatory process is activated with the formation of immune complexes that damage the nerve sheath or axonal core.
- Pathogenesis
- Classification
- Clinical picture
- Diagnostics
- Differential diagnosis
- Treatment
- Disease prognosis
[/dt_sc_contents]
Classification
GBS with typical clinical manifestations:
- Demyelinating form (about 90% of cases of the disease) – the disease is based on acute demyelination of the roots of the spinal and cranial nerves.
- Axonal form (occurs much less frequently) - damage to nerve axons is typical, the course of the disease is much more severe. It is divided into 2 types:
- acute motor - distinctive feature: only motor fibers are affected.
- acute motor-sensory - a combination of damage to sensory and motor fibers.
GBS with an atypical clinical picture:
- Miller-Fisher syndrome is a variant of GBS characterized by a triad of symptoms: ophthalmoplegia (paralysis of the eye muscles), areflexia (decrease and then loss of reflexes), cerebellar ataxia (impaired motor coordination).
- Acute sensory polyneuropathy is a combination of severe sensory disturbances and increasing sensory ataxia (impaired gait and coordination of movements due to suffering from muscle-articular sensitivity).
- Acute pandysautonomia is characterized by the involvement of both the sympathetic and parasympathetic parts of the autonomic nervous system in the process, resulting in a symptom complex: orthostatic hypotension, impaired gastrointestinal motility up to gastroparesis, neurogenic urination disorders, impaired accommodation and pupillary reactions, disruption of the salivary glands. Violation of sweating, etc.
- Acute cranial polyneuropathy is characterized by the involvement of isolated cranial nerves in the process.
- Pharyngo-cervico-brachial form - characterized by impaired function of the muscles of the pharynx, arms and neck flexors.
- Paraparetic pariant - the lower extremities are affected by the disease, while the upper extremities remain unaffected.
Acute myelitis
The picture of myelitis develops acutely or subacutely against the background of general infectious symptoms: fever up to 38–39 °C, chills, malaise. Neurological manifestations of myelitis begin with moderate pain and paresthesia in the lower extremities, back and chest, which are radicular in nature. Then, within 1–3 days, motor, sensory and pelvic disorders appear, increase and reach a maximum.
The nature of neurological symptoms is determined by the level of the pathological process. With myelitis of the lumbar spinal cord, peripheral paraparesis and pelvic disorders in the form of true urinary and fecal incontinence are observed. With myelitis of the thoracic part of the spinal cord, spastic paralysis of the legs and pelvic disorders in the form of urinary and fecal retention, which turns into incontinence, occur. With suddenly developing transverse myelitis, muscle tone, regardless of the location of the lesion, may be low for some time due to diaschisis. When the spinal cord is damaged at the level of the cervical thickening, upper flaccid and lower spastic paraplegia develop. Myelitis in the upper cervical part of the spinal cord is characterized by spastic tetraplegia, damage to the phrenic nerve with respiratory distress, and sometimes bulbar disorders. Sensitivity disorders in the form of hypoesthesia or anesthesia are always conductive in nature with an upper limit corresponding to the level of the affected segment. Bedsores develop quickly, sometimes within the first days, on the sacrum, in the area of the greater trochanters, femurs, and feet. In more rare cases, the inflammatory process covers only half of the spinal cord, which manifests itself in the clinical picture of Brown-Séquard syndrome.
Forms of subacute necrotizing myelitis are described, which are characterized by damage to the lumbosacral part of the spinal cord with subsequent upward spread of the pathological process, the development of bulbar disorders and death. In the cerebrospinal fluid in myelitis, increased protein content and pleocytosis are detected. Among the cells there may be polynuclear cells and lymphocytes. In liquorodynamic tests, protein is absent. In the blood there is an increase in ESR and leukocytosis with a shift to the left.
The course of myelitis is acute, the process reaches its greatest severity after a few days, and then remains stable for several weeks. The recovery period lasts from several months to 1–2 years. Sensitivity is restored the fastest and first, then the functions of the pelvic organs; motor impairments regress slowly. Often persistent paralysis or paresis of the limbs remains. The most severe in course and prognosis are cervical myelitis due to tetraplegia, proximity of vital centers, and respiratory disorders. The prognosis for myelitis of the lower thoracic and lumbosacral localization is unfavorable due to severe damage, poor restoration of the functions of the pelvic organs and, therefore, the addition of a secondary infection.
Clinical picture
- The first clinical manifestations are often paresthesia (numbness, burning, tingling) and pain in the hands and feet, less often in the mouth and tongue.
- After this, general malaise and low-grade fever develop.
- Next, progressive muscle weakness appears (maximum severity develops by 4-5 weeks), which has a number of features:
- Symmetrical, as with other polyneuropathies.
— Ascending nature (first the lower limbs suffer, then the upper limbs are involved in the process).
— Involvement of facial muscles in the pathological process on both sides in 70%.
- More rare, but at the same time more dangerous, is the involvement of the swallowing and respiratory muscles; Oculomotor disturbances also sometimes occur.
- Weakening of reflexes and their complete loss.
- Autonomic disorders (orthostatic hypotension, supraventricular tachyardia, coldness and chilliness of the hands and feet, acrocyanosis, increased sweating and hyperkeratosis of the soles).
- A sharp decrease to the point of loss of vibration and proprioceptive sensitivity.
You should know that the diagnostic criteria for the disease are symmetrical progressive paresis in the limbs in combination with areflexia, appearing by 4-5 weeks of the disease (although the disease often reaches the peak of its severity by 2-3 weeks).
In favor of Guillain-Barré syndrome, the doctor should also be guided in the diagnostic search by such signs as: progression of symptoms up to 4 weeks, protein-cell dissociation in the cerebrospinal fluid, symmetry of symptoms, the presence of mild sensory disorders, changes in EMG (but it should be remembered that these are not obligate signs of disease)
Phases of the disease:
- The progression phase usually lasts 2-4 weeks and is characterized by an increase in these symptoms. If this phase lasts from 4 to 8 weeks, then the polyneuropathy is called subacute inflammatory demyelinating polyneuropathy. If this phase lasts more than 8 weeks, the disease acquires chronic status.
- The plateau phase lasts from 1 to 4 weeks and is characterized by stabilization of the patient’s condition.
- The recovery phase often lasts several weeks and sometimes months and is characterized by regression of symptoms and restoration of motor function.
Symptoms
Symptoms of Guillain-Barré syndrome initially manifest as general weakness, as well as low-grade fever and pain in the arms and legs. The pain can also be tingling in nature. But still, a distinctive sign of GBS is a clear feeling of muscle weakness in the limbs. Paresthesias occur in the distal parts of both the arms and legs, and in some cases they also occur around the mouth and tongue. Sometimes there is weakness of the facial muscles and other facial nerves, as well as autonomic disorders. Movement disorders initially appear in the legs, and later move to the arms. Sometimes the general symptom complex of this syndrome resembles signs of myopathy .
If, with the development of Guillain-Barré syndrome, damage to the nerves of the bulbar group , then without timely respiratory resuscitation the person may die.
Violations of a vegetative nature are also clearly expressed, which are manifested by chilliness and coldness of the distal parts of the extremities, and the phenomenon of hyperhidrosis. With severe development of the disease, sometimes there is a violation of pelvic functions, which is manifested by urinary retention. This symptom usually lasts from 3 to 5 days.
Acute polyradiculitis usually develops over two to four weeks, after which the person’s condition stabilizes and improves. Not only acute forms of the disease , but subacute and chronic ones . In most cases, we are talking about a favorable prognosis, but sometimes the disease develops according to the type of ascending Landry's palsy , when the paralysis spreads to the muscles of the arms, torso and bulbar muscles.
Diagnostics
- Careful collection of anamnesis for previous infections and vaccinations.
- EMG is not always informative, as it is often within normal limits in the first weeks. Typical changes are:
- in acute inflammatory demyelinating polyneuropathy: decreased impulse conduction speed along motor nerves, proximal type conduction block, increased latency of F-waves.
— about acute sensorimotor axonal polyneuropathy: a decrease in the amplitude of the total action potentials of motor muscles and sensory nerve fibers, signs of demyelization in a maximum of 1 nerve.
- in acute motor axonal polyneuropathy: a decrease in the amplitude of the total action potentials of the motor muscles, sensory fibers remain intact, demyelination is also in a maximum of 1 nerve.
- in acute sensory polyneuropathy: motor fibers are not affected, there is a decrease in the amplitude of the total action potential of the sensory nerves.
- Study of cerebrospinal fluid: protein-cell dissociation. In the first days, however, it is not always possible to detect it, therefore the study of the cerebrospinal fluid should be carried out over time. It should be remembered that false-positive results are possible with intravenous administration of immunoglobulins.
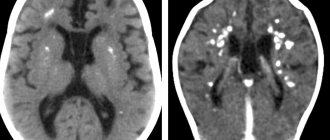
- MRI of the brain and spine allows you to see changes in the roots, but to a greater extent this method is used in the differential diagnosis of tumors and stroke.
- Blood tests: detection of antibodies in the blood
- for acute inflammatory demyelinating neuropathy - antibodies unknown
— for acute motor axonal neuropathy – GM1+GM1b, GD1a
- for acute motor-sensory axonal neuropathy - GM1+GM1b, GD1a
- for acute sensory neuropathy - GD1b
- for Miller-Fisher syndrome - GQ1b.
Differential diagnosis
- Spinal form of poliomyelitis. At the onset of the disease there may be meningeal signs; then asymmetrical flaccid paresis and paralysis develop, a decrease in tendon reflexes only on the affected side, and there are practically no sensory and autonomic disorders. Currently, given the vaccination against polio, the disease is rare and differential. Diagnosis of this disease is becoming increasingly rare.
- Spinal cord tumor. Common with Guillain-Barré syndrome: clinical picture and changes in the CSF. Differences: it often develops gradually, paresis is spastic in nature, pyramidal signs are detected.
- Polyneuropathy in acute intermittent porphyria. It is characterized by the onset of autonomic disorders: abdominal pain, constipation and diarrhea, rapid heartbeat, increased blood pressure. Also with this pathology, mental disorders are observed, such as anxiety, depression, and in more severe cases, delirium and convulsive syndrome. Polyneuropathy is of a peculiar nature: the upper extremities are the first to be involved, starting from the proximal parts; tendon reflexes remain intact longer, and sensory disturbances occur less frequently and are milder in severity.
- Brain stem stroke. The disease often manifests itself with complaints from the head: headaches, dizziness, accompanied by nausea and vomiting, speech impairment. Then alternating syndromes are added, characterized by damage to the cranial nerve on the side of the pathological process and motor or sensory disorders of the limbs and body on the opposite side.
General information
Guillain-Barré syndrome (another name for acute polyradiculitis ) is an acute inflammatory polyradiculoneuropathy, which is manifested by autonomic disorders, flaccid paresis , and sensory disturbances.
As a result of this disease, a person is in a state of complete or partial immobility. Gradually, as the disease develops, a person loses the ability to grasp things with his hands, swallow, lift his eyelids, etc. This disease is relatively rare. GBS is diagnosed in all countries of the world and manifests itself in both adults and children. It develops more often in men, but there is no significant difference in the number of cases of the disease between different sexes.
Treatment
General therapeutic measures:
- Considering the possibility of developing respiratory failure, monitoring vital capacity and respiratory rate is necessary, and it is possible to transfer the patient to mechanical ventilation.
- For swallowing problems with a risk of aspiration, insert a nasogastric tube.
- It is necessary to perform a dynamic ECG, since one of the complications of the disease is disruption of the heart rhythm. In this case, the doctor must be prepared to perform the Valsava maneuver, as well as drug and electrocardioversion.
- In case of urination disorders, bladder catheterization is performed.
Special treatment:
- Intravenous immunoglobulin (IVIG) is the method of choice.
- Plasmapheresis has long occupied a leading place in the treatment of Guillain-Barré disease, however, given the somatic burden of patients, this method is somewhat worse than the previous one due to its more severe tolerability.
The combination of these two methods does not provide a greater therapeutic effect than monotherapy with IVIG or plasmapheresis.