General information about dementia
The popular name for dementia is senile insanity or senile dementia. Most often, this disease occurs against the background of aging of the body and accompanying changes. Dementia usually develops after the age of 65, but due to certain diseases, intoxications or injuries it can appear at an earlier age. Damage to the central nervous system is irreversible; properly selected treatment can only stop the process, but not reverse it.
A mild form of the disease occurs in about one in ten people over 65 years of age, and 5% of older people develop a severe form. It leads to a complete loss of the ability to self-care, as a result of which the patient requires constant care and observation. Women are affected twice as often as men.
Make an appointment
Prevention of disease in old age
It is possible to prevent the development of dementia. Prevention measures are necessary in the early stages, without waiting for old age. Similar advice is given by specialists during the treatment of insanity. Doctors recommend taking care of your mental health after 40 years:
- It is necessary to control blood sugar levels, this will avoid the development of diabetes mellitus, against which dementia often develops. Blood vessels will be healthy and elastic until old age. This will have a positive effect on your well-being.
- Constant monitoring of blood pressure will help avoid stroke and myocardial infarction. It is important to periodically take tests to determine the amount of cholesterol in the blood to prevent the formation of cholesterol plaques on the inner walls of blood vessels and reduce the risk of blood clot formation and artery blockage.
- Bad habits, especially chronic alcoholism, often lead to senile dementia.
- Self-treatment of any mental disorders, even mild forms, is strictly prohibited. Very often, patients prescribe tranquilizers and antidepressants for long-term depression. All drugs aimed at suppressing brain activity can only be taken under the supervision of a doctor.
- Traumatic brain injuries are also becoming a risk factor. You need to protect yourself from various mechanical damage to the brain. If there has been a blow or fall in the past, it is necessary to undergo regular examinations with a therapist in order to prevent and develop the disease.
- Physical activity will help keep the circulatory system in good shape. Daily morning exercises, dancing, walking in the fresh air have a beneficial effect on the entire body.
- Positive emotions should become a habit. Frequent stress and neurosis can provoke changes in the cerebral cortex and nervous system, which complicates the treatment of dementia.
- Proper nutrition is the key to health. Your daily diet should include fish, meat, dairy products, and vegetables. It is necessary to avoid foods that contain preservatives, dyes, carcinogens and refractory fats.
- A proper sleep and rest routine will help keep your cardiovascular system in good shape. You need to sleep at least 8 hours a day.
- Training intellectual activity, meeting new people, learning foreign languages will help to delay as much as possible the moment when senile dementia begins to develop.
- Developmental exercises that train fine motor skills of the hands are very useful not only as a preventive measure, but also in the treatment of the first stage of dementia. Good for appliqué, handicrafts, drawing, modeling, assembling puzzles, and bead embroidery.
Causes
The causes of dementia are diseases and conditions that cause degeneration and death of brain cells:
- Alzheimer's disease;
- Pick's disease;
- severe atherosclerotic damage to the vessels of the neck and brain;
- hemorrhagic and ischemic strokes, as well as transient ischemic attacks;
- arterial thrombosis;
- severe arterial hypertension;
- diabetes mellitus (high blood glucose causes angiopathy - damage to small vessels with subsequent oxygen starvation);
- acute and chronic intoxication (including alcohol);
- neuroinfections (encephalitis, meningitis);
- head injuries (concussions, brain contusions);
- malignant and benign brain tumors.
The presence of dementia in parents or other older relatives significantly increases the risk of developing the pathology. Predisposing factors also include excess body weight and insufficient intellectual functioning throughout life.
Forms of dementia
There are different forms of dementia. They are usually systematized depending on the underlying disease that led to the development of dementia. In this regard, the dynamics of dementia can be different: progressive with progredient processes, regressive with regredient processes, stable or stationary with residual encephalopathy. Some authors distinguish between transient or transient dementia. Often the etiology of dementia is mixed. According to another approach, dementias are differentiated according to clinical and psychopathological characteristics. Let us present a brief description of the main forms of dementia known from the literature (Bleicher, Kruk, 1995); we will report in more detail only on changes in intelligence in patients with schizophrenia and epilepsy.
| | We will help you stop the progression of dementia. Call us or sign up online |
1. Alcoholic dementia - dementia of patients with alcoholic encephalopathy. Usually occurs in connection with severe and prolonged metal-alcohol psychoses - delirium with stunned consciousness, alcoholic encephalopathy Gaye-Wernicke, etc. The development of dementia is facilitated by somatic and metabolic disorders, vitamin deficiency, etc. In old age, dementia intensifies due to the addition of vascular and atrophic disorders. In the structure of alcoholic dementia, euphoria, a somewhat excessive tendency to make contact, and loss of memory mainly for current impressions are often particularly noticeable.
2. Amnestic dementia - dementia in which progressive amnesia and increasing depletion of memory come to the fore in the clinical picture. At the same time, amnestic disorientation is observed. Develops during progressive organic processes affecting the brain. Most often these are atrophic processes (senile dementia, Alzheimer's disease), less often - vascular diseases of the brain.
3. Amnestic-paramnestic dementia - dementia, in the clinical structure of which the central place is occupied by amnesia mainly for current impressions and paramnesia, mainly confabulations - Korsakov's syndrome. It is observed in a number of diseases: cerebral atherosclerosis, the presbiophrenic variant of senile dementia (from the Greek presbis - old, phren - mind, mind and from the Latin senilis - senile), Alzheimer's disease, intoxication and infectious psychoses.
4. Apathetic dementia - dementia with a predominance in the clinical picture of apathy, aspontaneity, and speech reduction. It is especially often observed with organic lesions of the frontal-convexitative localization. This is, for example, the frontal variant of Pick's disease.
5. Apoplectic dementia, or post-stroke dementia , is dementia that occurs as a result of cerebral hemorrhage or cerebral infarction due to atherosclerosis, hypertension, and other vascular processes. The specific clinical structure of the disorder depends on the location, volume of the lesion, the severity of previous vascular pathology and a number of associated factors. Lacunar dementia is more common.
6. Asemic dementia (from the Greek a - prefix of negation, sema - sign) - dementia with a predominance in the clinical picture of focal lesions of the functions of speech, gnosis and praxis. Most often it is a stage in the course of a number of debilitating processes (cerebral atherosclerosis, Pick's disease, Alzheimer's disease, senile dementia, progressive paralysis).
7. Atherosclerotic dementia - lacunar dementia that occurs with non-stroke cerebral atherosclerosis. In unfavorable cases, there is a tendency to transition to global dementia. The clinical structure of dementia is very diverse: dysmnestic phenomena, psychopathic-like disorders, Korsakov's syndrome, pseudoparalytic states; Psychotic, in particular hallucinatory-delusional, disorders may also occur.
8. Infantile dementia - progressive dementia that develops in children after two or three years of age - Heller-Zappert disease (Heller, Zappert, 1909). After a short period of affective disorders (depression, sullenness, tearfulness, aggressiveness), signs of intellectual decline and impoverished speech are revealed. Six months to a year after the onset of the disease, speech stops, patients do not speak themselves, and do not understand the speech of others. Motor skills suffer: movements become monotonous and stereotypical. Sometimes catatonic symptoms, violent laughter and crying, and epileptic seizures occur. Despite profound dementia, the patients' faces retain a meaningful expression.
9. Myoclonic dementia - dementia that occurs with myoclonus epilepsy. The predominance of personality changes of the polar type is typical: patients are either capricious, angry and gloomy, or euphoric and foolish.
10. Subcortical dementia - dementia due to organic processes of subcortical localization (striatum, etc.). A decrease in intelligence is accompanied by extrapyramidal symptoms (stiffness, hyperkinesis, etc.). Characterized by importunity, stickiness of patients or akairia (from the Greek a + kairos - appropriate measure, norm). For example, a patient constantly asks the same question, although he has already received an answer to it and even remembers what was told to him. Mental rigidity, disturbances in the sphere of drives, a decrease in the level of personality, as well as mnestic-intellectual decline, expressed to varying degrees, are typical. The disorder is observed in postencephalitic parkinsonism, Huntington's chorea.
11. Polysclerotic dementia - dementia observed in the later stages of multiple sclerosis. Most often it is presented by pseudoparalytic syndrome in the form of euphoria, carelessness, disinhibition, followed by depression, anxiety; weakening of memory, decreased level of thinking, sometimes delusional ideas of expansive or depressive content.
12. Postanoxic dementia - dementia that arose in connection with postanoxic encephalopathy, that is, in conditions of oxygen starvation, for example, in suicide victims rescued after hanging.
13. Presenile dementia is a collective group of painful conditions, including different types of dementia that occurs in presenile age (Pick's, Alzheimer's, Kraepelin, Jacob-Creutzfeldt, Neumann-Kohn, Huntington's diseases). Typically global dementia with asymbolic manifestations (from the Greek a + symbolon - sign), that is, with symptoms of aphasia, agnosia and apraxia.
14. Dementia with moria (from the Greek moria - stupidity) is dementia observed with organic lesions of the fronto-basal localization. A moderate mnestic-intellectual decline is observed against the background of euphoric elation (“empty fun”) with inappropriate jokes and stupid antics, as well as disinhibition of behavior. The disorder has been described in brain tumors of the frontal region. In the frontal variant of Pick's disease, moria is less pronounced, and rapidly progressive intellectual decline predominates.
15. Tabetic dementia is a characteropathic variant of psychoorganic syndrome with moderate mnestic-intellectual decline, observed with tabes dorsalis. A depressed mood with dysphoria or “flat” euphoria predominates. Profound dementia, as a rule, does not occur. An increase in intellectual deficit with a tendency to transition to global dementia may indicate the addition of progressive paralysis - taboparalysis.
16. Thalamic dementia - dementia observed when organic brain damage is localized in the region of the dorsomedial nucleus of the thalamus optica. Emotional devastation and lack of spontaneity are typical. The disorder in terms of its main manifestations is very similar to frontal convexity disorders.
17. Terminal dementia or mental insanity characterizes the final stage of progressive dementia. It manifests itself as an almost complete and irreversible cessation of mental activity.
18. Traumatic dementia - dementia observed in the residual period of the course of a traumatic disease. Occurs as a result of severe traumatic brain injury with damage to the substance of the brain. The clinical picture of the disorder significantly depends on the location of the main lesion. For example, conditions similar to those of Pick's disease have been described (Gurevich, 1948). The flow is stationary. An increase in signs of dementia usually indicates the addition of another disease: cerebral atherosclerosis, etc. A type of disorder is boxer's dementia, or Martland's syndrome.
19. Choreatic dementia - dementia observed in Huntington's chorea. Typically, characteropathic manifestations (increased excitability), disturbances in the sphere of drives, impoverishment, and then aspontaneity of speech predominate. Asemic symptoms, as a rule, do not occur.
20. Schizophrenic dementia is an ambiguous concept. Patients suffering from schizophrenia may indeed experience dementia of organic etiology, that is, associated with known causes. The frequency of organic forms of dementia in patients with schizophrenia is unknown, the features of the clinical structure have not been virtually studied. It has been established that schizophrenia that occurs in early childhood can cause regression of intellectual level or delay in subsequent mental development. As for schizophrenic dementia itself, there are different opinions on this matter.
E. Bleuler (1920) describes “schizophrenic dementia” as follows: “Schizophrenic dementia receives its characteristic mark, primarily from a disorder of affect; indifference, on the one hand, unbridled passions, on the other; then from a disorder of associations: vagueness and aimlessness, the desire for side paths - leads to insufficient, incorrect, meaningless, strange, ridiculous results.
However, even in severe schizophrenics, many associations still proceed correctly, and although celebris paribus, more complex and subtle functions, of course, are more easily upset than gross and simple ones, the fact that the patient cannot cope with a particular task does not depend on its difficulty. A schizophrenic may not be able to add two-digit numbers and immediately takes the cube root. Severe schizophrenic dementia differs from milder ones not so much in that it affects simple functions as in the fact that the tasks that the patient cannot cope with become quantitatively greater, regardless of whether they are easy or difficult.
The so-called examination of intelligence may give an excellent result, and yet the patient may be completely unable to control himself correctly even in a simple environment. He may be well versed in a philosophical article and not understand that he needs to behave well if he wants to be discharged from the hospital. Where the patient’s complexes are affected, you will not clash with him; he does not feel gross contradictions either in logic or in everyday real ideas. A schizophrenic is not weak-minded in general, but he is weak-minded in relation to a certain moment, a certain constellation, certain complexes.”
K. Jaspers adds to the above that mental abilities in schizophrenia most likely remain unaffected, and “all changes are nothing more than changes in the personality itself.” At the same time, “an inability is also revealed to capture the basic, the most essential - or, at least, what is considered essential in the social, objective, empirically real world. When characterizing patients with schizophrenia, we note the lack of contact with reality - in contrast to patients with progressive paralysis, who, despite severe destruction, manage to maintain some contact with their reality...
The absolute heterogeneity of the organic and schizophrenic varieties of dementia is undeniable: the first is “simply” destruction, while the second is an insane distortion of human nature. In many cases of schizophrenia, we are additionally faced with a loss of spontaneity, a twilight existence that can only be interrupted by strong stimulation, which is surprisingly capable of sometimes generating an appropriate reaction.
Instead of a “general description,” K. Jaspers gives the following illustration of a “relatively mild” case of schizophrenic dementia: “A patient named Nieber is characterized by full orientation, awareness of actions, lively temperament, talkativeness, cheerful disposition, constant readiness for sharp and appropriate remarks; he shows no signs of acute distress.
At a doctor's appointment, he begs to be released immediately; If he is released, he will come to the clinic from time to time. Nevertheless, he goes back to his room without any difficulty and never talks about being discharged again. Instead, he has other plans. He plans to attend the University of Tübingen to work on his doctorate in engineering.
“In it I will outline the plan of my life. I will certainly become a doctor, unless I deliberately make mistakes.” He wants to get hired as a photographer at the clinic; he demands to be provided with several separate rooms; he wants to be looked after to the highest standard, etc.; but he never insists on his demands. Every now and then he takes on more and more new activities, but almost immediately abandons them and forgets about them.
He writes poems, countless petitions, letters to those in power, to doctors, to other hospitals, to titled persons; in addition, he is writing a dissertation: “Closet paper: an impromptu essay by G.J.Nieber.” Let us quote several passages from this voluminous manuscript: “Works have already been written and published on the immortality of the cockchafer, on the dangers associated with firearms, and on the controversial nature of Darwin’s theory of heredity.
So why should recognition and rewards be denied to the work on toilet paper? I believe that the price of 30 marks will not be too high for a whole volume of text. Particular attention will be paid to the social and political aspects of the subject. Therefore, I include in my work a statistical table that will provide invaluable assistance to lower-level politicians when discussing problems of the national economy,” etc.
The patient, with endless diligence, draws a bank check with all the usual patterns and sends it to the address of his former hospital in payment for the food he was fed there: “It seems to me that the sum of 1000 marks is sufficient as payment for the care provided to me, including here doctors' fees." Every now and then he surprises his interlocutors with his usual phrases: “Psychiatry is nothing more than the study of law and its beneficial effects as applied to individuals...”, “I am of the opinion that there is no such thing as mental illness... Psychiatry should give existence to those who born for working life.” There is a temptation to interpret the conversations and behavior of such patients as mockery of others, but in reality there is nothing of the kind. This is exactly how, without any serious efforts on their part, their lives can drag out in hospitals for decades. Another “temptation” may, it seems, appear: to interpret many of the patient’s actions as confirmation of the thesis that he perceives any of his desires, including the absurd, as relating to the world of reality.
G.I. Kaplan and B.J. Sadok, when describing schizophrenia, only mention the dementia of patients with its individual malignant forms and prefer to talk about “personality destruction” instead of the term “schizophrenic dementia.” In ICD-10, the fact of dementia is generally considered as a sign that excludes the diagnosis of schizophrenia.
21. Epileptic dementia is a dementia that develops in some patients with unfavorable epilepsy (20% of patients with temporal lobe epilepsy experience significant personality changes; in 7 hospitalized patients, clear signs of dementia are revealed 20 years after the onset of the disease). There is an opinion that this dementia is not associated with epilepsy itself, since there is no evidence that the degree of intellectual decline depends on the frequency of epileptic seizures (Gastaut, 1975). H. Gastaut believes that dementia in patients is nonspecific; in his opinion, it is not caused by the disease itself, but is associated with cerebral edema and ischemic disorders. Of some importance are probably long-term therapy with anticonvulsants, especially barbiturates, metabolic disorders, as well as repeated concussions in patients with uncontrolled falls at the onset of major seizures. Having observed such patients for a long time, we were able to verify that such falls with significant bodily injuries and possible concussion occur on average up to 10–15 per 10 years. Enechetic personality changes can be observed with tumors and, in general, temporal (temporal) brain damage.
Nevertheless, the role of such a serious pathology as epilepsy cannot be underestimated with regard to significant and, moreover, quite definite changes in personality and intelligence in this disease. Such changes include, for example, difficult-to-formulate viscosity, rigidity (viscosity, stickness), which, as some authors say, conveys the sensations of an impatient listener who does not know how to delicately extricate himself from a drawn-out conversation with a verbose and extremely detailed patient. It is also significant that disorders of the intellect and personality in general represent, in essence, only an intensification of the premorbid qualities of patients, excluding, of course, the final stage of the process with the phenomena of mental insanity. These qualities, as is known, became the basis for the identification of an epileptoid constitution, ictaphine diathesis (from the Greek ictus - seizure, from the Latin affinis - related, from the Greek diathesis tendency, predisposition), glishroidia (from the Greek glykys - sweet, eides - similar) or the enechetic structure of personality. Similar personality traits are also found in blood relatives of patients.
E. Bleuler reports: “Epileptics are usually psychopaths even before the disease leaves a peculiar mark on them. A significant proportion of them, especially in cases with early onset, are directly brain patients and imbeciles. However, epilepsy is characterized by specific mental features, and with the development of the disease they usually intensify. Looking at the degree of development of the disease, we talk about an epileptic character, an epileptic psychopathic constitution, or, in severe cases, about epileptic dementia.” K. Jaspers writes the following: “In other cases - with atherosclerosis, progressive paralysis, severe epileptic dementia - the process in the brain leads to a progressive disorder of the entire complex of mental abilities. Ultimately, the patient completely loses the ability to judge, to differentiate between the main and the secondary; the level of his abilities turns out to be lower than even that of patients with congenital mental defects... The ability for apperception drops to a minimum. The patient is guided by random impressions and is not influenced by opposing ideas; they are deprived of any initiative and ultimately find themselves in a state of severe mental emptiness, in which they can only lead a purely plant-based lifestyle.”
Epileptic dementia, according to E. Bleuler, who gave perhaps the best description of it, is characterized by such characteristic signs that a diagnosis of the disease can be made based on them alone. First of all, attention is drawn to excessive affective excitability and affective viscosity, presented in different proportions and relating to all emotions without exception. “The mood of patients is usually very clearly expressed... and everything unimportant is just as strongly shaded affectively as the essential... we often see a disproportionately strong affective connotation of concepts related to “justice.”
My own self receives special attention.” “All mental functions, especially sharp thinking, are greatly slowed down and clumsy; If we take the flow of speech as a scale, then we can say that they are carried out hesitantly, in jerks. Features of thinking in terms of content appear most clearly in experimental associations: slowness, wretchedness of thoughts, a tendency to repetition in form and content, to definitions, the inability to respond with one word, the frequency of egocentric interpretations, affective emphasis on proposed ideas and the choice of words with an affective meaning for reactions, with a particular preference for words containing an affective assessment (good, beautiful, bad, disgusting), inability to find the right expression with a tendency to clumsy expressions of one’s own invention.” These features of epileptic thinking, as well as excessive thoroughness, a tendency to tautology and perseveration, are complemented by its ambiguity, uncertainty, vagueness of the boundaries of concepts and ideas, and the use of more general ones instead of partial ones.
The same features are characteristic of the speech, writing and graphics of patients. The drawings are oversaturated with details - hypergraphia, figures of speech are florid, helpless and always unclear. The content of the latter is usually everything that directly concerns the patient, his illness, members of his family, his clothes and “heaps of all sorts of small things”, which, if allowed, he willingly carries with him everywhere. Moreover, “all this is mostly carefully wrapped in many pieces of paper and shreds, each bundle is tied with a separate rope, then photographs, letters, decorations that have no price, etc.”
Changes in the personality of patients in a pious environment easily take on religious forms: “Consciousness of one’s backwardness, the need to rely on oneself, to put the well-being of one’s own personality in the foreground, to give ready-made pathetic turns and intense feelings to vague concepts - all this easily conveys to patients, especially in a pious environment, the character of an inflated religiosity and puts all their sorrows and joys into appropriate formulas (“divine nomenclature”).” “Especially characteristic of them is the manner of taking the doctor aside with an important face and mysteriously telling him some trifle or something that everyone knows.”
“Thus, the behavior of an epileptic is outwardly decent, but it quickly tires those around him due to thoroughness, pestering and digging into details.” Patients “are annoying in expressing love and vindictive in the affect of resentment; They do not let go of the offered hand for a long time; If you forget to say hello to them, your mood will darken for a long time. As long as there is an opportunity, they are always doing something, although little good comes out of it; the more feeble-minded are often unpleasant in the department precisely because of their stupid helpfulness; in war, this zeal is reflected in the fact that they are “eager to fight,” they forget about their illness and everyone rushes to the front.
Their inconstancy is very great when they are left to themselves. They take everything very close to their hearts, but... due to mood swings, they cannot settle anywhere; many end up thrown out onto the street. The mood of a given moment also determines their attitude towards the disease; Sometimes it’s very serious, sometimes it gets better or even goes away completely. However, they are constantly running around with their illness, their numerous minor ailments; all this is incredibly important, they talk about all this endlessly in order to arouse sympathy or to brag about how good they feel. In general, “epileptic optimism (Rieger)” predominates; Even the most intelligent patients, despite all the misfortunes and warnings, do not take their illness into account enough, find themselves in dangerous situations, or take on tasks and responsibilities that they in no way can fulfill.”
The thoroughness and stickiness of thinking is sometimes reflected in the actions and behavior of patients: “A healthy person sits down, so to speak, immediately, an epileptic must specially adjust the chair, then he will examine his position in relation to the chair, then he will take the desired position, specially straighten his dress, for example, the tails of his coat, and finally he will sit down.”
The attention of epileptics is characterized by insufficient vivacity, poor switchability and unevenness. Memory gradually deteriorates, but without a specific system; old and new are equally forgotten. In addition, experiences are incorrectly associated, and real illusions of memory often appear. Orientation is mostly intact, except for profound dementia, which few patients reach.
Perceptions are somewhat vague, require more time, are more often than in healthy people, and are erroneous, including due to perseverations. It becomes difficult for patients to master complex relationships, although they cope with simple ones no worse than healthy individuals. For example, the patient is able to notice a slight difference in the length of the lines, but it is difficult for him to understand what is depicted in the artist’s canvas. He fails to follow the rapid turn of speech or the rapid development of the plot in the film. Sometimes there is a big difference in the acquisition of individual words or entire sentences.
The speech of epileptics is often very characteristic: it is slow, hesitant, syllables are often repeated, and speech moves forward slowly (unlike stuttering, there are no convulsive phenomena on the part of the speech muscles). It takes on a melodious character. Individual vowels are pronounced either higher or lower, and minor syllables have the same meaning as the main ones. At the same time, tone modulations are ponderous, rare, without subtle nuances, so that speech also seems monotonous. The mentioned features of thinking and speech can intensify before a seizure, as well as in the post-seizure period.
E. Bleuler illustrates this very complex picture of epileptic dementia with a number of examples.
Here is an observation of perseveration and the inability to transfer speech to another topic C. Wernike: “What is your name?” - "Martha Glockner." - "How old are you?" - "Martha Glockner."
- "Where are we?" - "Martha Glockner." - "How old are you?" - "22 years old". - "What do you do?" - "22 years old". - "Who am i?" - "George's cousin." - “Who is this gentleman?” - "George's cousin."
Another observation concerns thoroughness and a tendency towards tautology: “Dear Mr. Director, I send you my heartfelt greetings and wish you with all my heart good health and God’s blessing, I show you my respect and thank you with all my heart and I wish all this to both Mr. Director and Mr. to the pastor and wish all this and to all your relatives and I ask you with all my heart that you send to Ruti the letter that I gave you that week and to the parents in Ruti I also send my bows from the bottom of my heart, I also show them my respect and thank them them with all my heart and I also wish them with all my heart good health and God’s blessing, both healthy and sick, I really miss home, for its piety and preaching and Bible lessons and all the prayer books were inside me ... "
Another short example from Ulrich concerns the annoying sweetness of patients: “I am the sweet maiden Mrs. XX from XX, community X, canton X, Switzerland.” She would like the doctors to tell her every day that she is a sweet, charming young lady XX; She shook everyone's hand very long and firmly, both left and right. She always wished everyone a sweet good Resurrection, sweet good everyday life, a good good night; when they wished her the same, she answered completely satisfied: “that’s so good.”
In an associative experiment, the poverty of ideas, egocentric relationships, sentimental tone and affective assessment of concepts, as well as awkward and unclear detailed expressions are clearly revealed.
The poverty of ideas is expressed in meaningless associations, grammatical expansion of words, tautologies, etc. Here are the patients’ associations for the proposed words: long - not short; cute - what you like is cute; heart - people; blows - people; sacrifice - there are all kinds of sacrifices; surprise - to be surprised.
Examples of egocentric relationships: desire - health; Naturally, you want to be healthy rather than sick.
Examples of feeling tone and affective evaluations: greenish is a beautiful color; sweet - good; divorce is ugly; youth is joy; beat - beat bad people. Examples of unclear expressions: happiness - joyful or something like that; anger - a person is angry; flower - flowers decorate windows in people's homes, don't they?; spicy - spicy can be made; what they do in stores when they make stone or
anything at all.
Types of pathology
There are several types of classification of senile dementia. The most common is based on the mechanism of development of the disease. The following types of pathology are distinguished:
- Alzheimer's (atrophic): based on a degenerative process in the cerebral cortex, most often found in Alzheimer's disease;
- cerebrovascular: occurs against the background of chronic insufficiency of blood supply;
- mixed.
The location of pathological foci is the basis of the second classification: cortical, subcortical, mixed and multifocal forms of dementia are distinguished.
Clinical manifestations allow us to distinguish two variants of the disease:
- lacunar dementia: mainly the intellectual sphere suffers, memory suffers, but the person is aware of himself and can assess his condition;
- total: loss of self-service skills and inadequate perception of reality.
Dementia in older people
Translated from Latin, the word means “dementia.” The main reason is organic damage to the brain, leading to dysfunction of higher nervous activity. The patient's mental abilities decrease, he cannot perform basic calculations, practical skills and knowledge are lost, and it becomes impossible to acquire new ones.
Our clinic specialists are guided by a complete medical history in the treatment of dementia. The clinical picture depends on the location of the brain lesion, its extent, the prerequisites for the development of the disease, age and general health.
The danger lies in the persistence of the disorder; it only progresses over time. Initially, the defeat affects intellectual activity, then disturbances in the emotional-volitional sphere become noticeable. The final stage is the complete and irreversible disintegration of personality.
Severity
There are three degrees of severity of pathology:
- mild: there is a decrease in short-term memory, emotional instability, inability to remember new things; the person can take care of himself independently and understands the need for treatment;
- moderate: self-care becomes difficult; a person begins to forget about basic actions (close the door, turn off the gas), and may get lost on the way to the store; already at this stage the patient requires constant monitoring;
- severe: complete loss of the ability to self-care and critical perception of reality, the need for constant care.
Stages of dementia
Dementia-related symptoms and signs progress through three stages.
- At the early stage of dementia, the disease often goes unnoticed, as it gradually develops with the following characteristic symptoms: forgetfulness, disorientation, and the patient losing track of time. With significantly impaired social activity, the ability to live independently is preserved, and the rules of personal hygiene are observed.
- The middle stage of dementia progression is characterized by more pronounced signs and symptoms: forgetting the names of people and recent events, disorientation, increasing difficulties in communication, behavioral difficulties - walking aimlessly and asking repetitive questions. The patient requires assistance with self-care.
- Late stage dementia is characterized by almost complete dependence and passivity, a fragmented sense of self, significant memory impairment, difficulty recognizing loved ones, loss of orientation in space and time, difficulty moving, and increased behavioral changes, including aggression. The patient requires constant supervision.
Symptoms
The main symptoms of dementia occur in all forms and types of the disease. They include:
- decreased short-term memory;
- difficulty in perceiving new information, learning new skills (for example, working with a computer or smartphone);
- viscosity of thinking: the patient takes a long time to think, he needs more time to solve any problems or issues;
- speech difficulties: slurred pronunciation, difficulty finding words;
- impaired coordination of movements, especially fine motor skills;
- uncertainty, unsteadiness of gait;
- inappropriate behavior: patients become overly sweet or, conversely, aggressive;
- disorientation in space and time.
Different types of dementia have their own characteristic symptoms. For example, the Alzheimer's type is manifested mainly by mental and memory disorders, changes in thinking, and inappropriate behavior. The vascular form of the disease is characterized by both intellectual and motor impairments, and dementia with Lewy bodies often takes on the character of a psychiatric pathology and is accompanied by hallucinations, delusions, insomnia and depression.
General groups of symptoms
The disease distinguishes two groups of disorders: cognitive and neurological.
Cognitive disorders come to the fore, that is, regression of cognitive and thinking functions.
At the initial stage of the disease, memory is primarily affected. At first these are subtle changes. A person forgets some events, individual names and dates, and cannot find the right word to express a thought. The process of assimilation of new knowledge worsens, and it becomes increasingly difficult for the patient to remember and analyze new information.
Gradually, amnestic symptoms increase. The person does not grasp the meaning of what was said, and it becomes more and more difficult to find words. Because of this, his speech becomes meager, his sentences are short and monosyllabic. If talkativeness manifests itself, then it is incoherent; letters in words can be rearranged, words can be replaced. The person himself does not understand the meaning of what he said. Speech impairment leads to difficulties with writing and reading.
Amnesia occurs in the following forms:
- progressive - the patient begins to forget what happened to him recently, and then earlier events;
- fixation – inability to perceive, analyze, store new material, current events. Consciousness in such patients is preserved; they remember well the events of the past, but cannot remember what they talked about with the person 5 minutes ago. Having bought milk, brought it home and put it in the refrigerator, a few minutes later they are going to the store again to buy it, since they have already forgotten that they purchased it;
- Paramnesia is false memories when the patient supplements reality with unreal events. For example, he may pass off as reality events read in a book or seen in a film, and believe that this actually happened to him. Or he simply fantasizes, passing off as reality what did not happen. It is possible that events may shift in time, that is, what happened many years ago is perceived by a person as having happened yesterday.
In addition to memory, other cognitive functions are affected in vascular dementia. Attention is scattered, it is impossible to fix it for a long time. Perception is disrupted. Thinking becomes inflexible. It is difficult to switch from one activity to another.
Often, as the process progresses, patients develop a symptom such as Korsakoff's syndrome, named after the doctor who first described it. It combines several symptoms. First of all, this is fixation amnesia. As already mentioned, the patient does not remember current events, but retains memory of the past. In this regard, he loses orientation in time and space. So-called amnestic disorientation develops.
There are also various variations of paramnesia: doubts about the occurrence of a particular event, their displacement in time, a mixture of fictional and true events.
Against this background, a person gets lost in an unfamiliar environment. He doesn't understand where he is. While in the hospital, he cannot find his bed, but in a familiar environment, at home, he finds his way around perfectly.
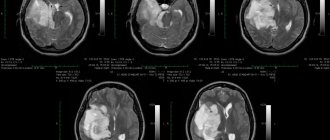
Diagnostics
Neurologists and psychiatrists diagnose dementia. The examination includes:
- collecting complaints and medical history, determining the approximate time of onset of the disease, the most pronounced signs, as well as concomitant pathology;
- detailed neurological examination with assessment of reflexes, motor and sensory function;
- general urinalysis, general and biochemical blood tests, tests for hormones, infections, electrolytes, determination of basic blood clotting indicators;
- ECG, ultrasound of the heart;
- CT or MRI of the brain to detect structural lesions;
- Doppler ultrasound of neck and brain vessels;
- electroencephalogram (EEG);
- neuropsychological tests to assess the state of the psyche and the quality of thinking.
If necessary, a more detailed diagnosis is carried out.
Types of organic dementia
Types of organic dementia are determined by the time of occurrence of the disorder and the degree of its impact on mental processes. The disease is usually classified as residual or progressive. The first is more typical for children, the second for older people.
Residual organic dementia is essentially a residual lesion formed as a result of the impact on the brain of other factors that destroy it: infections, injuries, toxic poisoning. Finding itself defenseless against these problems, the brain begins to deteriorate, but while the root cause is eliminated, the consequences persist forever. They cannot be corrected, but they do not worsen unless other reasons contribute to this. This type of dementia is characterized by dementia and psychopathic-like behavior.
A progressive organic disorder develops slowly, affecting more and more areas of the brain. It is this type that includes the classic version of senile dementia, when mental functions fade away gradually, along with motor functions. It should be noted that, unlike residual, which can stop at one stage of development, progressive will develop constantly until it ultimately leads to the death of the patient.
Dementia treatment
Treatment depends on its type and extent. The main task of the doctor is:
- normalization of the patient's behavior;
- improving the functioning of the central nervous system;
- improving quality of life.
For mild forms of the disease, the drugs of choice are:
- sedatives for excessive anxiety;
- antidepressants to improve emotional state and correct memory;
- means for improving brain activity that improve the conduction of nerve impulses (donezepil and drugs based on it, neuromidin).
Psychotherapy helps slow the progression of the disease in the first stage. The patient is taught special exercises to train memory and logical thinking. With regular exercise, patients become more adapted to everyday life, and the process of degradation slows down.
Moderate dementia requires the use of drugs to protect nerve cells (Actovegin, Cerebrolysin), as well as drugs to restore memory and thinking (Phenibut). Hypnotics or sedatives may be used symptomatically.
For severe dementia, powerful drugs that stimulate brain activity (memantine, rivastigmine) are used. They are taken constantly and allow the patient to maintain a relatively clear consciousness for as long as possible. For aggressive behavior and hallucinations, antipsychotics (haloperidol) are prescribed.
Selecting medications to support a patient with dementia is a complex task that requires constant interaction between the doctor, the patient and his relatives.
Make an appointment
Types of dementia depending on the cause
- Atrophic type of dementia
– with primary degenerative processes in nerve cells at its core. Dementia of the Alzheimer's type is a progressive dementia with pronounced signs of atrophy of the cerebral cortex. Histological examination reveals the presence of characteristic changes in neurons - plaques and neurofibrillary tangles. Memory impairment is the leading and earliest symptom. There are variants of this type of dementia: presenile (formation occurs in the fifth or sixth decade) and senile (in the seventh or eighth decade of life). Semantic dementia, called primary progressive dementia, is another type of dementia associated with cortical atrophy. It has special symptoms: speech impairment occurs, with the replacement of words, similar consonances, while speech remains smooth, but meaningless. When the left hemisphere is damaged, prosoagnosia develops - loss of the ability to recognize faces. When the right hemisphere is damaged, anomia develops - the patient cannot name an object. Another type of dementia associated with atrophic changes in the cerebral cortex is Pick's disease (a type of frontal or frontal temporal dementia) - Vascular type of dementia (atherosclerotic)
- with the secondary development of degeneration of the central nervous system, develops as a result of pathological circulatory disorders in the vessels of the brain. The most common cause is arterial hypertension and cerebral atherosclerosis. Initially, neurosis-like emotional disorders develop, and later memory impairment is added. Multi-infarct dementia, a common cause of which is arterial hypertension, with the formation of numerous small infarcts of varying duration in the brain, is also associated with a vascular factor. Men over seventy years of age are more likely to get sick. The onset of the disease is characterized by emotional distress, depression, and the presence of hemiparesis - unilateral disturbances of movement and sensitivity. Memory impairment develops later. - Idiopathic type of dementia
is a type of presenile (presenile) dementia with an unclear cause. - Epileptic type of dementia
- develops against the background of diseases such as epilepsy and schizophrenia, with characteristic cognitive impairment and disorder in the emotional-volitional sphere. Epileptic dementia is affected by the severe course of the underlying disease with long-term use of antiepileptic drugs, injuries during seizures, and hypoxic damage to neurons during status epilepticus. Characterized by a narrowing of the range of interests, viscosity of speech and thinking. Symptoms of behavior are selfishness, hypocrisy, servility and sweetness, combined with quarrelsomeness, rancor and cruelty. - Traumatic type of dementia
. If the cause is a single, severe traumatic brain injury, dementia may not progress. Repeated and frequently repeated injuries can cause the formation of progressive dementia with symptoms of parkinsonism. - Alcohol-induced dementia
is caused by long-term toxic effects of alcohol on the brain. The development of the disease is facilitated by vascular pathologies and endotoxin poisoning with liver damage, hepatic encephalopathy. At the third and final stage of alcoholism, all alcoholics exhibit atrophic changes in the brain and personality degradation is noted. In the case of complete abstinence from drinking alcohol for six months or more, regression of signs of alcoholic dementia and some smoothing of organic defects are observed. - Drug-induced dementia
is a toxic type of dementia that develops as a result of long-term use of large doses of medications in an unfavorable combination. Sleeping pills, antidepressants, antiarrhythmic and antihypertensive drugs have the greatest risk of developing dementia, which is reversible in these cases. - A type of dementia caused by multiple sclerosis, a severe neurodegenerative disease in which the myelin sheath of nerves is destroyed
. The development of dementia can be affected by the unfavorable course of the disease and the lack of adequate treatment at the last stage of the disease. Multiple sclerosis affects young people, so dementia develops at a relatively young age.
Caring for a person with dementia
Having a relative with advanced dementia is a real challenge. The behavior and well-being of the patient depends on the behavior of the people around him, which is why it is important to devote a sufficient amount of time to care. To maintain a relatively stable patient's condition, it is recommended:
- organize a clear, understandable and stable daily routine;
- involve a person in family life and communication as much as possible;
- constantly stimulate thinking: solve crosswords, play chess, read and discuss what you read;
- give small tasks around the house so that the patient feels important and useful;
- avoid conflicts, violence, bullying, and excessive care.
As dementia progresses, it is recommended to make your home as safe as possible by removing any dangerous objects and securing heavy furniture. The patient needs constant observation and control, since he can harm himself or get lost simply by leaving the house. Severe degrees require constant care: feeding, hygiene procedures.
Causes of dementia
Scientists believe that in the modern world, dementia can occur in anyone, regardless of age. And yet there are people who are at risk. These include:
- elderly people (dementia is very common among older people and is called “senile insanity”);
- people who have relatives with serious illnesses accompanied by dementia (Alzheimer's disease, Huntington's chorea);
- patients suffering from diabetes;
- persons who are overweight;
- patients suffering from sluggish chronic hypoxia;
- everyone who moves little and does not perform even the simplest physical exercises.
According to recent research, there are approximately seven million people with dementia around the world every year. It is expected that this number will increase in the future. To date, dementia cannot be completely cured. You can only slightly slow down the development of the disease or prevent its occurrence. It is important to diagnose the disease in time, as well as to identify its cause. This will help patients with this disease feel much better and return to their previous lives.
We recommend
“Dementia in older people: symptoms and treatment” Read more
Prevention
Prevention of dementia helps not only to prevent the development of this pathology, but also to slow down the progression of the process that has already begun. Doctors recommend:
- be promptly examined and treated as necessary;
- avoid excess body weight;
- stop smoking and drinking alcohol;
- regularly engage in amateur sports to maintain tone (walking, swimming, yoga, etc.);
- eat properly and balanced, drink enough clean water;
- avoid stress, physical and mental fatigue;
- engage in mental work regularly.
Treatment at the Energy of Health clinic
Neurologists at the Energy of Health clinic offer the most effective treatment and prevention methods for senile dementia today:
- reliable drug regimens that are selected on an individual basis;
- course treatment using intravenous infusions (droppers) in a day hospital;
- Psychiatric consultations and psychotherapy;
- training in home prevention and patient care.
We will conduct a full examination of the patient to identify concomitant pathologies and select medications with a minimum number of contraindications, as well as organize spa treatment if necessary.
Signs and symptoms of organic dementia
Since dementia develops in stages, its first symptoms are often missed by both the patient and his loved ones. Attention should be paid to the appearance of the following signs of the disease:
- Changes in behavior, namely increased impulsiveness, irritability, aggressiveness.
- Forgetfulness, at first very mild, is perceived as fatigue (the patient forgets his keys, loses his glasses, forgets to call, and so on).
- Decreased interest in what is happening around, giving up hobbies.
- Deterioration in performance, some drowsiness (these signs are also attributed to fatigue and stress).
- Absent-mindedness, inability to perceive and remember new information.
- Apathy, depression.
- Lack of a critical attitude towards yourself and your appearance.
Since symptoms do not appear all at once, but gradually, it is very difficult to detect the period of onset of the development of organic dementia. Especially if the patient lives away from young relatives. Naturally, in this case, seeking medical help comes quite late, when several brain structures are affected.
Advantages of the clinic
The Health Energy Clinic provides qualified medical care in various areas. We offer each patient:
- screening diagnostic examinations;
- targeted diagnostics using modern equipment and laboratory research;
- consultations with experienced specialists who regularly improve their skills, as well as foreign experts;
- individual selection of complex treatment;
- disease prevention activities;
- organization of sanatorium-resort treatment according to indications;
- own day hospital for course treatment.
Senile dementia turns the life of a person and his family into a real hell. Do not allow the disease to progress. Sign up your loved ones for an examination at Health Energy and let our specialists choose the most effective treatment.
Treatment and care
In the modern world, numerous drugs are being studied in various stages of clinical trials for the treatment of dementia. Unfortunately, there is currently no therapy to cure or change the course of the disease. Comprehensive treatment of dementia is aimed at stabilizing the process and reducing the severity of existing symptoms. Treatment should be carried out for hypertension, atherosclerosis, diabetes mellitus, obesity - diseases that aggravate dementia. Much can be done to support and improve the lives of people with the condition and their carers.
The main goals of medical care for dementia are: whenever possible, early diagnosis and prevention of the development of the disease; as well as measures to optimize the patient’s physical health, activity, and maintenance of mental perception processes. It is necessary to identify, treat and correct comorbidities, behavioral and psychological symptoms. Provide information and long-term support to carers.