Hospitalization and treatment under the compulsory medical insurance quota. More details after viewing the pictures.
Brain tumors can be benign or malignant; the latter are aggressive in nature and pose a significant threat to life. Neoplasms form inside the skull due to abnormal disturbances in the cellular genetic apparatus, which leads to uncontrolled growth of tissue structures. Atypical cells are formed from normal ones as a result of mutations, exposure to physical, chemical or other factors. These can be various cells of brain tissue, for example, neurons, glial cells and others. Often, metastasizing cells formed from cancer of other organs enter the brain, which leads to the formation of secondary malignant tumors. The main treatment involves surgical removal of pathological foci, additionally radiation and chemotherapy are prescribed, as well as drugs to relieve negative clinical manifestations.
Causes of tumors
At the moment, medical science does not fully understand the reliable causes of the formation of cancer. Doctors name factors that increase the risk of tumor formation. An important role is played by the age and gender of a person. Some types of cancer, such as meningiomas, are more often diagnosed in women over 45-50 years of age. This is due to the characteristics of the female endocrine system and hormonal levels. For example, during pregnancy, some neoplasms progress more intensively. Brain tumors in men, as a rule, have a more severe course and complex prognosis, because in this case the tumors are highly malignant.
Other provoking factors include:
- adverse environmental impacts: radiation, hazardous industries, living in contaminated areas, etc.;
- constant contact with toxic elements;
- infection with viruses that can contribute to the development of cancer;
- genetic characteristics (the presence of certain genes in the human genome that increase the risk of developing a brain tumor);
- head injuries of various nature and origin;
- treatment with drugs, for example, hormones, chemotherapy;
- bad habits;
- consumption of low-quality food saturated with carcinogenic elements.
These factors can influence the formation of diseases both separately (for example, heredity) and in combination.
Classification
Given that cancer cells in the brain do not migrate or grow to other parts of the body, it is not possible to stage brain cancer using the conventional classification system (TNM). It is also difficult to divide by stages because sometimes a tiny tumor can cause much more harm than a large one (depending on its location).
In this regard, it is customary to distinguish I, II, III and IV degrees of malignancy. The lower the degree, the greater the chance of recovery.
Stage 1 brain tumors are best treated. Stage 3 and 4 brain cancer often recurs, meaning the disease comes back. In addition, stage 4 neoplasms form their own blood vessels, due to which they grow and multiply even faster.
Types of tumors
Neoplasms that form in the brain can be:
- Benign – tumor tissue does not contain cancer cells. Neoplasia of this type is characterized by clear edges and slow growth. They are much easier to treat surgically, but can become malignant, that is, turn into cancer;
- Malignant tumors contain abnormal cells that can divide uncontrollably and metastasize to other organs. In this case, the disease is difficult to control; in the later stages, surgery is impossible. Treatment in this case is difficult, has a high cost and, as a rule, poor prognosis.
Brain glioma
Glioma
This type of tumor is diagnosed more often, accounting for approximately 60% of all types of cancer that form in the brain. The tumor is formed from glial cells. In most cases, this is a primary neoplasm, most often formed in the area of the chiasmata or ventricles, but it can also affect the brain stem; pathogenesis rarely extends to the bones of the skull, however, in rare cases this is possible. The size of gliomas is usually up to 14 cm. Metastases are rare, growth is usually slow, but due to penetration into adjacent tissues, the boundaries of the lesion are difficult to distinguish.
Three varieties are known
- astrocytoma – diagnosed more often than others (it accounts for about 50% of gliomas);
- oligodendroglioma – up to 10% of cases;
- ependymoma – less than 7%.
According to the World Health Organization classification, there are 4 stages of glioma:
- The first stage is benign. It is characterized by slow growth. Example: giant cell astrocytoma.
- Second stage. Features: borderline malignancy with slow tissue growth, easily progresses to stages 3 and 4. In this case, only one symptom of cancer is identified - cellular atypia.
- Third and fourth stage. In this case, the tumor has all the signs of cancer, for example, necrotic changes in glioblastoma multiforme.
Brain astrocytoma
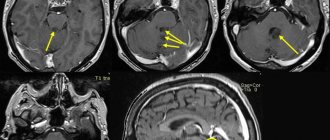
Removal of a large GRADE II WHO astrocytoma of the right temporal lobe (before surgery)
This malignant neoplasm of varying degrees of aggressiveness is diagnosed quite often. The beginning is given by degenerated glial cells - astrocytes (hence the name - astrocytoma). There are:
- Common astrocytomas: protoplasmic, fibrillary and hemisrocytic.
- Special astrocytomas: cerebellar, piloid, microcystic and subependymal.
Astrocytomas are distinguished by the stage of malignancy:
- The first stage (benign tumor) includes piloid or pilocytic astrocytoma of the brain.
- Second stage of malignancy: fibrillary tumor is also an ordinary neoplasia, second degree of malignancy.
- The third stage is already cancer. It includes anaplastic astrocytoma of the brain.
- The most life-threatening are glioblastomas (giant cell glioblastoma and gliosarcoma), which are classified as stage 4 and are characterized by rapid growth and the ability to metastasize.
In addition to the ones mentioned, there are other types of astrocytomas, for example, ependymoma (develops from ventricular cells), oligodendroglioma (forebrain) - grow quite slowly without the formation of metastases, and glioma of the brain stem.
Meningioma of the brain
Removal of a large middle cranial fossa meningioma before surgery
Pathogenesis begins with pathogenic cells in the superficial membrane that surround the brain tissue. The neoplasm is oval in shape, grows slowly, and is therefore considered benign. Meningiomas are diagnosed in 15% of cases (of all brain tumors). The risk of degeneration into cancer is about 3-4%. The clinical signs that appear are caused by increased intracranial pressure and tissue compression. With malignancy (degeneration of somatic cells into carcinogenic ones), meningiomas become aggressive. Usually more than one lesion forms and may spread to the spinal cord. After surgical treatment, there is a high probability of relapses. As a rule, pathology is diagnosed by chance, because symptoms appear only when the lesion reaches a large size. There are no early signs of the disease.
Note. Meningiomas often form in females.
Other types of brain tumors
There are quite a lot of types of neoplasms. Here are some of those that are diagnosed relatively often (besides those mentioned above):
- medulloblastoma is a brain cancer that originates from the structures of the cerebellum;
- germinoma - formed from germ cells, most often it is detected in the first half of a person’s life;
- Craniopharyngeoma - develops in the pituitary gland at the base of the brain;
- Shawnoma – formed from degenerated Schwann cells;
- tumors in the pineal gland area.
Diagnosis of the disease and methods of treatment of giant meningioma of the anterior cranial fossa
Relying solely on symptoms alone, one cannot talk about the specification of this disease, and therefore additional research into the patient’s condition is simply inevitable in this situation. Moreover, any neurosurgeon will directly insist on conducting additional research, on the basis of which it is already possible to draw certain conclusions regarding the presence of meningioma in this practice, and not a banal inflammatory process.
Typically, the neurosurgeon will want to perform an MRI scan of the head. The results of this make it possible to localize the disease, find out about its size and talk about its prospects. For example, vision loss can be caused by fouling of the optic nerve, and changes in the social behavior, character and criticism of a person with this disease are explained by swelling and compression of the frontal lobes of the brain, respectively.
Thus, only a detailed study using computed tomography of the brain allows us to talk about drawing up a competent further treatment strategy. It is worth noting that in most cases there is a need for a surgical solution to such a problem through surgical excision. In rare cases, a small part of the tumor may be left in order to avoid fatal bleeding and to ensure that the optic nerves and other important parts of the brain responsible for the proper functioning of the human body systems are not damaged during the operation.
After the operation, there may be complications in the form of paralysis, paresis, and so on, but the neurosurgeon must warn his patient about this in advance during the study. If there are no such risks and the surgical intervention is performed efficiently, then there will be no negative consequences. After the operation, the patient must undergo a repeat MRI analysis to evaluate the result obtained from the surgical intervention of surgeons in the field of neurology.
Clinical manifestations
Symptoms are usually divided into general and focal. In the latter case, the symptoms depend on where the tumor forms.
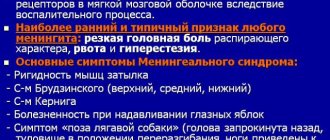
General symptoms
The clinical picture is caused by an increase in pressure inside the skull and the toxic effect of metabolites of pathogenic cells on healthy tissue. Common signs include:
- headache not relieved by conventional analgesics;
- various visual impairments, for example, fog, doubling, glare, decreased visual acuity and others;
- loss of appetite, poor health, nausea and vomiting that are not caused by food poisoning;
- changes in the usual emotional state: mood swings, depression or aggressiveness, and others;
- symptoms of an epileptic nature;
- weakening of the brain: it is difficult for a person to concentrate, mental activity is disrupted, there is a loss of concentration, memory problems, etc.
Important. Early signs of cancer are often misunderstood by sick people. They seek help when clinical signs significantly impair quality of life. In this case, the brain tumor is diagnosed late, which significantly complicates treatment and worsens the prognosis.
Focal symptoms
Signs of this type arise due to changes in the functioning of cerebral structures, so the clinic depends on the location of the neoplasm:
- when the hemispheres are damaged, tactile sensitivity decreases, muscles in the opposite part of the body weaken (in the presence of pathogenesis in the right hemisphere, problems arise on the left side);
- disease in the temporal lobe leads to a deterioration in the ability to speak, memory suffers, and the perception of smells changes;
- pathological changes in the cerebellum lead to disturbances in gait and coordination of movements;
- damage to the frontal lobe causes mental and cognitive changes;
- neoplasia in the parietal lobe changes tactile sensations and fine motor skills;
- damage to the occipital zone negatively affects vision, and hallucinations are possible.
Important. The presence of these signs (of any type and intensity) is a good reason to seek medical advice. Early detection of pathologies improves the prognosis of treatment.
Symptoms of cerebral aneurysm
As we previously noted, in most cases the aneurysm does not become clinically apparent until the acute phase of rupture occurs. But when the lesion is large in size, when the lesion seriously puts pressure on nearby structures and disrupts the transmission of nerve impulses, neurogenic symptoms are usually felt. Since a cerebral aneurysm puts a person’s life at risk, it is important to identify it in the early stages, but the trouble is that no one even thinks of going to the hospital if there are no or minimal complaints.
Doctors urge every adult, especially after the age of 35, to undergo diagnostics of cerebral vessels at least once a year for their own good.
Now let’s voice all the possible clinical signs that generally begin to worry when there are dangerous volumes of an unruptured defect, when the cranial nerves are affected:
- pain in the eye area, decreased or blurred vision;
- hearing disorder (decreased, sensation of noise),
- hoarseness of voice;
- numbness, weakness, pain along the facial nerve, usually on one side of the face;
- muscle spasm in the neck (inability to touch the chin to the chest);
- skeletal muscle cramps;
- weakness in an arm or leg;
- decreased sensitivity, impaired tactile perception in certain areas of the skin;
- problems with coordination;
- dizziness, nausea;
- unreasonable drowsiness or, conversely, insomnia;
- inhibition of movements and mental activity.
To exclude or determine pathology, immediately undergo a targeted medical examination if you notice at least one symptom!
Diagnostics
The initial examination involves an oral interview and a physical examination. The doctor assesses the patient’s general condition, determines the nature of clinical manifestations, their duration and intensity, evaluates coordination, reflexes, psycho-emotional state, and so on. Next, the patient will have to undergo a thorough diagnosis, which may include the following types of studies:
- general blood and urine tests;
- blood chemistry;
- Ultrasound (echoencephalography);
- angiography - X-ray contrast study of the condition of the blood vessels of the head;
- examination of eye function and level of vision;
- computed tomography or magnetic resonance imaging – obtaining high-precision layer-by-layer images, which allows you to identify all the nuances of the disease and determine the method of tumor removal;
- magnetic resonance spectroscopy – study of the functioning of pathogenic tissues at the biochemical level;
- positron emission tomography (PET) of the head shows the characteristics of metabolic processes in the painful focus, which makes it possible to talk about the rate of development of the disease;
- biopsy - tissue collection for histological examination; in this case, the material is obtained after tumor removal.
Also of great diagnostic importance is the study of cerebral fluid, in which pathological cells are located. The stereotactic biopsy method is the most informative in terms of determining the type of carcinogenesis and its characteristics.
Brain tumor removal
Therapy for neoplasms is complex, always complex and quite expensive. For example, in Russia, surgical treatment of a brain tumor is estimated at approximately 350 thousand Russian rubles. You can find out the final cost of treatment in one of the best oncology centers in the Russian Federation after consulting a neurosurgeon. Prices abroad are much higher. In Germany, for such therapy you will need to pay about 28,000-30,000 US dollars, in Israel it is several thousand cheaper, so it is important to take this fact into account when choosing a clinic. You need to pay attention to the nuances. For example, the equipment in foreign clinics is often better, although the treatment methods and results are not fundamentally different, but in the event of an unfavorable outcome, Western specialists will not have to deal with paying local insurance, so they easily take foreign patients who pay for everything themselves.
Note. The main treatment is a radical surgical operation; other methods used in combination act as auxiliary ones (chemotherapy, radiotherapy and other methods).
Brain cancer can only be removed through surgery. It is performed for nodular tumors and is impossible for diffuse neoplasms due to deep infiltration into nearby structures. In such circumstances, brain tumor surgery is performed to remove some of the abnormal tissue, relieve pressure inside the skull, and prevent dropsy. The size of the tumor and the stage of the cancer play a decisive role in deciding whether to remove the tumor.
Radiotherapy involves repeated exposure of cancer cells to radiation, which leads to blockade of division and death of the latter. With significant doses of radiation, pathogenic cells stop developing and most of them die.
At the same time, treatment involves the use of chemotherapy through oral and intravenous administration of cytostatics (toxic substances for pathogenic cells). These therapies have many negative effects. Recently, medicine has been producing more and more unique chemical drugs that selectively target tumor cells, which can significantly reduce the negative impact of poisons on the body.
At the same time, medications are prescribed to eliminate unfavorable signs that can be caused by both the tumor and side effects from the proposed treatment.
Surgery
Surgeries to remove tumors in the brain are the only effective treatment. This type of treatment is very complex. The possibility and effectiveness of the operation depends on many factors, among which important are the stage of cancer, the nature of the spread of pathogenic tissues, the presence of metastases and secondary foci, as well as the localization of pathogenic formations in brain tissue.
Any neurosurgical operation is quite complicated, because the doctor must remove a malignant tumor located between healthy brain tissue. Therefore, treatment of this kind is traumatic, and in some cases impossible. For example, cancer removal is not carried out if the tumor is large, when it affects vital parts of the brain, or if the disease is at a terminal stage. In addition, the person’s health status, the presence of chronic diseases, their stages, the patient’s age and other features are taken into account.
In each specific case, the choice of technique and method of tumor removal is selected individually. At the moment, doctors have a lot of specialized surgical equipment in their arsenal, for example, tomographs, laser and ultrasound equipment. This significantly increases the efficiency of operations to remove tumors.
Most often, surgical removal of brain cancer involves trepanation and resection of the skull. The methodology is as follows:
- At the beginning of the operation, the surgeon dissects the skin layers above the cranial vault (a scalp incision is made).
- After turning away the cut skin, the doctor moves the muscle layers aside.
- At the next stage of the operation, the required part of the bone tissue of the skull is removed so that the brain tumor becomes accessible for manipulation.
- Then the pathological focus is excised and the extracted bone tissue is installed in its original place (this is called trepanation). If part of the skull is not returned to its original place, then such an operation is called resection.
- At the final stage of the operation, the soft tissues covering the skull are restored and sutures or staples are applied.
After resection, the hole in the skull is closed with a special material or mesh. Removing pathogenic tissue reduces intracranial pressure, freeing up space for swollen tissue afterwards. In addition, craniotomy is necessary if the tumor process has spread to bone tissue. After removal, the extracted biological material is sent for histological analysis.
Symptoms of astrocytoma
The trigger for the development of a tumor can be various factors, but the exact causes of the disease are unknown. Clinical signs of the disease directly depend on the location of the formation, its type, as well as its pressure on surrounding tissues.
All symptoms of astrocytoma are divided into two categories: general and local. In the first case, clinical signs appear due to increased intracranial pressure, and local ones associated with the direct effect of the tumor on brain tissue. In the initial stages of cancer, the symptoms are not so pronounced, but as the tumor grows, the following ailments appear:
- headache of varying intensity and character;
- dizziness;
- convulsions;
- tremors in the arms and legs;
- nausea, vomiting not associated with food intake;
- decreased memory, attention;
- mental disorders, hallucinations;
- speech disorders;
- decreased sensitivity in the limbs;
- deterioration of vision, hearing and smell;
- sudden weight loss;
- frequent mood swings, increased irritability.
All symptoms of the disease can manifest themselves with varying intensity, but in any case, at the first signs you should immediately consult a doctor. The main and, perhaps, the first sign of cerebral astrocytoma is headache. At first, it may bother you intermittently, often at night or during the day. Then the pain syndrome intensifies, the nature of the pain is compressive, throbbing, and can affect part or all of the head.
With a benign tumor and its slow growth, symptoms develop slowly, but with malignant tumors, the person “fades away” in a short period of time.
The location of the tumor will play an important role in the clinical picture of the disease:
- Frontal lobe – frequent mood swings, unsteadiness of gait and tremors, paresis of facial muscles, decreased sense of smell.
- Temporal lobe – memory impairment, hallucinations, stuttering, problems with thinking.
- Parietal lobe – decreased sensitivity in the legs and arms, difficulties with motor skills.
- Cerebellum – instability, mental disorders;
- Occipital lobe – decreased visual acuity, hormonal disorders, hallucinations.
Brain astrocytoma is a dangerous neuroectodermal tumor, so its symptoms significantly affect the functioning of the nervous system and the body as a whole. Having studied several types of brain cancer, it is safe to say that the symptoms are very similar to each other, so to determine the type of cancer, it is important to undergo a comprehensive examination. The results will help confirm or exclude a terrible diagnosis.
Life forecast
Without surgery, treatment of malignant tumors is ineffective, and the prognosis is extremely negative. After removal of a tumor, life expectancy depends on the stage, level of malignancy, type of carcinogenesis and the degree of its germination into other structures. As a rule, after partial removal of the tumor, brain cancer comes back again, so surgery in this case prolongs the patient’s life for a very short time. The patient will live no more than a year if the relapse is aggressive, and only 25% of patients will live more than two years. After removal of the pathological focus at the first stage of malignancy, life expectancy in 80% of patients is estimated at more than 5 years (in the case of complete removal of carcinogenic tissue). The most dangerous are the late stages of the disease. The prognosis for life at the quadruple stage is not very encouraging - a person will not live longer than a year.