Lennox-Gastaut syndrome
Symptomatic Lennox-Gastaut syndrome, as a rule, debuts against the background of an existing lag in mental and mental development. In the cryptogenic form, the development of the child at the time of manifestation of the syndrome corresponds to the norm. LGS is characterized by a large variability of attacks, their varying duration and frequency.
Atonic paroxysms
caused by short-term loss of muscle tone. With their generalized nature, the child falls, the so-called. "drop attack". Local paroxysms can take the form of sudden bending of the knees, objects falling out of hands, nodding the head, etc. A distinctive feature of atonic episodes in LGS is their lightning speed and short duration (up to 5 seconds). Generalized atonic paroxysms of LSH require differentiation from attacks of myoclonic-astatic epilepsy, fainting, and stroke.
Myoclonic paroxysms
represent local muscle twitching. Most often it affects the flexor muscles of the proximal arms; when it spreads to the lower extremities, a fall occurs. They are characterized by symmetrical serial occurrence in both limbs and stereotypy. Need differentiation from myoclonus in tick-borne encephalitis and toxic lesions of the central nervous system; non-epileptic myoclonus, which is characterized by irregular asymmetric myoclonus that occurs in response to various sensory stimuli (sound, light, touch) and is not accompanied by EEG changes.
Tonic paroxysms
DES often occur during sleep and are distinguished by their short duration (average duration 10 seconds). Accompanied by a loss of consciousness. They may be generalized in nature or manifest themselves in the form of tonic tension of individual muscle groups (posterior cervical, dorsal, abdominal muscles, shoulder girdle, etc.). Tonic paroxysms are accompanied by tachycardia, facial cyanosis, lacrimation, apnea, and hypersalivation. Minimal local paroxysms of a tonic nature can sometimes be difficult to differentiate from yawning or stretching.
Atypical absence seizures
associated with partial impairment of consciousness. They manifest themselves as temporary “numbness”, lack of any physical activity. With a short duration, absence seizures are often not recognized by people around the child. With LPH, absence seizures can be accompanied by muscle hypotonia (atonic absences) and hypertonicity of the back muscles (retropulsive absences). More often than other types of epilepsy, Lennox-Gastaut syndrome is accompanied by absence seizures—absences that continuously follow each other. This non-convulsive epistatus usually occurs upon awakening and can last several hours or days.
Psychomotor development delay
(ZPR) is noted in almost all cases of LGS. Its severity depends on the form of the syndrome (cryptogenic or symptomatic), the nature of the background pathology of the central nervous system, the severity and frequency of epileptic paroxysms. As a rule, problems with learning new skills and mastering new information come to the fore. Aggression, hyperactivity, emotional instability, and character traits characteristic of autism are often observed. About 50% of adolescents with Lennox-Gastaut syndrome do not have self-care skills. Another 25% are socially and emotionally maladjusted due to severe mental retardation. Features of behavior and character do not provide the opportunity to adapt normally in society even to those patients whose mental retardation is mild. Normal social adaptation is observed only in 15% of cases.
Reasons for appearance
The etiology of the disease has not been established to date. In medicine, it is generally accepted that this disorder is symptomatic. This means that it only indicates the presence of genetic abnormalities, but there is no substantiation of this hypothesis. Factors that increase the risk of developing Lennox-Gastaut syndrome in a child have been precisely identified:
- Intrauterine infections: bacterial and viral. If the mother is ill during pregnancy, there is a high risk of damage to the fetus. Since the active formation of the child’s nervous structures occurs during this period, diseases such as rubella, toxoplasmosis or common herpes can harm the baby’s health.
- Fetal hypoxia caused by disturbances in the development of the placenta, immunological problems and other damaging factors. This condition can also develop in the first years of life, since even healthy children periodically suffer from apnea - stopping breathing, usually occurring during sleep.
- A common cause that provokes the development of Lennox-Gastaut syndrome at two to three months of age is birth trauma. They may have different mechanisms of negative impact. In severe cases, deformations of the skull and spine, hemorrhages, and hypoxic phenomena occur, which often accompany the entanglement of the umbilical cord around the child’s neck.
- There is a genetic disease that is directly associated with this form of childhood epilepsy. This pathology is called tuberous sclerosis and is a hereditary problem that causes disorders of the nervous system. The disease is a common cause of seizures.
Treatment methods
There are no effective treatments for Lennox-Gastaut syndrome. Therapy is designed to bring the disease under control and reduce the intensity of clinical manifestations. Surgical treatment methods are also used, which are also not highly effective.
Drug therapy
The main goal in the fight against Lennox-Gastaut syndrome in children and adults is to reduce the frequency of seizures. For this, antiepileptic drugs such as Carbamazepine and Phenytoin are used. They have a pronounced effect only in 15% of cases. However, their use is associated with the risk of worsening the patient’s condition. Felbamate has a more pronounced effect, although it belongs to the same antiepileptic group of drugs. It allows you to monitor the patient's condition, but the use of the medicine is limited. This is due to serious side effects that occur with prolonged use. Drugs that are derivatives of valproic acid are effective. They allow you to stop attacks, but their effect is too short-lived.
Neuroprotection is promising in the drug control of many types of epilepsy, including Lennox-Gastaut syndrome. This is a fairly young method, which is currently being actively studied in models and animals. The technique, although only effective against a few aspects of the complex cascade of reactions that occur in the brain during a neurological disorder, is considered extremely promising in preventing the unpleasant consequences of paroxysms. Antiepileptic drugs have a certain protective effect on nerve cells. However, neuroprotection should be aimed at other parts of the pathogenesis. The main idea is to influence the mechanisms that trigger hyperactivity of cerebral structures, and not to suppress it.
So far, research has focused only on epilepsy of post-traumatic origin, since its nature is most clear. In the future, treatment of Lennox-Gastaut syndrome may focus not on the use of antiepileptic drugs, but on the use of drugs that reduce the negative effects of free radicals. Medicines from the group of NMDA receptor antagonists are also promising.
Surgical intervention
Surgical treatment of Lennox-Gastaut syndrome is based primarily on callosotomy. This procedure involves cutting the corpus callosum, a structure that connects the hemispheres of the brain. This action leads to a significant improvement in the condition of 40% of patients. Callosotomy does not cure the disease, but only prevents the spread of pathological excitation during an attack, which allows one to avoid falling during a paroxysm.
One of the new methods of treating the syndrome is the installation of a vagus nerve stimulator. Such operations are already being carried out, but their effectiveness is being studied. Callosotomy has had great success to date. At the same time, stimulation of the vagus through the installation of a special electrical device is associated with a lower risk of developing problems, especially those associated with weakening of mental abilities.
Nutritional Features
Very often, along with other therapeutic methods, the ketogenic diet is used. It represents a decrease in carbohydrate intake and an increase in fat intake.
In addition, foods with a low glycemic index are recommended, i.e. those that lower blood sugar levels. These include: fruits, vegetables, legumes, whole grains, skim milk.
During such a diet, the doctor should monitor the possibility of reducing the doses of medications taken.
Surgery
If there is no positive effect after drug therapy, surgical treatment is performed using various methods:
- Implantation of a vagus nerve stimulator . It is performed by sewing into the collarbone a special device with an electrode that transmits electrical impulses to the vagus nerve. This method can reduce the number of seizures. As practice shows, in more than half of patients, thanks to this method, the frequency of attacks is noticeably reduced.
- Implantation of an RNS stimulator under the scalp, which generates electrodes in the brain area. Electrodes continuously record the electrical activity of the brain, and at the onset of an attack, the stimulator delivers electrical impulses that suppress the epileptic focus.
- Callosotomy is a dissection of the corpus callosum, which is a bundle of nerves that connects the hemispheres of the brain and transmits epileptic impulses from one part of the brain to another. After the operation, the attacks do not disappear completely, but become less intense, because impulses are not generated from one hemisphere to the other. This treatment is usually used in cases of uncontrolled epileptic seizures.
Prognosis and possible complications
Most patients with Lennox-Gastaut syndrome die in childhood due to injuries during attacks. This is due to the low effectiveness of currently available treatment methods. That is why the prognosis for the disease is unfavorable. Even if the patient can be stabilized, he is assigned a disability. Such a person needs constant help and regular use of symptomatic medications. In adulthood, the syndrome is associated with the occurrence of other neurological disorders. Patients also have an increased chance of developing autonomic disorders, which can be fatal.
Diagnostics
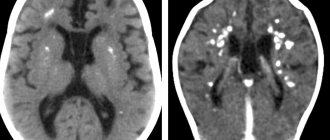
To confirm the disease, a comprehensive examination is required. Since the first symptoms are registered in infancy, a careful collection of family history is necessary. The neurologist examines the patient to determine the intensity of clinical manifestations. An important method in diagnosing the disorder is electroencephalography (EEG), which allows assessing brain activity. During seizures, the results are specific, although during periods of normal well-being, deviations in the functioning of the central nervous system are noted. This method is also used to distinguish pseudo-Lennox syndrome from nocturnal tonic seizures, which have similar symptoms.
Since the disorder is often symptomatic, it is important to identify the organic basis of the problem, which takes an active part in the pathogenesis. For this, visual methods are used, such as computed tomography and magnetic resonance imaging. PET is also used, which makes it possible to characterize the metabolic activity of the brain. However, this method only allows one to register deviations in the process of using the nutrient substrate by nerve cells. At the same time, the nature of the disorders in Lennox-Gastaut syndrome is different. In some areas of the brain, increased glucose metabolism is detected, in others, on the contrary, it is reduced. In some cases, there may be no PET abnormalities at all.
The final diagnosis is made after all the necessary studies and based on the collected family history.