Neuromuscular diseases
This is a group of hereditary diseases that are transmitted at the genetic level (X-linked, autosomal dominant, autosomal recessive forms, maternally inherited mitochondrial forms). About a third of disease cases are the result of new mutations. Taking into account the structural organization, the following levels of damage to the neuromuscular system are distinguished:
- Primary muscular lesions (muscular dystrophy of Duchenne, Becker, myopathy, myotonia).
- Synaptic lesions (neuromuscular transmission disorders - myasthenia gravis).
- Neuronal lesions (spinal muscular atrophy).
TREATMENT
Treatment depends on the cause of the pathology. Non-steroidal drugs (local, tablet or injectable) are often prescribed, which eliminate inflammatory processes and anesthetize tissues.
For infectious diseases, antiviral, antiparasitic or antibacterial drugs are used. In the autoimmune form, drugs that suppress the immune system (glucocorticosteroids or cytostatics) are used. To strengthen the defenses, complexes of vitamins and minerals are prescribed.
Non-drug therapy plays a special role in treatment. This includes:
- massage (there are contraindications);
- physiotherapy;
- physiotherapy (electrophoresis, magnetotherapy, amplipulse therapy).
SYMPTOMS OF NEUROMUSCULAR DISEASES
The main symptom of neuromuscular diseases is muscle weakness. The clinical picture depends on the affected area (shoulder girdle, hips, pelvis, lower extremities, facial muscles, respiratory muscles). Depending on the form of the disease, muscle weakness and increased fatigue during physical activity develop, muscle atrophy / pseudohypertrophy, fasciculations appear, tendon reflexes are inhibited , gait is disturbed, special motor techniques appear when getting up from a lying or sitting position. Neuromuscular diseases occur in stages. A neurologist will help determine the stage of development of pathological processes using medical diagnostics.
SYMPTOMS OF THE DISEASE
Muscle tissue diseases are disorders of the working condition of an individual muscle or an entire group caused by various reasons and locations. As a rule, muscle tissue diseases have common symptoms.
- sharp or dull (aching) pain in the disease area (neck, shoulder girdle, lower back and others);
- increased pain when pressing, leaving a state of rest (when getting up in the morning), physical activity;
- redness and swelling of the skin in the area of the disease;
- detection of swelling or nodules in the muscles;
- muscle weakness, which is accompanied by dystrophy (shrinkage);
- pain and difficulty in performing simple everyday movements (turning the head, nodding, bending the body).
DIAGNOSTICS
The diagnostic task is to establish the level of damage to the neuromuscular system, establish the cause and determine whether there is a specific treatment.
- Electroneuromyography and electromyography. Diagnostic methods help determine primary and secondary myopathy. Also assess the degree of damage to the spinal cord and peripheral nerves.
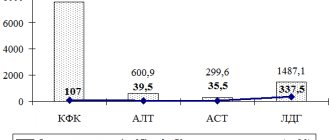
- Laboratory tests. A clinical and biochemical blood test is required to determine the level of electrolytes, protein, lactate, CPK, ALT, AST, myoglobin and thyroid hormones.
- Muscle biopsy with pathomorphological examination of muscle tissue. The diagnostic results help to establish an accurate diagnosis (Duchenne, Becker muscular dystrophy), which is important for selecting the correct therapy.
- Molecular genetic diagnostics is the most informative diagnostic method, which is prescribed for neuromuscular diseases.
- Magnetic resonance imaging of the brain and cervical spine.
- An electrocardiogram (ECG) evaluates heart rhythm.
- ECHO CG reveals hypertrophic, dilated cardiomyopathy.
TYPES OF MUSCLE DISEASES
Muscle diseases are divided into groups that have a similar occurrence, characteristic manifestations, course and treatment methods.
Diseases include:
- myasthenia gravis – muscle weakness due to autoimmune processes;
- myalgia – pain in muscle tissue due to cell spasm;
- myositis - inflammatory processes that occur against the background of infections, parasites, and other causes);
- Rhabdomyolysis is a serious disease that develops due to the destruction of skeletal muscle and the release of myoglobin (protein) into the blood.
TREATMENT OF NEUROMUSCULAR DISEASES
As for treatment, there is no specific therapy. The therapeutic approach is based on creating the prerequisites for successful rehabilitation and providing high quality general and specialized care.
- Drug therapy. The goal is to compensate for the energy deficiency of muscle tissue, improve tissue metabolism and peripheral circulation. Myotropic drugs and anabolic steroids are used. In the case of Duchenne muscular dystrophy, glucocorticosteroids are used. In the case of myasthenia gravis, anticholinesterase drugs are used. For secondary damage and/or dysfunction of the central nervous system, courses of neuroprotective and neurotrophic therapy are carried out. Drug therapy for bulbar and pseudobulbar disorders.
- Physiotherapy. The goal is to correct metabolic disorders, improve neuromuscular conduction, normalize muscle tone, and prevent the development of contractures.
- Physiotherapy. The goal is to prevent the development and correction of contractures of the limbs, maintain motor activity, improve muscle tone, delay the development of atrophies, and prevent complications caused by inactivity. Teaching the patient how to use assisted sitting and standing devices.
- Orthopedic correction.
- Early detection of swallowing disorders (dysphagia) and the possibility of drug correction (together with ENT doctors, based on the results of nasopharyngoscopy - the functional state of the epiglottis, the presence of regurgitation, and in older children + analysis of the results of an X-ray contrast study of the act of swallowing).
- Neurological assessment of respiratory function (ENMG analysis of the phrenic nerves + ultrasound of the diaphragm, analysis of respiratory function, pulse oximetry and capnometry, mechanics and type of breathing, ECHO data, ECG with a cardiologist’s conclusion).
Neurological examination of patients for respiratory failure makes it possible to clarify its causes, reversibility of disorders and the degree of their compensation. In the case of an established dependence on mechanical ventilation, work in a team of doctors to create a multifunctional therapeutic program that is aimed at improving physical condition and restoring normal life functions. choice of treatment methods and their order (medication and non-medication, including management of respiratory support parameters, breathing exercises, physical therapy, physiotherapeutic techniques, psychological assistance, etc.).
MYALGIA
Pathology of muscle tissue, accompanied by acute or dull spastic pain, both in a tense state and at rest, is called myalgia. Soreness can be of different origin and intensity, it can intensify and subside. It usually occurs due to an inflammatory process in the fibers.
Myalgia - symptoms and treatment
The disease can occur as a result of foreign factors, the effects of which the body itself cannot overcome:
1. External causes - high or low temperature, strong pressure on muscles, bacteria, fungi and viruses, ultraviolet radiation, exposure to heavy metal salts or acids.
2. Internal causes - complications of diseases of internal organs.
Myalgia is a disorder that affects not only older people, but also children. Only a doctor can diagnose and determine individual therapy. If you do not consult a specialist in a timely manner and the disease develops, then from an acute form it can become chronic (permanent).
Treatment of myopathies
Currently, there is no pathogenetic therapy for most myopathies, but methods of gene and cell therapy are being developed, and for myopathies associated with storage diseases, therapy is being developed to replace enzyme deficiency in the body. For some diseases, treatment is already available. These include Pompe disease.
In addition to pathogenetic treatment, symptomatic therapy is carried out. It includes various classes of drugs that enhance metabolic processes, increase muscle strength, and support the normal functioning of the nervous system, brain, heart, and digestive organs3.
Non-drug treatment includes a number of therapeutic techniques aimed at improving the quality of life and socialization. These include physical therapy, physiotherapy, psychological rehabilitation, massage, and others.
The prognosis of hereditary myopathies can be different. Timely diagnosis is extremely important.
References
- Antelava O.A., Nasonov E.L. Modern approaches to the classification criteria of idiopathic inflammatory myopathies // Scientific and practical rheumatology - 2007. - T. 45 - No. 5 - P. 41–46.
- Sparks SE, Escolar DM Congenital muscular dystrophies // Handb. Clin. Neurol. Elsevier. 2011; (101):47–79.
- Kurushina O.V., et al. Modern approach to the diagnosis and treatment of primary and secondary myopathies // Bulletin of the Volgograd State Medical University - 2021. - No. 1. -P. 16–22.
- MSD Manual Professional Version. Congenital Myopathies. 2021. URL: https://www.msdmanuals.com/professional/pediatrics/inherited-muscular-disorders/congenital-myopathies (accessed: 04/04/2019).
- Fedotov V.P., Ryzhkova O.P., et al. Miyoshi myopathy: diagnosis of a familial case of dysferlinopathy // Neuromuscular diseases - 2021. -T. 6 – No. 1.
- Zhdanova E.B., Kharlamov D.A., Belousova E.D. Somatic disorders in progressive Duchenne muscular dystrophy // Russian Bulletin of Perinatology and Pediatrics – 2011. – T.56 – No. 5.
- ACMG Working Group on Management of Pompe Disease AWG on M. of P. et al. Pompe disease diagnosis and management guideline. // Genet. Med. Various. 2006;8(5):267–288.
- Skoromets A.A., Kazakov V.M., Rudenko D.I. Facioscapulohumeral muscular dystrophy and its connection with facioscapulohumeral muscular dystrophy. History, clinical picture, genetics and differential diagnosis. Litres. 2021.
GZEA.PD.18.09.0435b
Skeletal muscle biopsy
Very often, when visiting a doctor, a person talks about muscle weakness and fatigue as symptoms of a disease, and it is important to figure out what is the direct cause of these symptoms. muscle biopsy plays a critical role in the evaluation of patients with neuromuscular diseases , often being the gold standard for diagnosis . Muscle biopsy is recommended for patients with these symptoms, as well as for various systemic diseases, diseases of the nervous and muscular systems, diabetes mellitus, thyroid dysfunction, athletes, as well as elderly people who often develop inflammatory reactions . It is especially important not to miss the corresponding symptoms in children. Effective diagnosis is the first step to solving the problem: conducting a muscle biopsy in our laboratory, which meets international standards, is a unique opportunity that will not only make a diagnosis, but also select an effective treatment and clarify the prognosis of the disease.
DETAILED DESCRIPTION:
Taking a biopsy is a surgical procedure, and despite the fact that it is relatively simple and does not pose a risk to the patient, the biopsy must be taken in a specialized institution in compliance with certain rules for storing the material taken, so that the pathologist can optimize the research process.
The study of a biopsy of skeletal muscle tissue is a complex process that includes classical histological stains (hematoxylin and eosin, Gomori stain modified for muscle tissue, PAS reaction, Van Gieson stain, Sudan stain, etc.), histoenzyme-chemical methods (detection of mitochondrial enzyme activity), immunohistochemical studies to identify specific proteins (dystrophin, sarcoglycans, myosin, actin, dysferlin, merosin, collagens, calpain, caveolin, major histocompatibility complex-I and some others), as well as electron microscopy for assessment of the biopsy at the ultrastructural level.
Thus, the full range of studies includes a complex of classical histological stains, immunohistochemical examination and electron microscopy. Conducting a full range of studies that meet international standards is a unique opportunity that our laboratory can provide. Making a diagnosis takes into account data from all of these methods, which requires extensive experience and deep knowledge from the pathologist. Despite all the complexity, the results of muscle biopsy analysis in our laboratory will be ready within 2-3 weeks . The most important advantage of our laboratory is the ability to carry out these studies at a time, since the laboratory is equipped with the necessary equipment that meets international standards and has specialist experts in the field of neuromuscular diseases. The laboratory offers consultations in English .
In addition, the laboratory has the possibility of a minimal set of studies , in which our specialists perform only immunohistochemical analysis to confirm the clinically suspected diagnosis, as well as the possibility of a consultation between a neurologist and a pathologist on your case, which is the best option, since it allows you to select a personalized algorithm research and further treatment.
A muscle biopsy can help determine the immediate cause of the disease, as a number of diseases can cause muscle weakness and muscle pain. Among them are diseases of the nervous system, connective tissue, vascular diseases and the musculoskeletal system. Timely diagnosis of the process allows you to choose effective treatment.
The following are the most common diseases, the diagnosis of which is based on a biopsy of skeletal muscle tissue:
Muscular dystrophies are a very wide range of genetically determined diseases in which muscle is destroyed and replaced by connective tissue. To determine the specific type of muscular dystrophy, immunohistochemical studies are required in combination with clinical and radiation diagnostic methods at the Neurology Center.
Metabolic, toxic, mitochondrial myopathies are muscle diseases associated with a deficiency of certain enzymes/caused by the toxic effects of various substances (including medications), or damage to mitochondria.
Myositis is an inflammatory muscle disease of various nature. Muscle biopsy is indicated primarily for those that are classified as inflammatory idiopathic myopathies (polymyositis, dermatomyositis, myositis with inclusion bodies).
Neurogenic atrophy is damage to motor neurons that causes muscle atrophy.
Congenital (structural) myopathies are a large group of hereditary diseases that usually debut in the form of a nonspecific myopathic symptom complex at different ages (from neonatal to adult).
PREVENTION OF MUSCLE DISEASES
Preventive measures include a number of simple rules:
- avoid hypothermia, wear seasonal clothing;
- carefully follow all doctor’s orders for any disease;
- do not self-medicate;
- practice a healthy lifestyle;
- use regular exercise.
It is best to practice under the guidance of experienced instructors who will select an individual rehabilitation program and help you achieve a quick and high-quality recovery. This is the approach that the specialists at the Center for Restorative Medicine follow. The cost of admission and other details can be found on the Center’s website or by calling.
Certain types of myopathies: clinical picture and features
Distal Miyoshi myopathy is the most common distal form, although the exact number of patients cannot yet be determined. It has an autosomal type of inheritance. The main clinical signs are progressive muscle weakness and atrophy of individual muscles. Most often the disease manifests itself in adolescence, occasionally after 40 years. The feet and legs are primarily affected.
Typical complaints at the beginning of the disease manifestation are difficulties when standing on your toes, weakness when walking on your toes. Soon the calf muscles begin to atrophy, sometimes greatly decreasing in volume in just a few days. Gradually, weakness appears in the muscles of the back of the thigh, buttocks, wrists, and fingers. The disease progresses slowly, and disability usually occurs several decades after the first signs appear5.
Duchenne muscular dystrophy is one of the most common inherited forms. Inherited in a recessive, X-linked manner. It develops only in boys. Symptoms appear between 2 and 5 years of age. Clinical signs - fatigue, difficulty climbing stairs, frequent falls, progressive muscle weakness, atrophy - muscle tissue is replaced by fibrosis or fatty tissue. Children develop hyperlordosis of the lumbar spine and contractures of large joints. Internal organs are affected. Patients lose the ability to move independently at 7-13 years of age6. Duchenne muscular dystrophy is characterized by a very high level of CPK (cretin phosphokinase), above 2000 U/l.
Pompe disease is a rare progressive neuromuscular disease transmitted in an autosomal recessive manner. It is associated with a deficiency of the lysosomal enzyme alpha glucosidase, as a result of which glycogen accumulates in cells, so the disease is classified as a lysosomal storage disease. The disease is characterized by progressive degeneration of skeletal, respiratory, and, mainly in infants, cardiac muscle tissue. Pompe disease can develop at any age, including adults. The main manifestations are muscle weakness, muscle atrophy. This leads to gait disturbance, difficulty walking, climbing stairs, and hyperlordosis. Respiratory symptoms are manifested by shortness of breath with minor exertion, frequent infections of the upper respiratory tract and lungs. Pompe disease is one of the few hereditary pathologies for which replacement therapy has been developed to slow the progression of the disease and improve the quality of life of patients7.
Distal Nonaka muscular dystrophy is inherited in an autosomal recessive manner. Symptoms begin in the 20s and 30s with damage to the tibialis anterior muscles. After a few years, the function of the foot is impaired, then the thigh muscles and iliopsoas muscles are affected. It becomes difficult for patients to climb stairs or get out of a chair. Soon weakness of the flexors of the neck, shoulder girdle, and hands occurs. 13 years after the onset, patients are unable to move independently8.