Choroid plexus cyst in fetus and adult: causes, symptoms
Choroid plexus cyst (CPC) in the fetus and newborn is an ultrasound term formed due to excess accumulations of cerebrospinal fluid along the vessels. In most cases, as the baby grows, the formations go away on their own. If the structures are preserved, they do not pose a danger to the child's health. If the structures are preserved, they do not pose a danger to the child's health. Only in rare cases is surgery required to remove an overgrown cystic cavity.
The optimal period for diagnosing formations is the fetus at 18-22 weeks, when the structure of the brain is formed. Repeated ultrasound at 24-28 weeks notes a decrease in the number of cystic cavities.
Choroid plexus cyst in the fetus - what is it?
CSS is dangerous in children with chromosomal abnormalities such as Edwards disease (trisomy 18). The nosology is characterized by multiple malformations, so intracerebral cavities with cerebrospinal fluid are a minimal problem in treatment.
Down's disease is not characterized by the formation of the cerebral coronary artery system.
Interesting facts about choroid plexus cysts in children:
- Spontaneous disappearance in 90% of fetuses by 28 weeks of development;
- The prevalence rate of nosology among pregnant women is 2%;
- The shape, size, number of cavities varies;
- Found in adults and healthy people;
- The frequency of villous and choroid plexus cysts is about 3%.
It is impossible to determine the initial type of formations in the fetus due to physiological degradation. The absence of pronounced symptoms does not allow doctors to accumulate enough information about the pathology.
Morphological structure of choroid cystic cavities in a child
The accumulation of cerebrospinal fluid inside the choroidal formations does not pose a threat to the health of the baby. Morphologically, the cavity is represented by a thin wall, capable of changing size and shape.
Vascular plexuses are early structures in the formation of the central nervous system of the fetus. Bilateral localization is due to the presence of two hemispheres that require the content of cerebrospinal fluid. Scientists were unable to explain the need for the formation of limited cavities around the plexuses. Presumably, the structures are part of the formation of the central nervous system, and therefore disappear by 28 weeks. If development slows down, CSS can be observed in newborns, infants 3 months and somewhat older.
Cystic cavities of the brain are sometimes observed in adults. The pathology does not produce clinical symptoms, so they are detected by chance on an MRI performed due to the verification of another etiology.
Practice shows that there is no health hazard in the persistence of choroid plexus cysts after 30 weeks, with the exception of Edwards disease.
Origin
The choroid plexuses are derivatives of the pia mater, which are localized in the ventricles of the brain. During embryogenesis at week 4, 3 brain vesicles are formed from the neural tube:
- front;
- average;
- diamond-shaped with internal cavities.
The walls of their cavities are lined with a layer of ependymal cells, and the blisters themselves are filled with cerebrospinal fluid (the contents of the future cyst). Blood vessels grow through the cells of the ependyma (the future pia mater) and ensure its protrusion into the cavity of the brain vesicles, where folds of cells form. The choroid plexuses are formed in the following order:
- 4-5 weeks – network in the fourth ventricle;
- 6-7 weeks – network in the third ventricle;
- Weeks 7-9 – lateral ventricles.
Thus, based on the characteristics of the formation of choroid plexus cysts, we can conclude that they do not belong to typical cystic formations (they are regarded as a congenital malformation).
Causes of CSS
The etiology has not been established. It is considered likely that cystic cavities will persist for a long time against the background of viral infections, herpes, or complicated pregnancy. The absence of clinical manifestations until the end of a person’s life indicates the absence of harm from the pathology. The formations require dynamic monitoring. Blind fontanelles in a child allow an ultrasound of the skull to be performed, and periodic MRI is recommended for adults.
Viral cysts can change: they grow, they degenerate. Dynamic observation determines the prognosis of consequences for a person with CSS.
Two different diagnoses should be distinguished: “fetal choroid plexus cyst” and “cerebral vascular cyst”. The first nosology is harmless, goes away on its own or persists without dynamics for many years. The second type is dangerous, as it sometimes provokes symptoms.
There is a definition of “pseudocyst”. On the screen of an ultrasound monitor, doctors can detect a cavity formed by physiological structures.
The exclusion of pathological conditions after the diagnosis of “choroid plexus cyst” in a newborn and fetus is ensured by an additional comprehensive examination. Genetic counseling rules out Edwards disease. Magnetic resonance imaging shows the structure of the soft tissues of the brain with high resolution, three-dimensional modeling of the area under study.
Detection of a choroid plexus cyst in a child requires verification of provoking factors: viral and bacterial infections, changes in the composition of the cerebrospinal fluid, increased intracranial pressure. If there are no additional changes, it can be argued that there are no conditions for the negative development of a vascular cyst.
Treatment
Not required in 95-98% of cases. Only monitoring of the child's condition is indicated.
If clinical manifestations occur, medications may be prescribed:
- Antiviral agents – for laboratory-confirmed herpes virus (Acyclovir).
- Drugs that reduce intracranial pressure (diuretics) – if signs of hydrocephalus occur (Spironolactone).
- Anticonvulsants - they are prescribed not only when an epileptic focus has formed in the brain, but also when there is pronounced activity of the neural network (pre-epileptic state).
- Weak sedatives – for increased excitability (Glycine).
- Antioxidant complexes and nootropics - to restore metabolic processes in the brain and normalize blood circulation.
All these groups of drugs are used only to eliminate symptoms.
Choroid plexus cysts of a newborn baby
Detection of CSS after birth is not a dangerous condition, but requires examination of the newborn baby. Herpetic infection is activated when the immune system is weakened and can cause changes in the choroid plexus. As the baby grows, the immune system strengthens, so after 3 months, active development of immunity is observed. A decrease in viral activity stabilizes the condition. Cystic cavities can be observed in infants in the absence of clinical pathology. According to the standard scheme, children are examined three times:
- 3 months;
- 6 months;
- 12 months.
The absence of progression indicates the absence of changes that will contribute to the development of dangerous conditions.
Left choroid plexus cyst in a child
The choroid plexus is formed in the fetal body quite early. Education takes part in the formation of cerebrospinal fluid, which provides nutrition to the brain.
The diagnosis of left plexus cyst is common in newborns, although bilateral localization is more common. Pathology develops before the age of 1 year, when intrauterine infections are present. Cystic cavities are equally likely to form in any part of the brain.
Choroid plexus cyst of the right lateral ventricle
The nosology is considered the most benign, since most variants disappear on their own. Found after 22 weeks. An ultrasound scan after 28 weeks shows no pathology. The cystic cavity of the right ventricle can resolve. If there is no associated pathology (with damage to other ventricular spaces), this location of the cyst will not cause complications throughout life, even if the nosology persists in the child after 1 year. In adults, the nosology is rare.
Bilateral choroid plexus cysts
The pathology can persist into adulthood. Some cavities disappear, some remain. Despite the bilateral location, no clinical symptoms occur. Dynamic observation can reveal an increase in size and a change in shape. Only then is conservative treatment carried out. Chromosome mutations are preliminarily excluded. Geneticists can identify a genetic predisposition to Edwards disease. True, pathology can be determined without consulting on the external symptoms of the nosology, characterized by multiple malformations.
Ultrasound examination every 3 months allows you to monitor the condition of the brain parenchyma in infants. The procedure is sufficient to obtain information about the degradation or progression of cystic cavities.
Small cystic cavities in a child's brain
The nature of the CSS has not been reliably established. The pathology is an incidental finding. Small lesions do not affect the human psyche or metabolic reactions. There is no metabolic disorder, so there is no danger.
Small plexus and vascular cysts should be differentiated. The latter option provokes some symptoms. There is no threat to life or health. In adults, minor hemorrhages may occur, soaking into surrounding tissues.
Intrauterine infection provokes inflammatory damage to the walls of the cavity. Detection of infection requires the prescription of antibacterial drugs.
Detection of a plexus cyst at 19 or 20 weeks is not a reason for parents to worry. A repeat examination at week 29 will show no cavities.
Most scientists consider a cystic plexus of intracerebral vessels to be normal. The absence of a clinic suggests that the nosology is a variant of the norm. Improvements in diagnostic methods have made it possible to detect the disease in fetuses and infants more often.
You should pay attention to late cyst formation, which is the result of infection with herpes and a number of other viruses.
Relationship with other pathologies of intrauterine development. Does she really exist?
In medical literary sources, you can find information that there is some connection between the presence of choroid plexus cysts and some congenital pathology caused by a genetic mutation. Moreover, the localization of the cystic cavity on the right, left or both sides at the same time has absolutely no significance. But here it is very important to remember that it is NOT a cyst that provokes developmental anomalies, but on the contrary - a violation of intrauterine development contributes to the formation of vascular cysts , therefore the connection between them is limited only by the presence or increase in the number of choroid plexus cysts and that’s all. Nothing more. Such genetic defects, when a cystic cavity is diagnosed more often than usual, include trisomy 18, known as Edwards syndrome (non-disjunction of the 18th pair and the addition of another chromosome 18 to it, so instead of the normal two, there are 3 of them, and the entire genotype of such an embryo is represented by 47 chromosomes). By the way, it is believed that trisomy 21 (Down's disease) has a much smaller effect on the increase in the incidence of choroid plexus cysts than trisomy 18.
In addition, it is important to note that in the case of other pathology, the primary role does not belong to the cyst, but to the deviations that it accompanies, for example, the same Edwards syndrome, so its significance here is reduced to zero.
Thus, a choroid plexus cyst, no matter right or left, is single or represented by several small formations:
- Equally safe;
- Doesn't play any role;
- Does not participate in any important processes;
- Incapable of growing and being reborn.
Pregnant women should know about it so as not to be afraid and not to be confused with other cystic formations that have similar names, but a completely different genesis and location.
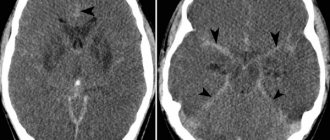
Bilateral choroid plexus cysts on MRI images
Symptoms of choroid plexus cysts
A brain cyst in adults can be a consequence of a hematoma. Limited accumulation of blood (subdural, epidural) with penetration into the ventricles of the brain contributes to ventricular cyst formation.
Pathology contributes to the appearance of clinical symptoms:
- Dizziness, headache;
- Movement coordination disorder;
- Muscle cramps, epilepsy;
- Hypertonicity in newborns.
Localization of manifestations near important nerve centers contributes to the emergence of specific symptoms.
The presence of cytomegalovirus or herpetic infection complicates the course of the disease. Detection of a pathogen and CSS in an adult with a high degree of probability indicates a viral etiology of cystic cavities.
Microcyst of the choroid plexus of the right lateral ventricle rarely causes neurological disorders.
In children, vascular microcysts and larger formations are not accompanied by pathological symptoms. The International Classification of Diseases (ICD 10) does not classify nosology as a number of pathological conditions.
Brain cyst, true form, causes and prognosis
The prognosis of cystic formations in a child depends on the cause, location and size of the cyst, therefore such children undergo PCR diagnostics to determine the virus, and if it is present, the necessary treatment and further observation, which includes mandatory ultrasound examination of the brain (neurosonography) at 3 months, six months and a year of the baby’s life. In most cases, a choroid plexus cyst detected in a newborn, even in the presence of a virus, has a favorable prognosis , disappears by the age of one year and does not resume its development in the future.
A ramolitic cyst can also end its existence in infancy, or it can behave like a formation that arises for other reasons and is called a vascular cyst with a stretch, since its genesis is a violation of the vascular wall, but it itself is localized in the brain tissue (after the fact) .
Thus, the reasons for the formation of a pathological brain cyst may be as follows:
- Infections;
- Birth and other injuries;
- Microstroke;
- Hemorrhagic stroke (a cyst occurs at the site of a hematoma formed as a result of vascular damage);
- Ischemic stroke (tissue necrosis will give rise to a remolition cyst of vascular origin)
- Aneurysm.
It should be noted that if we are talking about damage to the vascular wall, then in this case we mean the arterial wall, since veins, as a rule, do not participate in such processes.
Consequences of choroid plexus cysts
Complicated cystic formations cause specific manifestations:
- Hypertonicity of newborns;
- Neurological symptoms due to compression of brain structures;
- Epilepsy (muscle cramps);
- Slight loss of vision and hearing.
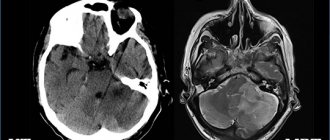
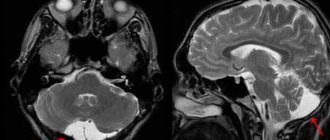
Magnetic resonance imaging will need to distinguish a true vascular cyst from a pseudocyst. The latter type is a variant of the physiological development of the brain, but the anatomical structure when examined by ultrasound resembles a cavity. Magnetic resonance imaging is an accurate study (informativeness is about 96%). The three-dimensional modeling mode will allow you to correctly verify the nosology.
Edwards syndrome can be detected by ultrasound by identifying abnormalities of the limbs and changes in internal organs. Additional diagnostic tests:
- Determination of the concentration of human chorionic gonadotropin;
- Blood chemistry;
- Analysis of amniotic fluid.
A special risk group is women aged 32 years and older with hormonal disorders.