Find out more about nervous diseases starting with the letter “N”: Sleep disturbance; Narcolepsy; Hereditary cerebellar ataxia of Pierre-Marie; Spinal circulatory disorders; Trigeminal neuralgia; Neuralgia of the submandibular and sublingual nodes; Neuralgia of the glossopharyngeal node; Neuralgia of the ear ganglion; Neurasthenia; Neural amyotrophy of Charcot-Marie-Tooth; Acoustic neuroma; Neuroma; Optic neuritis; Pharyngeal neuritis; Neuritis of the facial nerve; Neuritis; Obsessive-compulsive neurosis; Pharyngeal neurosis; Neuroses; Neurosis-like stuttering; Femoral nerve neuropathy.
What is glossopharyngeal neuralgia?
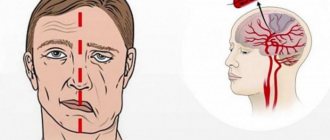
If the cranial nerve is affected by a quarter on one side, and paroxysms of pain appear in the tonsils, soft palate, pharynx and ear, then the patient may have neuralgia of the glossopharyngeal nerve. With this pathology, a violation of the taste perception of the posterior third of the tongue, on the affected side, is detected. Hypersalivation and decreased reflex of the palate and pharynx are also noted. To make a diagnosis, an examination by a neurologist or dentist is required. CT and MRI of the brain are indicated as hardware diagnostic methods. In most cases, treatment is conservative, including:
- Anticonvulsants;
- Analgesics;
- Sleeping pills and sedatives;
- Vitamin therapy;
- Physiotherapy;
- General strengthening procedures.
4.Treatment
Treatment for glossopharyngeal neuralgia is aimed primarily at relieving pain. Given its severity and specificity, in some cases it is necessary to prescribe both non-narcotic and narcotic analgesics; Antiparoxysmal and anti-inflammatory drugs, vitamin complexes, restorative therapy, and electrophysiotherapeutic methods are also used. In situations where the established cause of neuralgia is mechanical compression (compression) of the nerve, for example, with hyperplasia of structures adjacent to the nerve, neurosurgical intervention is performed.
Conservative treatment usually lasts quite a long time (up to several years), but in most cases it leads to the elimination or significant reduction of neuralgia.
Structure of the glossopharyngeal nerve
N. glossopharyngeus or glossopharyngeus nerve begins in the nuclei of the medulla oblongata. It is based on motor, sensory and autonomic parasympathetic fibers. Moreover, the sensory fibers begin in the sensory nucleus common to the vagus and glossopharyngeal nerves. They innervate the mucous membrane of the pharynx, soft palate, tongue, tonsils, and Eustachian tube. The sensation of taste in the anterior two-thirds of the tongue is provided by taste fibers emerging from the nucleus of the tractus solitarius. The taste fibers of the glossopharyngeal nerve are responsible for the taste sensations of the posterior third of the tongue and epiglottis.
The motor fibers originate in the nucleus ambiguus and innervate the stylopharyngeal muscle, which is necessary for raising the pharynx. Together with the vagus nerve, they form the reflex arcs of the pharyngeal and palatal reflexes.
Parasympathetic fibers originate in the salivary nucleus. Being part of the tympanic and lesser petrosal nuclei, they reach the autonomic ganglion, and with the branch of the trigeminal nerve they regulate salivation of the parotid gland.
Since the pathways and nuclei of the glossopharyngeal and vagus nerves are common, isolated pathology n. Glossopharyngeus. But more often symptoms of combined lesions are observed.
Pathogenesis
There are cases of idiopathic Sicard syndrome. At the same time, it is almost impossible to establish the etiology of the disease. Provoking factors may be:
- Acute or chronic intoxication;
- Otitis;
- Pharyngitis;
- Tonsillitis;
- Sinusitis;
- Atherosclerosis;
- Viral infections incl. flu.
Secondary neuralgia occurs due to:
- Arachnoiditis, encephalitis and other infectious lesions of the posterior cranial fossa.
- TBI.
- Hyperthyroidism.
- Diabetes mellitus.
- Meningiomas, gliomas, medulloblastomas and other intracerebral tumors of the cerebellopontine ganglion.
- Compression and irritation of any part of the glossopharyngeal nerve.
- Nasopharyngeal tumors.
- Intracerebral hematomas;
- Carotid artery aneurysm;
- Hypertrophy of the styloid process.
- Overgrowth of osteophytes of the jugular foramen.
- Ossification of the styloid ligament.
In some cases, pathology may be the first symptom of cancer of the larynx or pharynx.
Symptomatic picture
Clinical signs include painful paroxysms lasting from a few seconds to three minutes. A sharp acute pain originates at the root of the tongue and instantly spreads to the tonsils, soft palate, ear and pharynx. May radiate to the eye, neck and lower jaw. Pain can be triggered by coughing, chewing food, its temperature, yawning, swallowing and even talking. During paroxysm, dry mouth is noted, immediately after hypersalivation. But dryness is not a mandatory sign of diagnosis, because the secretory insufficiency of the parotid gland can be compensated by the remaining salivary glands.
Paresis of the levator pharyngeal muscle does not cause swallowing disorders. But difficulties in chewing and swallowing associated with impaired proprioceptive sensitivity, which is responsible for the position of the tongue, may be noted by patients.
The disease has a wave-like course, worsening in autumn and winter.
Neuralgia treatment and prevention
Very often, for neuralgia, physiotherapeutic treatment is prescribed - magnetic therapy, UHF, electrophoresis, massage, etc. Manual therapy is also used to treat neuralgia, as well as acupuncture, physical therapy, and B vitamins. In extreme cases, treatment of neuralgia can be surgical.
With timely treatment, neuralgia can be corrected. With symptomatic neuralgia, treatment of the underlying disease is imperative.
The importance of seeing a doctor for diagnosis and treatment of neuralgia is due not only to the fact that serious diseases that cause neuralgia may be hidden behind it, but also to the fact that based on symptoms, other diseases can be mistaken for neuralgia - acute cholecystitis or pancreatitis, myocardial infarction, etc. .
Different types of neuralgia require different approaches to treatment, so the treatment prescribed by a specialist depends on the location of the neuralgia and its origin. Treatment is prescribed based on the diagnosis, which is made based on the results of studies - MRI, ECG, radiography, etc.
Preventive measures to avoid neuralgia include regular medical examinations, avoidance of hypothermia, drafts, sudden movements, a healthy lifestyle, and treatment of chronic diseases. Taking B vitamins reduces the risk of developing neuralgia.
Diagnostic methods
The diagnosis is made by a neurologist, who, if necessary, can involve an otolaryngologist and dentist. During the examination, the doctor determines analgesia, that is, the absence of pain sensitivity at the base of the tongue, upper parts of the pharynx, and tonsils. Taste sensitivity is also studied, for which a taste solution is applied to symmetrical areas of the tongue. The diagnosis is confirmed by isolated unilateral taste disorder in the posterior third of the tongue. Bilateral disruption is typical for diseases of the oral mucosa, such as chronic stomatitis.
The pharyngeal reflex needs to be checked. To do this, touch the back wall of the throat with a paper tube, which provokes a swallowing movement and occasionally a cough. Normally, touching the soft palate should be accompanied by a lifting of the palate and uvula. Sicard syndrome is characterized by the absence of reflexes on one side. But a similar symptomatic picture can occur with damage to the vagus nerve. If the pharynx and pharynx are strewn with herpetic rashes, the doctor can diagnose ganglionitis of the ganglionitis of the glossopharyngeal nerve nodes, which differs in almost identical n. Glossopharyngeus clinical picture.
To establish the root cause of symptomatic neuritis, neuroimaging diagnostics is needed:
- MRI or CT scan of the brain;
- Electroencephalogram;
- Echo-EG;
- Ophthalmoscopy with consultation with an ophthalmologist.
It is necessary to distinguish between neuralgia of the glossopharyngeal nerve and diseases that cause painful paroxysms of the face and head. These include:
- Neuralgia of the ear ganglion;
- Trigeminal neuralgia;
- Oppenheimer's syndrome;
- Glossalgia;
- Ganglionitis of the pterygopalatine ganglion;
- Retropharyngeal abscess;
- Tumors of the pharynx.
Chronic catarrhal laryngitis
Characterized by superficial inflammation of the laryngeal mucosa. We can talk about chronicity of catarrhal laryngitis when the symptoms of the disease last more than six months. Most often it occurs as a consequence of other diseases that have become chronic, such as: rhinitis, sinusitis, tonsillitis, periodontitis, periodontitis, bronchitis - that is, diseases in which there is a focus of chronic infection. Often one of the main causes of catarrhal laryngitis is extraesophageal reflux (reflux of contents from the stomach into the esophagus, and then from the esophagus into the hypopharynx and larynx). Extrafood reflux occurs in people with gastroesophageal reflux disease (GERD) and most often occurs during sleep, so the patient may not be aware of the problem. Also, factors contributing to the development of the disease include: smoking, specifics of the profession (increased vocal load, dust, gas pollution, frequent hypothermia). Thus, chronic catarrhal laryngitis occurs due to a combination of reasons: chronic infection, both bacterial and mixed, various types of irritants, insufficient immune response.
Symptoms: change in voice (hoarseness or hoarseness, voice fatigue), soreness or discomfort in the throat.
On examination, redness and unevenness of the laryngeal mucosa are visible, the vocal folds are often pink in color, thickened, with a pronounced vascular pattern; during phonation, the vocal folds do not close tightly. Enlarged lymphoid granules of the larynx and hypopharynx are often detected.
Treatment: identification and elimination of the cause of inflammation of the mucous membrane of the larynx and hypopharynx, identification of foci of infection of the ENT organs, oral cavity, tracheobronchial tree, GERD. A culture and PCR test from the pharyngeal mucosa is prescribed to identify pathogens. Drug treatment is most often local antibacterial and anti-inflammatory therapy, treatment of the source of infection and GERD (if present).
Therapy
To treat neuralgia of the glossopharyngeal nerve, conservative therapy is prescribed. The only exception is if the underlying cause is tumors and hypertrophy of the styloid process, leading to compression of the nerve. In these cases, surgery is indicated.
To relieve pain, a 10% solution of cocaine is prescribed, which is applied to the root of the tongue and pharynx. This allows you to eliminate paroxysms for 6-7 hours. If this remedy turns out to be ineffective, a 1-2% novocaine solution is injected into the root of the tongue. Non-narcotic analgesics and anticonvulsants are also prescribed internally. If the pain syndrome is pronounced, it is advisable to prescribe sedatives, hypnotics, antipsychotic medications and antidepressants. AFT, multivitamin complexes and FiBS are used as general strengthening agents.
Among the physiotherapeutic procedures that have proven effectiveness are:
- SMT on the area of the larynx and tonsils;
- Diadynamic therapy;
- Galvanization.
1.General information
One of the paired cranial nerves is called the glossopharyngeal. This (IX) pair received its name in connection with the functions that it controls: the activity of the stylopharyngeal muscle, the sensitivity of the taste pimples of the basal part of the tongue, the secretory activity of the parotid gland, as well as the tactile sensitivity of a number of structures of the hearing organs and the oral cavity.
The term "neuralgia" is translated as "nerve pain" or "nerve pain." Neurogenic pain syndromes are distinguished by their specific nature (the pain is usually piercing, the sensations are similar to an electric shock extended over time), significant severity and persistence: it is impossible to find a forced position, conventional analgesics have little effect, etc.
A similar syndrome, caused by an isolated lesion of the glossopharyngeal nerve, is very rare in clinical practice - its statistical frequency is one case in approximately 620,000 people. Among the patients, men predominate, and in the age group - people over 40 years old.
A must read! Help with treatment and hospitalization!