Depending on the cause, the headache can be localized in a specific area or cover the entire head. The nature of the sensations may also vary, as well as their frequency. One of the most debilitating is considered to be a headache in the crown of the head. The crown is a part of the surface of the head located between the back of the head and the forehead, i.e. on top.
It is worth noting that no one is immune from headaches in the crown area. It can even appear in a child. If the crown of your head hurts, the nature of the pain may be different. There may be a feeling of squeezing, bursting from the inside, sometimes even tingling. Often, pain symptoms can be pulsating in nature or radiate to the ears or optic nerve.
At CELT you can get advice from a specialist algologist.
- Initial consultation – 4,000
- Initial consultation with the head of the Pain Clinic - 4,500
Make an appointment
The reasons why the parietal part of the head hurts can be very different. The most common is considered to be increased intracranial pressure, but it is not the only one.
Causes of pain in the parietal part of the head
As already mentioned, the causes of headaches in the crown area can be different, but some of them are more common and have similar symptoms.
Pain in the crown due to tension
If the crown of the head hurts, the reason may lie in tension, which arises due to prolonged stay in an uncomfortable position, without the necessary movement and insufficient lighting. Occupational pain in the crown of the head occurs due to the fact that the workplace does not meet ergonomic standards.
The pain is dull, pressing, squeezing in nature. They make you feel as if you are wearing a tight helmet on your head.
Pain in the crown due to neuroses
More than 50% of complaints of pain in the parietal region belong to patients with neuroses. They can be either constant or periodic, vary in intensity and are accompanied by:
- panic attacks;
- experiences;
- emotional instability.
If pain symptoms are accompanied by dizziness and numbness of the arms and legs, you should urgently seek medical help.
Pain in the crown after injury
Even minor traumatic brain injuries can cause pain in the crown of the head. It may be due to the following:
- disturbance of the movement of cerebrospinal fluid;
- pinched nerve roots;
- damage to the membranes of the brain.
The “companions” of pain symptoms in this case are:
- decreased performance;
- memory impairment;
- difficulty concentrating
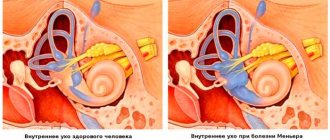
Pain in the crown due to vascular diseases
Diseases such as hyper- and hypotension, vegetative-vascular dystonia are also factors leading to the appearance of pain in the crown. Due to increased or decreased vascular tone, they are not able to provide the necessary blood pressure, which leads to spasms or compression of nerve cells.
More about vegetative-vascular dystonia
Why does my scalp hurt?
What exactly can the pain be associated with?
The simplest thing is hairstyles with pins, a tight ponytail, an unnatural parting that does not match the hair growth. Compressive headdresses too. This condition leads to impaired blood circulation in the scalp. It's just numbness, like what happens when you sit on your leg. This can lead to injury to the nerve endings of the hair follicles.
Therefore, you should not do such hairstyles often and for a long time; you need to periodically relax the tail, change the parting, and do a massage to restore blood supply to the hair follicles. The habit of tightly braiding your hair can lead to poor appearance and hair loss.
Occipital or trigeminal neuropathy or other neurological conditions. There may be symptoms such as:
- burning, shooting, throbbing pain in the neck and head
- pain on one side only
- elevated body temperature
These symptoms may indicate a neurological pathology; consultation with a neurologist is necessary.
Diseases of the scalp and hair. Pain is accompanied by symptoms such as:
- skin itches, itches;
- dandruff;
- hair loss (diffuse telogen effluvium);
- localized most often on the top of the head (parietal zone).
It could also be an allergic reaction to shampoo or other cosmetics, or skin damage due to coloring/bleaching.
Read more about the causes and treatment of itching >>>
A trichologist explains these symptoms in the video:
The best way out in this case is to consult a dermatologist or trichologist. Only an examination by a specialist using a trichoscope under good magnification will help establish an accurate diagnosis or exclude such serious conditions as:
- irreversible forms of hair loss of an autoimmune nature;
- lupus erythematosus;
- diffuse alopecia;
- androgenetic alopecia;
- alopecia areata;
- seborrheic dermatitis;
- psoriasis;
- eczema;
- bacterial or fungal infections (folliculitis, herpes zoster, furunculosis);
- herpes;
- common trichodynia (the exact cause is not clear).
With skin diseases, there will be obvious symptoms such as rashes, plaques, swelling, weeping, peeling, and swelling. Only a dermatologist can help here.
If there are no skin symptoms or other obvious causes, but there is pain, especially in combination with hair loss, an examination by a trichologist is necessary.
Which doctor can you contact for hair loss >>>
Why is it important to see a specialist? Taking time, self-medicating, without knowing the causes of scalp pain and hair loss, without establishing an accurate diagnosis, is fraught with aggravation of the problem. If time is lost, it will be more difficult or even impossible to restore the hair to its previous condition. Self-medication and procedures (hair growth stimulants, mesotherapy) can aggravate the situation.
Diagnostics
You should not postpone a visit to a specialist if, along with severe pain in the crown area, the following clinical manifestations are observed:
- increased pain;
- visual impairment;
- deterioration in general health;
- memory disorder;
- increase in general temperature;
- nausea, vomiting.
You can contact the CELT clinic, and our specialists will help you get rid of not only pain, but also the reasons that caused it.
In order to determine the cause of pain, our specialists carry out:
- magnetic resonance imaging (MRI);
- computed tomography ();
- blood test for infections;
- blood pressure monitoring.
If necessary, an examination by an ophthalmologist or surgeon may be scheduled.
What to do if your hair roots hurt?
- The most accessible remedy for scalp pain is a regular massage, which you can do yourself. This method of exposure can be used if pain is caused by fatigue or external factors
- The massage is carried out with light circular movements with your fingertips for 5-10 minutes in the morning and evening.
- 1-2 times a week you can additionally use natural oil - almond, burdock, olive, castor, combining the beneficial effects of massage with the nutritional properties of natural oils
- If the cause of pain lies in the use of inappropriate cosmetics, you should replace cleansers and care products, giving preference to products from organic cosmetics series. Another solution would be to prepare shampoos, conditioners and healthy masks at home.
Head massage for pain at the hair roots
Treatment
Analgesics are one of the effective means of combating headaches. However, we should not forget that they do not eliminate the main cause that caused such a reaction, but only eliminate the clinical manifestations, and after some time the pain will remind itself again.
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions
If your forehead hurts. We're talking about frontal sinusitis
Viruses, hypothermia, tobacco smoke, summer swimming and diving in ponds, seas and rivers... These factors can contribute to the development of acute and exacerbation of chronic rhinosinusitis, in particular sinusitis. What it is? How does it manifest itself? How is it detected and treated? Is it possible to cure sinusitis without antibiotics?
These and other questions are answered by Lyudmila Vladimirovna Vandysheva, Candidate of Medical Sciences, Associate Professor of the Department of Surgery at the Medical Institute of Tula State University, and otolaryngologist at the Expert Clinic Tula.
— Lyudmila Vladimirovna, tell us what kind of disease this is - frontal sinusitis? How common is it?
— Frontitis is an inflammation of the mucous membrane of the frontal (frontal) sinuses. In total, humans have eight paranasal (paranasal) sinuses (four on each side). All of them have anastomoses with the nasal cavity, through which the sinuses are ventilated and mucus is removed into the nasal cavity and pharynx. There are mainly two frontal sinuses. They are located in the frontal bone, behind the brow ridges.
How common is frontal sinusitis? Acute frontal sinusitis is an uncommon disease. In my practice, there are approximately 5–10 cases of sinusitis per 100 cases of inflammation of the paranasal sinuses. But in terms of the frequency of intracranial complications, frontal sinusitis ranks second (after inflammation of the ethmoid sinuses).
Frontitis occurs in both adults and children.
— When talking about sinuses, you can often hear the word “sinusitis.” Please tell me what it is and what is the difference between sinusitis and frontal sinusitis?
— It is more correct to say “rhinosinusitis,” since it has been proven that inflammation of the mucous membrane of the nasal cavity (rhinosinus) and inflammation of the paranasal sinuses (sinusitis) are inseparable from each other. But this is a general concept.
Depending on the location of the inflammatory process, the following are distinguished:
- sinusitis (inflammation of the maxillary sinuses);
- ethmoiditis (inflammation of the ethmoid sinuses);
- sphenoiditis (inflammation of the sphenoid sinuses);
- frontal sinusitis (inflammation of the frontal sinuses).
That is, frontal sinusitis is a special case of rhinosinusitis.
— At what age can a child develop frontal sinusitis?
— The literature indicates that by the age of 12–14 years the frontal sinuses are fully formed. But in practice, we see that even in the sinuses, which have not yet fully formed, there can be an inflammatory process. That is, the development of frontal sinusitis is possible in children aged 7, 8, 9, 10, 12 years, etc.
— What are the reasons for the development of frontal sinusitis?
— The main cause of inflammation is viral and bacterial infection. It has been proven that 98% of people with ARVI have swelling in the paranasal sinuses. By the time of recovery, this swelling goes away safely. But nevertheless, in 2% of patients this edema persists and leads to the development of rhinosinusitis. Therefore, if the patient’s complaints persist or intensify for more than 10 days after the onset of acute respiratory viral infection, he should be immediately examined for rhinosinusitis. These complaints include:
- difficulty breathing through the nose;
- nasal discharge or mucus running down the back of the throat;
- pain in the projection of the sinuses;
- loss of smell;
- cough in children.
Viral infection, hypothermia, toxic effects, tobacco smoking, etc. can provoke a decrease in the immunological activity of the mucous membrane, i.e. protection. And then its own bacterial infection activates, which constantly lives in our nasopharynx (the nasopharynx is a non-sterile place), and the inflammatory process begins.
Unfortunately, after insufficient treatment, as well as self-medication, swelling of the mucous membrane remains in the paranasal sinuses, the volume of the air cavity of the sinuses decreases, and infection can enter the sinuses through the natural anastomosis, water when swimming, especially diving in various bodies of water, which, naturally, are not sterile. This “recovery” often ends in the doctor’s office.
In addition, in adults, a provoking factor can be riding a motorcycle or bicycle in the cold season, when the wind hits the face and the frontal area is not protected.
— How does frontal sinusitis manifest itself?
— Earlier I listed the symptoms of rhinosinusitis. This is difficulty in nasal breathing, nasal discharge or mucus running down the back of the throat, pain in the projection of the sinuses, loss of smell, cough in children. Frontal sinusitis also manifests itself. Only pain in the projection of the frontal sinuses (in addition to the above complaints) is a clarifying factor of frontal sinusitis. But often frontal sinusitis is diagnosed only after additional examination methods and is a “find”, since the patient can only complain of nasal congestion, nasal discharge, loss or decreased sense of smell (especially if the inflammatory process is non-purulent, i.e. in the edema phase).
— Lyudmila Vladimirovna, what diagnostic methods are used to diagnose “frontal sinusitis”?
— The first is an examination of the nasal cavity, or rhinoscopy. When examined in the middle nasal passage, you can see a strip of pus or infected mucus, swelling of the mucous membrane. Next, it is recommended to take an x-ray of the paranasal sinuses. But today, according to various sources, the percentage of reliability of x-ray examination ranges from 37 to 45%. Therefore, the gold standard is magnetic resonance or computed tomography of the paranasal sinuses. Better, of course, is an MRI. Here you can see everything: swelling or the level of fluid in the frontal sinus, and even what kind of fluid it is (mucus or pus).
Often, acute or chronic frontal sinusitis occurs hidden, masked by other symptoms: headache, migraine, cough, weakness, etc.
Case from practice
MRI images of the frontal sinus of an 8-year-old child with obsessive coughing for 2 years, who was treated by a neuropsychiatrist for obsessive-compulsive disorder syndrome
MRI of the frontal sinuses (before and after treatment)
In addition, in order to correctly diagnose and prescribe quality treatment, swabs are taken from the throat and nose for microflora, and its sensitivity to antibiotics is determined. And to find out the intensity of inflammation, a blood test is performed.
You can sign up for an MRI of the paranasal sinuses here. ATTENTION: the service is not available in all cities
— How is frontal sinusitis treated?
— Treatment of frontal sinusitis can be conservative or surgical. The patient is either sent to a hospital or treated in a clinic office. If there is a level of pus in the sinus, it is necessary to puncture the frontal sinus. This is a traumatic procedure. It is carried out through the anterior wall of the frontal sinus, i.e. practically through the frontal bone. The anterior wall of the sinus is punctured and the pus is removed by rinsing the sinus through the puncture hole.
How is conservative therapy carried out? To remove the contents of the frontal sinus, it is necessary to create conditions for its drainage through a natural anastomosis that opens into the nasal cavity. In our clinic, frontal sinusitis is treated using the moving method. To do this, we insert a turunda (a small narrow gauze swab) with a vasoconstrictor into the nose. This relieves swelling of the mucous membrane and opens the passage into the frontal sinus. If necessary, we perform local anesthesia and begin to rinse the paranasal sinuses using the fluid displacement method.
There are several modifications of this method. In my practice, I rinse the sinuses with the patient sitting, with his head tilted back. A saline or antiseptic solution is slowly injected into one half of the nose using a syringe without a needle; mucus and pus along with the solution are evacuated from the other half of the nose using an electric suction. In this case, the patient either closes or opens his mouth, thereby changing the pressure in the nasopharynx.
Broad-spectrum antibiotics, a herbal preparation, and a mucolytic (expectorant) agent are required to help remove mucus better. And do not forget to give the patient a drug to normalize the intestinal microflora along with the antibiotic.
When we have completely cleared the sinuses, we prescribe decongestant therapy, magnetic therapy, and rehabilitation measures.
And I would like to dwell a little on frontal sinuses in pregnant women. The method of rinsing the nose by moving the liquid while the patient is sitting helps a lot here. With its help, the nose and paranasal sinuses are washed very well.
— Is it possible to cure frontal sinusitis without antibiotics?
— In my practice there were such cases. This is possible if frontal sinusitis is not advanced, if there is mucus in the frontal sinus and not pus. The displacement method is quite acceptable and sufficient for the treatment of non-purulent frontal sinusitis.
Read materials on the topic:
How to use antibiotics correctly? Instructions for use Why don't antibiotics help?
— Tell me, is it possible to treat frontal sinusitis at home, and if so, how?
- I don't recommend doing this. From the story of one patient: “I stuck a piece of chestnut in my nose and pus came out. I have recovered." This patient will come to us anyway, sooner or later. There is no fear of chestnut infection. Perhaps the immune system has somehow dealt with the small amount of pus, but the bacterial infection is still alive. And the strength of this infection depends on its quantity. As soon as provoking factors appear - ARVI, getting your feet wet, riding a motorcycle, diving (water under pressure entered the nose and sinuses) - what I said at the beginning of our conversation, the infection immediately activates. And then a chronic inflammatory process will begin. Therefore, such diseases are not treated at home either in children or adults.
— Is it possible to warm the forehead during frontal sinusitis?
- Of course you can’t. The strength of the infection, I repeat, depends on its quantity, and the number of bacteria is growing, there is active reproduction on the warm, moist mucous membrane of the paranasal sinus. At a certain stage of treatment, magnetic therapy, laser therapy can be used on the frontal area, on the area of the paranasal sinuses. But as for warming your forehead with salt, buckwheat, sand - this should not be done under any circumstances.
— What complications can there be if frontal sinusitis is not treated?
- Firstly, next to the frontal sinus there is an orbit. And the pus can destroy its wall and exit into the cavity of the orbit. That is, even complete loss of vision is possible.
Secondly, rhinogenic meningitis may develop. That is, meningitis, which is a consequence of purulent or even non-purulent inflammation of the sinuses. First, the forehead hurts, then nausea and vomiting begin, not associated with food intake, stiffness of the neck muscles occurs, that is, they become hard, the patient cannot touch the sternum with his chin. There may be headache and dizziness. If the diagnosis of meningitis is confirmed, then surgery is performed.
With complications of frontal sinusitis, there can be no talk of any conservative methods of therapy.
Read more about meningitis in our articles:
Attack to the head. How to protect yourself from summer meningitis? Will an MRI show meningitis?
— Is frontal sinusitis contagious to others?
- Yes, frontal sinusitis is contagious. This is a severe bacterial infection. Often the whole family comes with rhinosinusitis: dad has sinusitis, little one has ethmoiditis, mom has sinusitis. Therefore, the patient needs not only separate dishes, but also a separate towel, a separate pillow, etc. Close contact between a sick mother, father, grandmother, etc. and a child is prohibited (you cannot kiss the child). A spoon and pacifier are only the baby’s personal property; it is important to always remember this.
Interviewed by Marina Volovik
The editors recommend:
What will an MRI of the sinuses show? Not breathing! How to treat a runny nose in children? Deviated nasal septum: leave it or fix it?
For reference:
Vandysheva Lyudmila Vladimirovna
In 1982 she graduated from the pediatric faculty of the Voronezh Medical Institute. 1989 – specialization in otolaryngology. 2007 – 2009 – Postgraduate studies at the Medical Institute of Tula State University. Currently, he is a doctor of the highest category, Candidate of Medical Sciences, Associate Professor of the Department of Surgery at the Medical Institute of Tula State University, and an otolaryngologist at the Expert Clinic in Tula. Receives at the address: st. Boldina, 74.