The first signs of Parkinson's disease, modern methods of treatment
Parkinson's disease is a chronic degenerative disease of the nervous system in which a person loses the ability to control their movements. The disease develops relatively slowly, but has a tendency to progress. It is a fairly common problem - 4% of the elderly population suffer from manifestations of parkinsonism.
The development of the disease is based on changes that occur in the substantia nigra of the brain. The cells in this area are responsible for producing the chemical dopamine. It mediates signal transmission between neurons in the substantia nigra and striatum in the brain. Violation of this mechanism leads to the fact that a person loses the ability to coordinate his movements.
Epidemiology
Parkinson's disease accounts for 70-80% of cases of parkinsonism syndrome. It is the most common neurodegenerative disease after Alzheimer's disease.
The disease occurs everywhere. Its frequency ranges from 60 to 140 people per 100 thousand population, the number of patients increases significantly among representatives of the older age group. The proportion of people with Parkinson's disease in the age group over 60 years old is 1%, and over 85 years old - from 2.6% to 4%. Most often, the first symptoms of the disease appear at 55-60 years of age. However, in some cases, the disease can develop before the age of 40 (early-onset Parkinson's disease) or before 20 years of age (juvenile form of the disease).
Men get sick slightly more often than women. There were no significant racial differences in the incidence pattern.
Causes
There are two types of Parkinson's disease. The first is true parkinsonism, it accounts for up to 80% of cases of the disease.
The second is parkinsonism syndrome, which accompanies traumatic brain injuries, encephalitis, stroke, and brain tumors.
The exact causes of true parkinsonism, or Parkinson's disease, are unknown.
But several facts have been established:
the disease develops mainly in old age (after 60 years),
degenerative changes begin with the irreversible process of death of neurons in the brain stem,
the development of symptoms of the disease is associated with a lack of dopamine, a neurotransmitter on which signal transmission in interneuron connections depends,
there is a genetic predisposition.
In approximately 15% of cases, Parkinson's disease occurs against the background of a negative family history (presence of the disease in close relatives) and is inherited.
Some factors may influence the development of the disease:
- intoxication (chronic poisoning with chemical toxins in hazardous industries, unfavorable environment, exposure to pesticides, manganese),
- infectious lesions of the central nervous system (encephalitis, etc.),
- traumatic brain injuries,
- impaired functioning of the kidneys and liver.
Parkinson's disease - causes
The exact causes of Parkinson's disease remain a mystery to this day, however, some factors, coming to the fore, still take on the leading function, and therefore are considered to be the culprits of this pathology.
These include:
- Aging of the body, when the number of neurons naturally decreases, and, therefore, the production of dopamine decreases;
- Some medications used to treat various diseases and, as a side effect, have an effect on the extrapyramidal structures of the brain (aminazine, rauwolfia preparations);
- Environmental factors: permanent residence in rural areas (treatment of plants with substances intended to destroy agricultural pests), near railways, highways (transportation of environmentally hazardous goods) and industrial enterprises (harmful production);
- Hereditary predisposition (the gene for the disease has not been identified, but the family pattern is indicated - 15% of patients have relatives suffering from parkinsonism);
- Acute and chronic neuroinfections (for example, tick-borne encephalitis);
- Vascular cerebral pathology;
- Poisoning with carbon monoxide and heavy metal salts;
- Brain tumors and injuries.
At the same time, when considering the causes of Parkinson’s disease, it is worth noting an interesting fact that pleases smokers and coffee lovers. For those who smoke, the “chance” of getting sick is reduced by 3 times. It is said that tobacco smoke has such a “beneficial” effect because it contains substances resembling MAOIs (monoamine oxidase inhibitors), and nicotine stimulates the production of dopamine. As for caffeine, its positive effect lies in its ability to increase the production of dopamine and other neurotransmitters.
Forms and stages of the disease
There are several forms of the disease:
| Trembling-rigid | in this situation, trembling is a typical sign. A similar pathology is diagnosed in 37% of cases. |
| Rigid trembling | the main signs are general slowness of movements and increased muscle tone. This symptomatology is observed in approximately 21% of cases. |
| Trembling | At the beginning of development, the main symptom is trembling. At the same time, muscle tone does not increase, and slowness of movements or poor facial expressions appear slightly. This type of pathology is diagnosed in 7% of cases. |
| Akinetic-rigid | trembling may be completely absent or appear slightly - for example, during periods of excitement. This type of disease is detected in 33% of cases. |
| Akinetic | characterized by the absence of voluntary movements. This type of pathology occurs in only 2% of cases. |
The generally accepted gradation of stages of the disease, reflecting the degree of severity, is as follows:
- stage 0 – absence of motor disorders;
- stage 1 – unilateral nature of the manifestations of the disease;
- stage 2 – bilateral manifestations of the disease, the ability to maintain balance is not affected;
- stage 3 – moderately severe postural instability, the patient is able to move independently;
- stage 4 – severe loss of motor activity, the ability to move is preserved;
- stage 5 - the patient is bedridden or wheelchair-bound, and movement without assistance is impossible.
The modified Hoehn and Yarh scale (Hoehn and Yarh, 1967) suggests the following division into stages:
- stage 0.0 – no signs of parkinsonism;
- stage 1.0 – unilateral manifestations;
- stage 1.5 – unilateral manifestations involving the axial muscles (neck muscles and muscles located along the spine);
- stage 2.0 – bilateral manifestations without signs of imbalance;
- stage 2.5 – mild bilateral manifestations, the patient is able to overcome the caused retropulsion (the patient accelerates backward when pushed from the front);
- stage 3.0 – moderate or moderate bilateral manifestations, slight postural instability, the patient does not need outside assistance;
- stage 4.0 – severe immobility, the patient’s ability to walk or stand without support is preserved;
- stage 5.0 – the patient is confined to a chair or bed without assistance.
Stages
Five stages of the disease have been identified, as well as one intermediate stage, which is called one and a half. Therapy is most effective in the first and one-and-a-half stages.
- Stage 1.
A minor motor disorder is observed only in one hand. Non-specific symptoms also occur, such as sleep disturbances, impaired sense of smell, mood swings and persistent fatigue for which there is no reason. Later, when the patient is nervous, the fingers of the affected hand begin to tremble. By the end of the period, the shaking becomes constant.Intermediate stage.
Symptoms are also localized to only one limb or some other part of the body. Trembling is almost constant, disappearing only during sleep. Fine motor skills are very difficult, the kidneys are damaged. Sometimes the patient notes that there is slight stiffness in the upper back and neck. Swing movements of the affected arm are limited. Gait is noticeably impaired.
- Stage 2.
Difficulty in movement affects both sides of the body. Tremor of the tongue and lower jaw is quite common, and drooling is possible. Facial expressions worsen, speech slows down. All movements in the joints are difficult. The condition of the skin changes as the functioning of the sweat glands is disrupted. Because of this, it becomes too dry or, conversely, excessively oily. The patient can still restrain some involuntary movements. The patient copes with simple actions, but very slowly and with great effort. - Stage 3.
The patient's condition worsens. The gait becomes doll-like - small steps with parallel feet. The face takes on the appearance of a mask. The trembling spreads to the head and manifests itself in the form of nodding movements like “yes” or “no”. The supplicant pose characteristic of the disease is formed. Her back is slouched, her head is bent down, her arms extended forward are bent at the elbows and pressed to her body, her legs are bent. All joint movements become sharp, like a gear mechanism. Speech impairments continue to progress. The patient often repeats the same words and does not always understand their connection with each other. A person can still take care of himself, but with great difficulty. Getting into the sleeves or fastening the buttons in one go is not always possible. He already needs help getting dressed. Hygiene procedures take much more time than before. - Stage 4.
The patient has great difficulty maintaining his balance and, getting out of bed, easily falls forward. If he, standing or moving, is slightly pushed, he immediately continues to move by inertia in a given direction until he encounters an obstacle. Frequent falls lead to injuries and fractures. It becomes difficult to change body position for a while. Speech changes - it is blurred, quiet and nasal. The patient often experiences depression with suicide attempts. By the end of this period, dementia will most likely develop. A person cannot cope with self-care without outside help. - Stage 5.
Progression of the disease leads to further deterioration of motor functions. The patient cannot stand up, walk or sit independently. It becomes impossible to eat food not only due to the development of tremors and constrained movements, but also due to changes in swallowing function. There is no control of urine and feces. It is almost impossible to understand speech, or it is completely absent. The mood is almost always depressed. The patient cannot cope with any, even the simplest tasks, without outsiders and is completely dependent on those who care for him.
Due to the slow progression of the disease, in people who are diagnosed with Parkinson's disease in old age, death often occurs before stage 5 due to other pathologies.
Rate of progression
Based on the rate of progression, the disease is divided into 3 degrees.
The most favorable prognosis, when maintenance therapy can prolong a normal, comfortable life for a long time, occurs with slow development.
| Degree | Rate of progression |
| Fast | Progression of the disease from stage to stage occurs in a short time with less than 2 years between them |
| Average | Progression from stage to stage occurs with 2 to 5 years between them |
| Moderate or slow | Symptoms develop slowly, progression from stage to stage lasting more than 5 years between each stage. |
Examples
With the slow development of the disease in old age, the manifestations of the disease look like normal senile impairment of motor skills and loss of strength.
At the same time, from the outside, due to the slow development of the disease, the increase in pathology is almost imperceptible. In the rapid form, violent symptoms, which manifest themselves clearly and develop in a short time, are, on the contrary, clearly visible, so it is almost impossible to miss the onset of the disease.
Symptoms of Parkinson's disease
In the early stages of development, Parkinson's disease is difficult to diagnose due to the slow development of clinical symptoms (see photo). It can manifest as pain in the extremities, which can be mistakenly associated with diseases of the spine. Depressive states can often occur.
The main manifestation of parkinsonism is akinetic-rigid syndrome, which is characterized by the following symptoms:
- Tremor. It is a rather dynamic symptom. Its appearance can be associated both with the emotional state of the patient and with his movements. For example, a tremor in the hand may decrease during conscious movements, and increase when walking or moving the other hand. Sometimes it may not exist. The frequency of oscillatory movements is small - 4-7 Hz. They can be observed in the arm, leg, and individual fingers. In addition to the extremities, trembling may occur in the lower jaw, lips and tongue. The characteristic parkinsonian tremor in the thumb and index finger resembles “pill rolling” or “coin counting.” In some patients, it may occur not only at rest, but also during movement, causing additional difficulties when eating or writing.
- Rigidity. Movement disorders caused by akinesia are aggravated by rigidity - increased muscle tone. Upon external examination of the patient, it is manifested by increased resistance to passive movements. Most often, it is uneven, which causes the appearance of the “gear wheel” phenomenon (there is a feeling that the joint consists of gear wheels). Normally, the tone of the flexor muscles prevails over the tone of the extensor muscles, so rigidity in them is more pronounced. As a result, characteristic changes in posture and gait are noted: the torso and head of such patients are tilted forward, the arms are bent at the elbows and brought to the body, the legs are slightly bent at the knees (“supplicant pose”).
- Bradykinesia. It represents a significant slowdown and impoverishment of motor activity, and is the main symptom of Parkinson's disease. It manifests itself in all muscle groups, but is most noticeable on the face due to the weakening of facial muscle activity (hypomimia). Due to the rare blinking of the eyes, the gaze seems heavy and piercing. With bradykinesia, speech becomes monotonous and muffled. Due to impaired swallowing movements, drooling may occur. Fine motor skills of the fingers are also depleted: patients have difficulty making familiar movements, such as fastening buttons. When writing, transient micrographia is observed: towards the end of the line, the letters become small and illegible.
- Postural instability. It is a special disorder of coordination of movements when walking, caused by the loss of postural reflexes involved in maintaining balance. This symptom appears at a late stage of the disease. Such patients experience some difficulty in changing posture, changing direction of movement, and starting to walk. If you push the patient out of balance with a small push, he will be forced to take several quick short steps forward or backward (propulsion or retropulsion) in order to “catch up” with the center of gravity of the body and not lose balance. The gait becomes mincing, “shuffling.” The consequence of these changes is frequent falls. Postural instability is difficult to treat and is often the reason why a patient with Parkinson's disease becomes bedridden. Movement disorders in parkinsonism are often combined with other disorders.
Mental disorders:
- Cognitive disorders (dementia) - memory is impaired, slow vision appears. With a severe course of the disease, serious cognitive problems arise - dementia, decreased cognitive activity, the ability to reason sensibly, and express thoughts. There is no effective way to slow the development of dementia, but clinical studies show that the use of Rivastigmine and Donepezil somewhat reduces such symptoms.
- Emotional changes - depression, it is the very first symptom of Parkenson's disease. Patients lose self-confidence, are afraid of new situations, avoid communication even with friends, pessimism and irritability appear. You experience increased sleepiness during the day, disturbed sleep at night, nightmares, and overly emotional dreams. It is unacceptable to use any medications to improve sleep without a doctor's recommendation.
Autonomic disorders:
- Orthostatic hypotension is a decrease in blood pressure when changing body position (when a person stands up suddenly), this leads to a decrease in blood supply to the brain, dizziness and sometimes fainting.
- Gastrointestinal disorders are associated with impaired intestinal motility - constipation associated with inertia, poor nutrition, and limited drinking. Constipation is also caused by taking anti-parkinsonism medications.
- Decreased sweating and increased skin greasiness - the skin on the face becomes oily, especially in the area of the nose, forehead, and head (provokes the occurrence of dandruff). In some cases, it may be the other way around, the skin becomes too dry. Conventional dermatological treatment improves skin condition.
- Increased urination or, conversely, difficulty emptying the bladder.
Other characteristic symptoms:
- Difficulty eating - this is due to limited motor activity of the muscles responsible for chewing and swallowing, and increased salivation occurs. Retention of saliva in the mouth can lead to choking.
- Problems with speech - difficulty starting a conversation, monotony of speech, repetition of words, too fast or slurred speech is observed in 50% of patients.
- Sexual dysfunction - depression, taking antidepressants, poor circulation lead to erectile dysfunction and decreased sexual desire.
- Muscle pain - aches in the joints and muscles are caused by poor posture and muscle stiffness, the use of levodopa reduces such pain, and certain types of exercise also help.
- Muscle spasms - due to lack of movement in patients (muscle stiffness), muscle spasms occur, more often in the lower extremities; massage, warming, and stretching help to reduce the frequency of cramps.
- Fatigue, weakness - increased fatigue usually worsens in the evening and is associated with problems starting and ending movements; it can also be associated with depression and insomnia. Establishing a clear sleep and rest schedule, and reducing physical activity helps reduce fatigue.
It is worth noting that the course of the disease is individual for each person. Therefore, some symptoms may predominate, while others may be mild. Signs of the disease are amenable to drug therapy. In some cases, surgery can effectively combat the disease.
Clinical signs of stage five Parkinson's disease
At the last stage of Parkinson's disease, patients experience motor fluctuations, drug-induced dyskinesias, walking is impaired, they fall or freeze in place. Akinetic and non-motor (vegetative, cognitive, neuropsychic) crises are characteristic.
Motor fluctuations are manifested by the phenomenon of “depletion of the effect of a single and daily dose,” freezing, and the “on-off” phenomenon. In later stages, patients experience long periods of decompensation, lasting from several days to several weeks, as well as akinetic crises. They are accompanied by dysphagia, oliguria, hyperthermia, autonomic disorders, and confusion.
The last stage of Parkinson's disease is characterized by the progression of all symptoms:
- motor disorders;
- tremors and stiffness of movements;
- swallowing disorders;
- inability to control urination and bowel movements.
At the last stage of Parkinson's disease, the patient is in a wheelchair and is fed with a special spoon. Dementia and severe depression often develop, and suicidal thoughts arise. Neurologists at the Yusupov Hospital are successfully removing patients from this condition. Doctors use modern treatment regimens for the disease with effective drugs that reduce the severity of symptoms and prolong life expectancy.
Diagnostics
Comprehensive diagnosis of the disease is based on the study of the neurological status, patient complaints and a combination of a number of criteria.
Among the instrumental research methods, the most reliable is positron emission tomography (PET), in which radioactive fluorodopa is injected intravenously and the degree of its accumulation in specific areas of the brain is assessed. The disadvantage of the method is its high cost and low prevalence. Other laboratory and instrumental methods do not reliably identify the causes of the disease and prescribe its treatment, therefore they are used to exclude other diseases with similar symptoms.
To make a diagnosis, a combination of hypokinesia with one or more signs (rest tremor (frequency 4-6 Hz), muscle rigidity, postural disturbances) is necessary.
Clinical forms of parkinsonism
Depending on the prevalence of symptoms, there are several forms of the syndrome.
Rigid-bradykinetic form
This form is characterized by limited mobility at the very beginning of movements. A person feels muscle stiffness. When activity occurs, the range of movements increases.
Trembling-rigid
The trembling-rigid form is characterized by headache, trembling and muscle stiffness. The progression of hypokinesia causes more noticeable dynamics in the neurological status.
Trembling
Trembling is one of the main symptoms of parkinsonism. In this form, it prevails over other characteristics. In this case, tremors of the arms, legs, and head are noted. Trembling of each limb may occur to a greater or lesser extent. During movements and sleep, the tremor subsides or disappears. As a result, a typical posture is observed - the head is lowered, the arms are in a bent state at the joints. In addition, poor facial expressions are noted. The trembling form is considered relatively favorable.
Signs and symptoms of parkinsonism become more common as people age. They do not always indicate a true disease. About 80% of cases of the syndrome are due to Parkinson's disease. It is characterized by a steady increase in severe symptoms. The doctor pays attention to additional symptoms and also uses instrumental diagnostics to make the correct diagnosis.
In some cases, a false syndrome appears. When the etiological factor is eliminated, it disappears without a trace or manifests itself with scant signs. Parkinson's disease requires patient care and lifelong use of medications prescribed by a doctor.
Treatment of Parkinson's disease
This disease is incurable; all modern drugs for therapy only alleviate the symptoms of Parkinson's disease. Symptomatic treatment is aimed at eliminating movement disorders.
How to treat Parkinson's disease? In the early stages of the disease, feasible physical activity and physical therapy are indicated. Treatment with drugs should be started as late as possible, since with long-term use of medications, the patient develops addiction, a forced increase in dosage and, as a result, increased side effects.
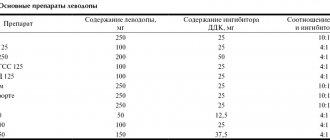
- For severe clinical manifestations of parkinsonism, levodopa is currently the basic drug, usually in combination with a decarboxylase inhibitor. Doses are increased slowly over several weeks until clinical effect is achieved. Side effects of the drug are dystonic disorders and psychosis. Levodopa, entering the central nervous system, is decarboxylated into dopamine, which is necessary for the normal function of the basal ganglia. The drug affects primarily akinesia and, to a lesser extent, other symptoms. When combining levodopa with a decarboxylase inhibitor, the dose of levodopa can be reduced and thereby reduce the risk of side effects.
- In the arsenal of symptomatic antiparkinsonian drugs, a large place is occupied by anticholinergic drugs, which, by blocking m- and n-cholinergic receptors, promote relaxation of striated and smooth muscles, reduce violent movements and the phenomena of bradykinesia. These are natural and synthetic atropine-like drugs: bellazone (romparkin), norakin, combipark. Phenothiazine drugs are also used: dynesin, deparkol, parsidol, diprazine. The main reason for the variety of medications used to treat parkinsonism is their insufficient therapeutic effectiveness, the presence of side effects, individual intolerance and rapid addiction to them.
- The morphological and biochemical changes in Parkinson's disease are so complex, and the course of the disease and its consequences are so severe, and are also aggravated by the effects of replacement therapy - levodopa, that the treatment of such patients is considered the height of medical skill and is subject to virtuosos - neurologists. Therefore, special centers for the treatment of parkinsonism are open and operating, where the diagnosis is clarified, observation is carried out, and doses of necessary drugs and treatment regimens are selected. You cannot prescribe or take medications on your own.
For replacement therapy, levodopa, carbidopa, and nacom are used. Adamantine, memantine, bromocriptine stimulate the release of dopamine, inhibit the process of dopamine reuptake - anticholinesterase drugs and tricyclic antidepressants (amitriptyline), inhibit the breakdown of dopamine selegiline, antioxidants are used as neuroprotectors of DA neurons - selegiline, tocopherol, calcium channel blockers - nifidipine.
In the early stages, the use of pramipexole (Mirapex) has been proven to preserve quality of life. It is a first-line drug for the treatment of Parkinson's disease with a high level of efficacy and safety. The treatment uses umex, neomidantan, neuroprotectors, and antioxidants. Patients need therapeutic exercises according to an individual program - to move as much as possible and stay active longer.
Treatment tactics
The treatment regimen is selected individually, depending on the stage of the disease and its clinical manifestations. Treatment will be more effective if the disease is recognized in the early stages. This way you can slow down the development of symptoms and maintain a person’s ability to work for 10 years or more. However, specialists at the Clinical Brain Institute have experience in successfully treating patients, including those in late stages.
In the early stages
Early diagnosis of Parkinson's disease is the key to the effectiveness of drug therapy. However, starting it when the first symptoms appear is not always advisable. It is necessary to take into account the patient’s age, the individual course of the disease, his social status and professional affiliation. The goal of treating the disease in the early stages is the maximum possible restoration of nervous activity through the use of minimal doses of drugs.
If the patient retains the ability to self-care, and his age does not reach 60-70 years, doctors tend to delay the use of levodopa on a regular basis. As an alternative, drugs are offered that enhance the synthesis of dopamine and stimulate its conversion. This way they prevent the destruction and death of nerve cells. The list of medications that are suitable for relieving symptoms of Parkinson's disease in the early stages includes:
- amantadine;
- dopamine receptor agonists (piribedil, pramipexole and others);
- selective MAO-B inhibitors.
These drugs are less effective than levodopa, a specific antiparkinsonian drug. However, they are suitable for stabilizing a person's condition in the early stages of the disease, as well as for reducing the dosage of levodopa in later stages. The dosage of medications is determined individually - they are prescribed in minimal doses that cause a positive response.
At a late stage
Parkinson's disease gradually progresses, regardless of the timeliness of starting therapy. This process is also due to side effects from taking levadopa. With prolonged regular use, this drug causes drug-induced dyskinesias - additional movement disorders. In addition, the natural sensitivity of dopamine receptors decreases. The only way to stop the manifestations of parkinsonism is to increase the dose of medication, which, in turn, leads to worsening side effects. At this stage, correction of the treatment regimen is required in one of the following ways:
- prescribing an additional dose of levadopa to reduce the interval between doses;
- taking drugs from the group of catechol-O-methyltransferase inhibitors;
- combined use of levadopa with entacapone.
The main complication of drug treatment for Parkinson's disease is drug-induced dyskinesia. This side effect is observed in the case of long-term use of both levadopa and dopamine receptor agonists. These symptoms often appear immediately after taking the drug, therefore, to reduce their intensity, a reduction in the single dosage of the drug while maintaining the daily dose is indicated. In addition, at the initial stages of therapy, minimal amounts of medications are selected that can cause positive dynamics.
In some cases, when conservative treatment is ineffective, surgery is prescribed. It can be performed by thalatomy or pallidotomy. In the first case, the surgeon destroys the anterior intermediate nucleus of the thalamus with a needle. This leads to a significant reduction in tremors and other symptoms of the disease. Neurostimulation of the brain is considered a less invasive and more effective method of surgical treatment of Parkinson's disease. To do this, electrodes are placed in separate areas of the brain, which receive impulses from a stimulator located subcutaneously in the chest area. This technique gives good results and is used mainly in developed countries.
Neurostimulation
Neurostimulation is a modern treatment method that is a minimally invasive neurosurgical operation.
This method is used in the following cases:
- Despite correctly selected drug therapy, the patient is unable to achieve a significant reduction in symptoms.
- The patient is socially active and is afraid of losing his job due to the disease.
- Progression of the disease leads to the need to increase doses of medications, and the side effects of the drugs become intolerable.
- The patient loses the ability to care for himself and becomes dependent on his family to perform daily activities.
Results of the operation:
- Allows non-invasive adjustment of stimulation settings as the disease progresses;
- Unlike palidotomy and thalamotomy, it is reversible;
- The period of effective control over the symptoms of the disease increases;
- The need for antiparkinsonian medications is significantly reduced;
- Can be bilateral (that is, effective for symptoms on both sides of the body);
- It is easily tolerated and is a safe method.
Disadvantages of neurostimulation:
- Relatively high cost;
- Possibility of electrodes moving or breaking; in these cases (15%) repeat surgery is needed;
- The need to replace the generator (after 3-7 years);
- Some risk of infectious complications (3-5%).
The essence of the method: the therapeutic effect is achieved by stimulating certain brain structures responsible for controlling body movements with a precisely calculated small amplitude electric current. To do this, thin electrodes are inserted into the patient's brain and connected to a neurostimulator (similar to a pacemaker) implanted subcutaneously in the chest area under the collarbone.
Types of parkinsonism
Prevalence of the most common types of parkinsonism:
- idiopathic Parkinson's disease accounts for approximately 85% of all cases of parkinsonism;
- medicinal - about 8%;
- multiple system atrophy (classified as atypical (AP)) - 2.5%;
- progressive supranuclear palsy, corticobasal degeneration (related to AP) - 1.5%;
- vascular - approximately 3%;
- postencephalitic – 0.5%.
Idiopathic parkinsonism
The destruction of dopamine neurons leads to the development of idiopathic parkinsonism. The pathology cannot be cured completely and requires constant medical support. Occurs in people over 55 years of age.
Characteristic features include:
- asymmetrical manifestation of tremors;
- speech disorder;
- there are no involuntary movements during movement.
This form is characterized by lack of strength, asthenia, and lack of sleep. Habitual actions are performed with great difficulty. Trembling covers the fingers and eventually spreads to the lower limbs. During emotional experiences, trembling becomes more pronounced. During sleep, the tremor stops.
Drug-induced parkinsonism
The cause of the syndrome is associated with the use of drugs, for example, those related to antipsychotics. They suppress the functioning of dopamine receptors.
Neuroleptic parkinsonism is characterized by rapid progression. A characteristic symptom is a bilateral manifestation. In addition, there is no tremor at rest.
After discontinuation of the drugs, the symptoms disappear. However, this process is lengthy and lasts several months. If the drugs are not removed from use, the pathology will progress all the time.
Vascular parkinsonism
With secondary damage to the tissue of the nervous system, which occurs, for example, against the background of a stroke, vascular parkinsonism may appear. It is characterized by symmetry, that is, symptoms appear simultaneously on both sides, and there is no trembling at rest. Associated symptoms include:
- urination disorder;
- dementia;
- ataxia.
Postencephalitic parkinsonism
The transferred encephalitis does not end without a trace. After the illness, symptoms resembling parkinsonism may appear. In addition, the disease is accompanied by endocrine disorders, as well as the manifestation of vascular, psychogenic signs. In this form, increased tendon reflexes are diagnosed.
Toxic parkinsonism
With prolonged contact of the body with substances such as mercury, carbon monoxide, lead, damage to neurons occurs with the subsequent development of toxic parkinsonism. Often this form of the disease develops in response to drug use.
The localization of the pathological change in the nervous system is reflected in the manifestation of symptoms, as well as the response to levodopa drugs. Cessation of exposure to harmful substances leads to regression of symptoms.
Manganese parkinsonism
Manganese parasite is formed by prolonged inhalation of manganese compounds. The syndrome was noted in the 19th century among ore miners. At the same time, gait and pronunciation of words were impaired, and increased salivation was noted.
Manganese toxicity can occur with prolonged parenteral nutrition, liver and kidney failure, and in individuals on hemodialysis.
The main clinical manifestations include:
- difficulty speaking;
- slow movements;
- muscle rigidity;
- gait disturbance.
MRI results indicate the presence of manganese in the basal ganglia. This type of parkinsonism cannot be treated with levodopa. After exposure to the substance ceases, the disorder continues to progress for several years.
Treatment using stem cells.
The results of the first trials on the use of stem cells in Parkinson's disease were published in 2009. According to the data obtained, 36 months after the introduction of stem cells, a positive effect was observed in 80% of patients. The treatment involves transplanting neurons obtained from differentiated stem cells into the brain. Theoretically, they should replace dead dopamine-secreting cells. As of the second half of 2011, the method has not been sufficiently studied and does not have widespread clinical application.
In 2003, for the first time, genetic vectors containing the gene responsible for the synthesis of glutamate decarboxylase were introduced into the subthalamic nucleus of a person with Parkinson's disease. This enzyme reduces the activity of the subthalamic nucleus. As a result, it has a positive therapeutic effect. Despite the good treatment results obtained, as of the first half of 2011, the technique is practically not used and is in the stage of clinical trials.
Physiotherapy
Patients may develop joint contractures as a result of impaired tone and hypokinesia, for example, shoulder-scapular periarthrosis. Patients are recommended to follow a low-cholesterol diet and a low-protein diet. For normal absorption of levodopa, protein products should be taken no earlier than an hour after taking the medicine. Psychotherapy and reflexology are indicated.
Maintaining physical activity stimulates the production of internal (endogenous) neurotransmitters. Scientific research is being conducted on the treatment of parkinsonism: these include stem and dopamine-producing cells, a vaccine against Parkinson’s disease, surgical treatment - thalamotomy, pallidotomy, high-frequency deep stimulation of the subthalamic nucleus or the internal segment of the globus pallidus and new pharmacological drugs.
Folk remedies
The patient will not be able to cope without drug treatment. Traditional medicine methods for Parkinson's disease will only slightly alleviate his condition.
- Patients often suffer from sleep disturbances; they may wake up repeatedly during the night and walk around the room in a half-asleep state. In doing so, they bump into furniture and can seriously injure themselves. Therefore, a patient suffering from parkinsonism should create an extremely comfortable environment for night rest.
- The patient will benefit from foot baths with fern decoction. To prepare the decoction you need to take 5 tbsp. l. dry rhizomes, add 5 liters of water and boil for at least 2 hours. Cool the broth and prepare a foot bath.
- A mixture of freshly squeezed juices of plantain leaves, nettle and celery will help reduce clinical manifestations.
- Herbal teas are prepared from linden blossom, chamomile, sage or thyme. It is better to take plants separately, adding to 1 tbsp. l. substrate 1 tsp. dry motherwort herb for a sedative effect. At 2 tbsp. l. of the medicinal plant, take 500 ml of boiling water and infuse it in a bowl covered with a towel.
Before using any products from this category, you should consult your doctor!
Forecast for life
The prognosis is conditionally unfavorable - Parkinson's disease is steadily progressing. Symptoms of movement disorders develop most quickly. Patients who do not receive treatment, on average, lose the ability to care for themselves after 8 years from the onset of the disease, and after 10 years they become bedridden.
- As of the second half of 2011, the vast majority of patients are receiving appropriate treatment. The prognosis in this group is better compared to patients who do not receive adequate therapy. Individuals taking levodopa become dependent on their caregivers after an average of 15 years. However, in each specific case the rate of progression of the disease is different. It has been noted that with the relatively early development of Parkinson's disease, symptoms of impaired motor activity progress most quickly, and when the first symptoms of the disease appear in people 70 years of age and older, mental disorders come to the fore.
- Adequate therapy slows down the development of a number of symptoms leading to disability in patients (muscle rigidity, hypokinesia, postural instability, etc.). However, 10 years after the onset of the disease, the working capacity of most patients is significantly reduced.
The life expectancy of patients is reduced. The ability to work in these patients is permanently and irreversibly lost; depending on the severity of neurological disorders, patients are assigned a disability group.
Determination of disability according to the degree of Parkinson's development
There is an opinion that all people diagnosed with Parkinson's are officially recognized as disabled. In reality, the situation is somewhat different. In the first stages, the disease does not have a serious impact on a person’s normal life and does not interfere with his ability to work, so doctors do not consider him incompetent. As the disease progresses, the situation worsens, but even then the degree of disability is determined in accordance with the rules.
Disability in the first degree of Parkinson's
Stage 1 Parkinson's disease does not reduce a person's motor activity, although the symptoms already affect one limb. At this stage, trembling may be invisible not only to the people around the patient, but also to himself. In this case, work activity is practically not affected. Excessive fatigue and some discomfort in the muscles are certainly present in daily life, but the person remains able to fulfill his usual obligations.
Only activities related to personal life and hobbies decrease, since in his free time the patient prefers to relax in silence, mistaking the existing signs of impairment for physical weakness characteristic of his age. Parkinson's degree 1 persists on average for up to 3 years, after which deterioration occurs and motor capabilities sharply decrease.
Disability in Parkinson's disease 2 degrees
The answer to the question at what degree of Parkinson’s disability is given can be unequivocal - the medical and social commission makes a positive decision starting from the second stage of the disease, although not always. At this stage, the disorder already affects both the left and right sides of the body. The patient still maintains her balance well, but rigidity and bradykinesia become more pronounced, so it becomes more difficult to carry out work activities.
If the symptoms of the disease manifest themselves so sharply that the patient cannot spend as much time at work as before without reducing the quality of the result, doctors may decide to assign him a 3rd disability group. This does not necessarily happen immediately after the disease affects the other side of the body. Stage 2 Parkinson's disease can last up to 7-10 years and a decrease in work activity occurs at different times.
Disability and Parkinson's disease 3 degrees
Parkinson's degree 2 practically does not change the patient's quality of life, which cannot be said about the next stage of the disease. The third stage of the disease is primarily characterized by postural instability. The ability to maintain normal balance is lost with any attempt to change body position. In addition to this, tremors of all extremities intensify, significantly reducing physical capabilities.
Parkinson's degree 3 still allows the patient to care for himself independently, therefore, during a medical and social commission, a decision is made to assign a second or third disability group. The duration of this stage of the disease with normal treatment can be up to 15 years, although only a few achieve this result, mainly those who became victims of the disorder at a fairly young age.
Disability with Parkinson's 4 degrees
Parkinson's stage 4 means that a person gradually becomes immobile. Even turning over while lying in bed is becoming more and more difficult for him every day; he cannot get out of it on his own. We are not talking about active work at this stage. The patient’s well-being deteriorates sharply, and the quality of life decreases. He can still walk or stand on his own, but only if there is a person nearby who can help him up and support him.
At this stage, the commission decides to assign a second or even first disability group, depending on many factors. The patient remains in this condition for a relatively short time - a maximum of 5 years. after this there is a transition to the last stage of the disease.
Disability in Parkinson's 5th degree
The last stage of the disease leads to severe disability and the patient is guaranteed to receive group 1 disability. The patient cannot take care of himself or move around. At best, he ends up confined to a wheelchair, at worst, to a bed. Even eating without assistance becomes impossible.
It is very difficult to judge life expectancy in such conditions. The fact is that ultimately it is not Parkinson itself that kills patients, but the accompanying problems. Thus, at the fifth stage of the disease, due to problems with swallowing and chewing, pneumonia or other similar diseases become a common cause of death.
Depending on what degree of Parkinson’s is detected in the patient and how competent the treatment is prescribed to him, the conditions in which he should live are determined. The first and second stages make it possible not to change your usual way of life, at least in relation to most things. In the third and fourth cases, it is better for the patient to move to relatives who will provide assistance in self-care.
Stage five Parkinson's is often called terminal. Nothing can help the patient in her treatment, but you can try to ensure at least some comfortable stay. Often at this stage of the development of the disease it is recommended to seek help from professional nurses or a boarding house. Providing comfort for the patient on your own is too labor-intensive.
Prevention
In order to reduce the risk of Parkinson's disease, you should adhere to the following preventive measures:
- Timely diagnose and treat vascular pathologies of the brain associated with injuries or infections. In this way, dysfunction of dopamine production will be avoided.
- Follow the timing of taking neurolipeptic drugs. They can be used for no more than 1 month without interruption.
- Consult a doctor if you notice the slightest signs of Parkinson's disease.
- Substances that are really able to protect neurons are flavonoids and anthocyanins. They can be found in apples and citrus fruits.
- It is worth protecting the nervous system by avoiding stress, leading a healthy lifestyle, and exercising.
- Increasing scientific evidence indicates that smokers and coffee drinkers have virtually no incidence of Parkinson's disease. But this is a rather specific preventive measure that should not be considered as a recommendation. Moreover, when a disease is detected, there is no point in starting to smoke or drink coffee, since this does not in any way affect the course of pathological processes. However, in the absence of contraindications, you can consume minimal doses of natural coffee on a regular basis.
- It is beneficial to eat a diet that is rich in B vitamins and fiber.
- Avoid contact with harmful substances that affect the development of the disease, such as manganese, carbon monoxide, opiates, pesticides.
New research shows that berries can have an impact on the risk of disease.
Parkinsonism syndrome - what is it?
Parkinsonism is changes in the central nervous system that lead to motor disorders in the form of:
- trembling of the limbs at rest is the main sign by which the disease is primarily judged. Usually one arm or leg begins to tremble. Subsequently, the tremor spreads to the entire limb;
- decreased mobility or initiative to move;
- changes in speech – a person speaks monotonously, the voice changes, the pronunciation of words changes;
- there is a tendency for phrases to fade at the end of a sentence;
- gait disturbances – shuffling appears when walking;
- mental problems – there may be increased anxiety, depression;
- stiffness of individual muscle groups.
Parkinson's disease and parkinsonism are not equivalent concepts. The latter can be an independent disease or manifest itself as a syndrome of other diseases of the nervous system.