Symptoms
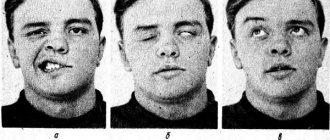
The inflammatory process begins to develop gradually. At first there may be a feeling of pain behind the ear, but after a few days facial asymmetry occurs. The patient has a drooping corner of the mouth on one side, and the eye on the affected side squints poorly. When you try to close your lips into a “tube” on the affected side, your mouth becomes distorted. When you try to “blow out the candle,” the cheek on the affected side “sails.” There may be lacrimation from the eye on the affected side. With this pathology, a person loses the sense of taste on the front of the tongue. Hearing disturbance and increased salivation may occur. When closing an eye on the affected part of the face, the eye may not close completely. The patient's smile is asymmetrical. Symptoms develop over one or two days.
Treatment
Treatment of facial nerve neuritis is carried out on an outpatient basis. The exception is cases of illness associated with ear pathology that require surgical intervention.
- At home, it is necessary to spare the organs of vision. Due to incomplete closure of the eyelids, the cornea of the eye quickly dries out, so it must be constantly moistened with special drops, wear dark glasses during the day, and cover the eyes with a bandage at night.
- The basis of treatment for facial neuritis is glucocorticoid preparations (prednisolone), which are often supplemented with non-steroidal anti-inflammatory and antiviral drugs.
- If facial neuritis is caused by damage to the part of the nerve that runs in the labyrinth, middle ear or mastoid process, then only surgery will bring the best results.
- In severe cases, accompanied by paralysis of facial muscles, microsurgical neurological operations are performed to stitch or transplant nerves.
Reconstructive surgeries that are performed on patients with severe cases of facial neuropathy:
- movement of the branches of the hypoglossal nerve to the distal end of the facial nerve;
- transposition of the temporal muscle to the corner of the mouth, which allows you to learn how to raise its corner;
- transplantation of a muscle flap from the thigh while preserving the nerve branches;
- plastic surgery – brow lift, face lift, partial lip resection, eyelid correction.
Tests and diagnostics
A neurologist makes a diagnosis based on the patient’s complaints and clinical picture. The neurologist may ask you to make movements with your facial muscles - close your eyes, bare your teeth, raise your eyebrows, puff out your cheeks or whistle, and wrinkle your nose. Such tests allow the doctor to determine the presence of neuritis. If the diagnosis is in doubt, the doctor may prescribe the following tests:
- CT, MRI;
- Electroneuromyography (ENMG);
Additionally, the neurologist may recommend consultation with a neurosurgeon and otolaryngologist.
Clinic
The development of the disease is often preceded by general or local hypothermia, especially of the head. Symptoms of a general illness (fever, general weakness) are not typical for idiopathic NLN; if they occur, it is important to exclude secondary LLN (especially those developing against the background of infections). The clinical picture of the disease is represented by acutely developed weakness of the facial muscles, the maximum of which is achieved within several hours or one day. Slowly increasing paresis of facial muscles (FMP; over weeks or months) is not typical for idiopathic NLN; most of such cases are subject to differential diagnosis with a space-occupying process.
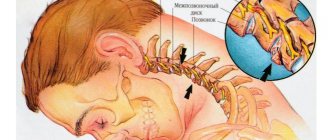
The main symptoms of NLN are caused by PMM of the upper and lower half of the face (prosopoplegia). Already at rest, the mask-like appearance of the corresponding half of the face (the face of the sphinx) attracts attention - the eye is wide open, almost does not blink; forehead without wrinkles; the nasolabial fold is smoothed; the eyebrow and corner of the mouth are lowered. The patient cannot frown, raise his eyebrows, when closing his eyes the eyelids do not close completely, the palpebral fissure gapes (lagophthalmos), when trying to close the eye, the eyeball rises upward and deviates outward (Bell's phenomenon), while the sclera is not completely covered. When smiling or laughing, half of the face is motionless; when grinning, the mouth deviates to the healthy side; when puffing out the cheeks, the diseased side “sails.” While eating, food gets stuck between the cheek and teeth, saliva and liquid food are poorly retained in the mouth, the patient cannot spit or whistle. During the acute period, the patient clearly pronounces labial sounds (b, m). Due to the slight displacement of the mouth, the protruding tongue may deviate slightly in the healthy direction.
Often, motor disturbances appear simultaneously with movement disorders, and sometimes they are preceded by usually mild and short-lived pain in the area of the mastoid process and the auricle. Other disorders may also be observed due to changes in the sweat, salivary and taste fibers of the nerve trunk, extending into the facial nerve canal at its different levels. When the facial nerve changes in the canal above the origin of the greater petrosal nerve, in addition to paralysis of the facial muscles, there is a lack of lacrimation (dry eye), sweating (dry skin of half the face), unilateral loss of taste in the anterior 2/3 of the tongue, strong, unpleasant perception of ordinary sounds (hyperacusis) . With damage below the origin of the petrosal nerve, increased lacrimation is observed, because due to the weakness of the lower eyelid, tears do not enter the lacrimal canal, but flow out, as well as taste disorders and hyperacusis. With a change below the stapedius nerve, hyperacusis does not occur; with a lesion below the origin of the chorda tympani, there are no disorders noted above, but lacrimation persists.
Lacrimation caused by weakness of the orbicularis oculi muscle is observed in 2/3 of patients with NLN; dry eye occurs much less frequently due to the involvement of lacrimal fibers. About a third of patients note a distorted, unpleasantly enhanced perception of sounds (hyperacusis) on the affected side, associated with paresis of m. stapedius Taste disturbance on the anterior 2/3 of the tongue on the affected side occurs in approximately half of the patients.
When the function of the facial nerve is impaired at the level of the geniculate ganglion, Ramsay Hunt syndrome is observed - a combination of peripheral paralysis of the facial muscles with herpetic rashes and excruciating pain in the area of the auricle, tympanic cavity, the back of the palate and the anterior half of the tongue [4].
NLN can sometimes be bilateral (diplegia facialis). Acute bilateral paralysis of facial muscles can develop with Guillain–Barré syndrome, tick-borne borreliosis (Lyme disease), tuberculous meningitis, sarcoidosis, and meningeal carcinomatosis [2, 3].
An important diagnostic and prognostic value is the study of electrical excitability of the nerve, which reveals a partial or complete reaction of degeneration, and complete is a prognostically unfavorable sign. An electromyographic study makes it possible to judge the speed of impulses along the facial nerve and its branches, as well as changes in the nucleus of the nerve.
Peripheral paralysis of the facial muscles should be distinguished from central paralysis associated with the involvement of the corticonuclear fibers of the bridge, in which the electrical excitability of the facial nerve is not qualitatively changed.
Purely clinical signs are also important in diagnosis. With NLN, the upper and lower groups of facial muscles are involved to the same extent. With central paralysis, the muscles of the lower half of the face suffer significantly more; paralysis of the muscles of the upper facial group is almost absent. The muscles of the upper parts of the face are innervated from that part of the facial nerve nucleus that receives bilateral corticonuclear pons fibers.
As a rule, the course and prognosis of idiopathic NLN are favorable. Mild cases are observed with complete restoration of facial movements within 2–3 weeks, moderate cases last about 2 months, sometimes recovery occurs only after 56 months. First, the function of the muscles of the upper half of the face is restored, then the lower half.
Most cases end with complete recovery with restoration of the functions of the facial muscles; in some cases, minimal residual symptoms remain, and in some patients, recovery is incomplete with the formation of contractures of the facial muscles and pathological synkinesis. Complete restoration of facial muscles is observed in approximately 70% of cases. The incidence of complications, in particular secondary contracture of facial muscles, is quite high and, according to various estimates, can range from 7.5 to 73.0% of cases [3]. The reason for the development of contractures of facial muscles after undergoing NLN is assumed to be the formation of the ephaptic region, where a kind of “artificial synapse” arises, transmitting impulses from one fiber to another. Postparalytic contracture is characterized by three main signs: persistent, painful tension of paretic facial muscles, the appearance of pathological synkinesis (conjugal movements), clonic-tonic spasms, tics, hyperkinesis in individual facial muscles [3].
Typically, signs of contracture appear within 3 to 6 months after the onset of NLN. Factors that provoke the occurrence of contracture of the facial muscles are long-term use of electrical procedures, early administration of anticholinesterase drugs (neostigmine methyl sulfate, galantamine), and excessively strong impact on the facial muscles during therapeutic exercises and massage [3]. With contracture, the palpebral fissure narrows on the affected side, the corner of the mouth is pulled up, and the nasolabial fold on the healthy side is smoothed out. During the study, it is established that the side on which differentiated movements are difficult has been changed. Pathological synkinesis is observed: eyelid-labial (when the eyes are closed, the forehead wrinkles and the corner of the mouth rises), eyelid-nasal (when the eyes are closed, the wing of the nose rises). When smiling, laughing, or showing teeth, an even greater narrowing of the palpebral fissure occurs at the same time, the eye may close, and when closing the eyes, the corner of the mouth tightens. More than 10 types of synkinesis have been described for contracture of facial muscles. Tics appear in the corners of the mouth, orbicularis oculi muscle, and cheeks. Mild synkinesis and isolated tic-like twitches may persist after complete restoration of the function of the facial muscles. Recurrences of LLN are possible both on the same and on the other side. They are rare and in some cases they are more severe, in others they are milder than the initial disease. With repeated episodes of PMM, a thorough examination of the patient is necessary to identify more severe diseases (carcinomatosis of the meninges, tuberculosis, sarcoidosis, etc.).
Treatment of neuritis of the facial nerve
Treatment begins with drug therapy to relieve swelling and inflammation. Treatment may include the following groups of drugs:
- glucocorticosteroids;
- vasodilators;
- diuretics;
- B vitamins (in the absence of allergic reactions);
- non-narcotic analgesics;
- Moisturizing drops may be prescribed for the eyes to prevent dry mucous membranes.
With secondary neuritis, it is necessary to treat the disease that caused the neuritis.
Causes
Facial neuritis occurs under the influence of the following etiological factors:
- in 15% of patients this is damage to the branches of the nerve during surgical interventions on the middle ear, mastoid process, and also associated with otitis media and other lesions of the hearing organ, for example, cholesteatoma;
- in rare cases, the disease is caused by infection - herpes virus (Hunt syndrome), mumps, polio, influenza, as well as Lyme disease, transmitted through tick bites;
- in 75% of cases, the cause of neuritis of the facial nerve cannot be determined; in this case, they speak of Bell's palsy, which worsens after hypothermia and colds.
Other causes include head trauma, surgery on the salivary gland, and removal of an acoustic neuroma.
Consequences and complications
Treatment must be started as quickly as possible, because
a year after the onset of the disease, the muscles will completely atrophy and their functionality cannot be restored. Complications may occur if therapy is not started at the first signs of the disease. With a long course of the disease, contracture of the facial muscles may occur, which is very difficult to restore. Disturbances in the sense of taste, visual disturbances (blindness, corneal ulcer), spasm of the muscles of the face and eyelid may occur. Consequences after the disease in some cases can last a lifetime.
Diagnostics
Neurological disorders characteristic of facial neuropathy can also occur with other diseases, in particular with stroke. That is why, if any similar symptoms occur, you should urgently consult a neurologist.
Diagnosis of pathology includes:
- collection of complaints;
- taking an anamnesis, during which the doctor clarifies the time and circumstances of the onset of symptoms, records previous and chronic diseases, injuries and other important details;
- neurological examination, during which a specialist checks skin sensitivity, motor function, muscle strength, quality of reflexes, functioning of the central nervous system, etc.;
- tests: general blood and urine analysis, biochemical blood test with mandatory determination of glucose levels, determination of antigens and antibodies to infectious diseases if their presence is suspected;
- X-ray of the chest organs: allows you to diagnose tuberculosis, tumors;
- MRI or CT scan of the brain: helps visualize tumors, areas of acute ischemia, hemorrhages, consequences of injuries and strokes;
- CT scan of the temporal bone;
- electroneuromyography: assessment of the speed of impulse transmission along nerve fibers and muscles, allows you to determine the level of damage and severity of the disease;
- consultations with specialists: therapist, otorhinolaryngologist, endocrinologist, infectious disease specialist, if necessary.
The list of studies can be adjusted depending on the specific clinical situation.