Epidural hematomas of the brain are an accumulation of blood between the cranial bones and the dura mater of the brain resulting from traumatic injury. It is considered a rare type of hematoma: according to medical statistics, it accounts for no more than one and a half percent of cases.
The Neurosurgery Department of CELT invites you to undergo diagnostics and treatment of hematomas in Moscow. Our multidisciplinary clinic has been operating in the paid medical services market for the third decade and enjoys a good reputation among patients. Our specialists have many years of practical experience and have modern techniques that allow them to carry out effective and most gentle operations.
Etiology of epidural hematomas
As already mentioned, the formation of an epidural hematoma occurs above the dura cerebral membrane, which causes its detachment from the inner cranial surface. Since under the age of two years and after sixty it is fused to the cranial bones, during these periods this type of hematoma is extremely rare. Most often it is diagnosed in male patients aged sixteen to twenty-five years who lead an active lifestyle.
An epidural hematoma occurs due to traumatic injuries. This can be a blow from a small object to a slow-moving head, or a blow to the head against a stationary object, usually when falling. Most often, the injury occurs in the area of the temples or crown, and hemorrhage occurs from the meningeal artery and its branches.
Treatment
The diagnosis of epidural hematoma is an indication for emergency surgery. A craniotomy is performed to remove liquid blood and blood clots using an aspirator. Then the source of bleeding is found and careful hemostasis is carried out. After placing a bone flap in place, the wound is sutured.
Conservative treatment methods involve managing the patient in the postoperative period and preserving the vital functions of his body. You can refrain from surgery if the volume of the hematoma is insignificant and there is no phenomenon of decompression and dislocation of the brain.
Epidural hematoma clinic
The diameter of the hematoma formed above the hard shell does not exceed eight millimeters, the volume is one hundred and twenty milliliters. Its peculiarity is that its thickness increases from the periphery to the center, and the danger is that it causes an increase in intracranial pressure and compression of brain tissue. The classic picture of hematoma formation is characterized by the presence of a clearly visible light interval, which lasts about half an hour and manifests itself as follows:
- The victim loses consciousness for a short period of time and then comes to, often maintaining an insignificant stunned state;
- He complains that he is dizzy, has a feeling of weakness and a headache of moderate intensity;
- He may experience a lack of symmetry in the nasolabial folds, as well as involuntary oscillatory movements of the eyeballs.
After this, the victim becomes worse, which is manifested by the following:
- Increased headaches;
- Depressed state of consciousness (sometimes comatose);
- Increased blood pressure;
- Facial nerve paralysis;
- Pupil dilation and lack of reaction to light.
Symptoms
Acute epidural hematoma has three main course options:
- Classic clinical picture.
At the moment of inflicting a traumatic brain injury, the patient briefly loses consciousness. Then there is a complete or partial (up to moderate stunning) restoration of the latter. The patient complains of dizziness, weakness throughout the body, and headache. Memory loss is possible - the victim does not remember events that occurred before the injury. Slightly expressed focal symptoms and meningeal signs are detected. After a few tens of minutes or hours, a sharp deterioration in the condition occurs. Psychomotor agitation develops; headache increases; vomiting occurs. Possible secondary loss of consciousness up to coma. The turn of stem symptoms comes: blood pressure rises, the pulse slows down, and respiratory rhythm disturbances appear. Upon reaching coma, severe disturbances of vital functions occur. - A variant in which the “light” gap is slightly expressed.
It's a little less common than the first one. The same phases persist: loss of consciousness, its restoration, repeated loss. However, the injury is most often very severe; the initial loss of consciousness can reach the depths of coma. Focal symptoms are severe, vital disturbances are also extremely severe. Then comes the “bright” period - a period of time during which it is possible to establish minimal verbal contact with the patient. Secondary loss of consciousness is accompanied by an increase in psychomotor agitation, brainstem syndrome, and the development of hormetonia. - A variant in which the “light” gap is absent and is not established even when collecting an anamnesis. Such patients are in a stupor or coma from the moment of injury until surgery or death.
Subacute epidural hematomas differ from acute forms in the duration of the “light” interval. In this case, this period of time takes up to one to two weeks. Focal symptoms have a smoothed severity, vital functions are slightly changed. Secondary loss of consciousness is preceded by an increase in cerebral and focal symptoms. Chronic epidural hematomas are practically never encountered in practice.
Diagnosis of epidural hematomas
In order to correctly make a diagnosis, CELT specialists conduct comprehensive studies to accurately determine the location, diameter and volume of the hematoma, as well as to determine its consequences. Instrumental diagnostic tests prescribed for the patient are presented as follows:
- X-ray of the skull to detect fractures;
- Cerebral angiography (study of cerebral vessels);
- Echoencephalography;
- Computer and magnetic resonance imaging, incl. and with contrast.
Diagnosis of the disease
The conclusion about the presence of an epidural hematoma is made by a neurologist or neurosurgeon in collaboration with a traumatologist based on anamnesis, clinical symptoms - impaired consciousness, unilateral mydriasis, the opposite hemiparesis, bradycardia. X-ray of the skull shows fractures of the bones crossing the meningeal vessels. The location of the fracture corresponds in 90% to the location of the epidural hematoma. Echoencephalography establishes the fact of a progressive displacement of the median echo. Performing an echo-EG is advisable if MRI or CT is not possible.
Cerebral angiography is one of the methods that confirms the presence of an epidural hematoma. The study indicates avascular areas in the form of a convex lens. A CT scan of the brain gives the exact size, configuration, location of the hematoma, and intracranial changes. Fusing with surrounding tissues, a small epidural hematoma is determined by performing an MRI of the brain, as well as to differentiate epidural, subdural hematomas, assessing the basal areas and the brain stem.
Treatment of epidural hematomas
When developing treatment tactics for hematomas, neurosurgeons and neuropathologists are based on the results of diagnostic studies and individual patient testimony. It may involve the use of conservative or surgical techniques.
| Hematoma treatment methods | What are they? |
| Conservative | Conservative treatment is carried out for hematomas with a volume of up to 50 mm if there is no progressive clinical picture and there are no symptoms of brain compression. It involves the use of drugs to prevent cerebral edema, relieve pain, vomiting and convulsions. |
| Neurosurgical | Surgery is the more common treatment option. Removal of the hematoma is carried out using endoscopic techniques through a specially created hole in the skull. Through it, part of it is aspirated, after which they resort to trepanation and completely remove the hematoma. The neurosurgeon also locates and ligates the damaged blood vessel using various techniques. |
The Neurosurgery Department of CELT is staffed by neurologists and neurosurgeons with many years of experience in scientific and practical work. You can make an appointment with them online on our website or by contacting our operators: +7 (495) 788 33 88.
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions
Description
Its average volume reaches one hundred and twenty milliliters; minimum - thirty, maximum - two hundred and fifty. It is seven to eight centimeters in diameter. The usual location of an epidural hematoma is one or two lobes of the brain; Hematomas of the temporal region and adjacent areas are more common. They are characterized by a thickened central part, tapering towards the periphery.
Compression of the dura mater and brain matter occurs as a result of the incompressibility of the hematoma. It seems to push through the shell with its mass, forming a dent of the appropriate size. Most often, the cause of a hematoma is the middle meningeal artery along with its branches, sometimes veins, and sinuses. Even less commonly, the source of bleeding is diploe.
In children under two years of age, the dura mater is fused with the inner surface of the skull more tightly than in adults. Therefore, epidural hematoma in children is observed much less frequently.
Medical Internet conferences
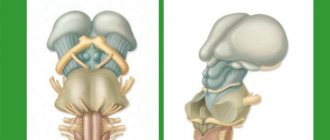
Vascular diseases of the spinal cord are often associated with acute disorders of spinal circulation. Hemorrhagic spinal stroke occurs due to rupture of an arteriovenous, arterial aneurysm or injury to the spine and spinal cord[1]. Clinical manifestations of spinal cord damage occur acutely at the time of injury or after intense physical activity[2]. The focus of hemorrhage is usually located in the gray matter of one or a number of adjacent segments, which leads to the occurrence of spinal syndromes. A picture of transverse lesions of the spinal cord with flaccid and later spastic paralysis of the limbs, with spinal conduction and segmental sensitivity disorders, dysfunction of the pelvic organs and autonomic disorders is often observed [3].
Patient O., 33 years old, working, height 180 cm, weight 100 kg. was admitted to the neurological department of the Municipal Clinical Hospital No. 9 in Saratov with complaints of weakness and numbness in the upper and lower extremities.
From the anamnesis it is known that the patient had a periodic increase in blood pressure to 160–100 mmHg for 10 years. rt. Art., took antihypertensive drugs occasionally. For 10 years, he noted periodic pain in the lumbar spine, which occurs with excessive physical activity and resolves on its own. He fell ill after a stressful situation, when during the daytime periodic shooting pain appeared in the cervical spine with irradiation to the upper limbs and chest. He did not seek medical help and did not treat himself. The next day in the morning after lifting a weight (about 10 kg), acute intense pain suddenly appeared in the cervical spine and weakness in all extremities to the point of plegia in the legs. The pain syndrome lasted about 2 hours. Hospitalized at the City Clinical Hospital No. 9 for examination and treatment.
Upon admission, the neurological status was represented by sensory disorders of the spinal conduction type from the Th3 level on both sides. Muscle strength in the upper extremities in the proximal parts - 4 points, in the distal parts - 2 points, in the lower extremities - paraplegia. Muscle tone is reduced, there is no atrophy. Tendon and periosteal reflexes are of average vivacity, without significant side differences, there are no pathological reflexes. There was a dysfunction of the pelvic organs such as periodic urinary incontinence. Meningeal symptoms were not detected.
Preliminary diagnosis: acute disorder of spinal circulation. Tetraparesis to the degree of plegia in the lower extremities. Dysfunction of the pelvic organs of the central type.
The patient underwent a CT scan of the cervical spine at levels C1 to T6. At the level C7 - Th2, a heterogeneous structure of the spinal cord was determined due to the presence of hypodense areas with blurred contours, with density indicators of 8-13 HU. Throughout the scanning area, no pronounced narrowing of the intervertebral foramina is detected; no signs of compression or restriction of the course of the spinal nerve roots in the intervertebral foramina are observed. Conclusion: Diffuse changes in the spinal cord at the C7 - Th2 level (differential diagnosis of the demyelinating process and space-occupying lesion).
An MRI of the cervical and thoracic spine was performed: MRI picture of epidural hemorrhage at the C7-Th1 level. Structural changes in the substance of the spinal cord at the C7-Th1 level are most likely compression myelopathy. MRI signs of degenerative-dystrophic changes in the cervical thoracic spine. MRI signs of degenerative-dystrophic changes in the cervical and thoracic spine.
CT angiography of the neck vessels (common carotid, external carotid and internal carotid systems) was performed. Conclusion: The tortuous course of the right vertebral artery at the level of the C4-C5 vertebrae.
Based on clinical data and the results of laboratory and instrumental examination methods, a diagnosis was made: Spontaneous epidural hemorrhage with the development of compression myelopathy at the C7-Th2 level with the development of tetraparesis to a more severe one in the lower extremities. Dysfunction of the pelvic organs of the central type. Sop: Arterial hypertension 1, risk 2.
During treatment with antihypoxants and neuroprotectors, there was an improvement in the patient's condition in the form of a decrease in the severity of tetraparesis. On the 7th day of treatment, movements appeared in the distal parts of the lower extremities, on the 10th day the patient was able to stand up independently, and on the 14th day he walked independently without support.
A clear clinical picture and a thorough neurological examination made it possible to diagnose a spinal cord lesion and determine the level of localization of pathological changes (Th3 segment). However, it was not possible to accurately establish the nature of the pathological process in the spinal cord based on clinical data. Additional research methods (MRI, CT) helped to verify the diagnosis and assess the nature of the process as epidural hemorrhage.
Differences between epidural and subdural hematomas
Subdural hematoma (SH), unlike epidural (EG), begins more slowly, this is due to the fact that the rate of venous bleeding is much less than the rate of arterial bleeding.
Other differences include:
- EG is characterized by arterial hemorrhage, while SG is characterized by venous hemorrhage.
- EG has a unilateral localization with limited distribution, SG can be either one- or two-sided with an extended distribution.
- With EG, the light period lasts one to two days, with SG it can reach several weeks.
- Symptoms of EG are focal in nature. Symptoms of HS are combined with signs of bruise and concussion.
The course of epidural hematoma of the brain can be classified according to its forms:
- acute;
- subacute;
- chronic.
Causes
The main cause of hematomas is traumatic brain injury with or without a fracture of the skull. Injuries in the elderly and children are most often associated with falls, and in young people with road traffic accidents, violent attacks, and accidents during recreation or sports. Accidents at work and when handling weapons lead to injuries.
Most often, epidural hematomas develop from small impacts. The source of bleeding in these types of hematomas is damage to the meningeal artery or rupture of the venous sinuses. The leaking blood peels off the dura mater and a hematoma forms. Most epidural formations are localized under the tentorium of the cerebellum and temporal region; they are rare in the posterior cranial fossa, but are life-threatening. The source of subdural hematomas is often veins that are damaged due to injury, bleeding from the sinuses during contusion.
If we consider non-traumatic intracranial hemorrhages, they occur when:
- Carrying out treatment with anticoagulants.
- Coagulopathies.
- Anomalies of cerebral vessels.
- Arterial hypertension.
- Hypovitaminosis C.
- Tumors.
- Meningitis and tuberculous lesions of the central nervous system .
- Convulsions.
Spontaneous subdural hematomas form on the surface of the brain adjacent to the temporal, frontal and parietal regions, but can be found in the posterior cranial fossa and the fissure between the hemispheres.
Prognosis and complications
In the case of conservative treatment of small hematomas with minor swelling, the percentage of rapid recovery is quite high. With surgical removal of hematomas with moderate decompensation, the prognosis in most cases will be favorable. The percentage of deaths is minimal.
However, if the epidural hematoma occurs without clear spaces, the mortality rate can increase to 25%. If, in addition to the epidural hematoma, a subdural hematoma is detected, the prognosis will be much worse, and then the mortality rate reaches 90%, the same applies to untimely treatment.
In most cases, with adequate and timely initiation of therapy, there are no consequences. Otherwise, the person may die. If the brain is damaged as a result of the hematoma, complete or partial paralysis may occur.
Preventive measures include only seeking medical help as soon as possible immediately after receiving a serious head injury.
Subacute form of EG
Hematoma of this form has some similarities with acute, but some differences should be highlighted:
- the clear interval occurs approximately 20 minutes after injury and can last more than ten days;
- vital functions remain intact;
- Arrhythmia and changes in blood pressure may be observed, but not always;
- consciousness does not change or signs of moderate stupor appear;
- presence of blood stagnation in the fundus.
After a light interval, a disturbance of consciousness occurs instantly and passes into the state: stunned - coma.
The chronic form of EG is almost never encountered in medical practice.
Diagnostics
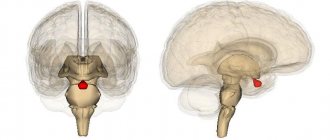
Subdural and epidural hematoma clinically do not have significant differences. Differential diagnosis is facilitated by computed tomography. Thus, on a CT scan of the brain, an epidural hematoma looks like a biconvex lens, and a subdural hematoma takes on a concave crescent shape.
Image of an epidural hematoma
When making a diagnosis, the severity of the process is determined by the time interval from the onset of injury, after which symptoms developed. For acute hematoma, this period is no more than three days, for subacute - two to three weeks, and for chronic - more than three weeks.