Hereditary factor
MS cannot be called a hereditary disease, but there is a theory according to which genes also play a role in the development of MS. To date, about 20 genes have been identified that determine the structural features of nervous tissue and may be important in the development of MS. This is confirmed by statistics: up to 20% of patients with multiple sclerosis have relatives with multiple sclerosis. However, even in the case of an existing predisposition, multiple sclerosis may not develop if other predisposing factors do not contribute to this.
ADVANTAGES OF TREATING MULTIPLE SCLEROSIS AT THE UNIVERSAL CLINIC "OBERIG"
- Diagnosis and therapy of multiple sclerosis is based on modern criteria and protocols, which are fully implemented at the Oberig Universal Clinic
- The clinic employs highly qualified neurologists with extensive experience in treating multiple sclerosis
- Our medical center has the necessary equipment for MRI of the brain and spinal cord, studies of evoked potentials of the brain, and laboratory diagnostics
Multiple sclerosis is a demyelinating disease of the nervous system. Multiple sclerosis can occur in the form of mild or, conversely, severe symptoms, such as paralysis, loss of vision, and loss of coordination.
The cause of multiple sclerosis remains unknown. In the mechanisms of development of the disease, the main role is played by the destruction of the myelin sheath of the nerves by the own immune system. At the site of damage, connective tissue (sclerosis) forms. As a result, the transmission of electrical impulses along the nerve is disrupted.
More than 2.3 million people worldwide suffer from multiple sclerosis. Diagnosis is usually made between the ages of 20 and 50 years. Two thirds of patients are women. Multiple sclerosis is more common among people in countries with cool climates.
Scientific research shows that genetic factors make some people more susceptible to the disease. But no evidence has been found that multiple sclerosis is directly inherited.
The concept of “hereditary” and “genetic” disease
A hereditary disease is a disease that arises and develops due to disturbances and damage in the genetic makeup of cells.
They can be associated with such types of mutations as chromosomal, mitochondrial and genetic.
Hereditary diseases can either be transmitted from one of the parents or as a result of mutations due to pathological changes in the embryonic tissue, zygote or in the early stages of pregnancy.
Genetic diseases are a group of diseases that arise as a result of DNA damage at the level of a specific gene.
In such cases, the disease is associated with a disorder and mutation within a gene, causing the genetic protein to change its quantity and function. Also, a genetic disease is a special case of hereditary disease.
Multiple sclerosis is not about absent-mindedness...
Many people think that multiple sclerosis is a disease of old age in which memory and attention suffer. In fact, it has nothing to do with either senile forgetfulness or absent-mindedness. This is a pathology of young people, which affects the so-called myelin sheath of the nerve fibers of the brain and spinal cord. “Sclerosis” in this case means “scar,” and “multiple” means multiple, because with multiple sclerosis, sclerosis foci are identified scattered throughout the nervous system, where normal nervous tissue is replaced by connective tissue. In this case, a person can rapidly lose vision, the ability to move normally, he develops paresis of the limbs and other disorders. This disease was first described in 1868 by a French psychiatrist, teacher of Sigmund Freud, Jean-Martin Charcot. Multiple sclerosis is a rare disease, although it is one of the most common among autoimmune diseases: it affects about three million people worldwide. About 150 thousand patients with this diagnosis are registered in Russia. What causes multiple sclerosis? How does it most often manifest itself? Can it be prevented? Are there effective methods for its prevention and treatment?
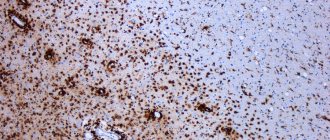
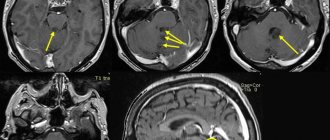
Doctors still don’t know the exact cause of multiple sclerosis, although they have been trying to study it for a century and a half. This disease occurs mainly between the ages of 14 and 40 years. The peculiarity of the disease is the simultaneous damage to several parts of the nervous system, which leads to the appearance of a variety of neurological symptoms in patients. The morphological basis of the disease is the formation of so-called multiple sclerosis plaques - foci of destruction of myelin, white matter of the brain and spinal cord. In these lesions, the normal composition of glial cells changes with an increase in the proportion of astrocytes. The size of plaques is usually from a few millimeters to several centimeters, but as the disease progresses, large fused plaques may form. They were described by pathologists as “sclerotic plaques,” hence the name of the disease. Damaged areas of brain tissue cannot perform their functions fully, which leads to disruption of the transmission of nerve impulses.
Like any other autoimmune disease, multiple sclerosis is a disease with a hereditary predisposition, the development of which is influenced by various external factors. But at the moment we do not know who may develop the disease and at what point it occurs, because the first visit to a neurologist does not coincide in time with the true onset of the disease. Its early stages are asymptomatic.
There are no warning signs for multiple sclerosis. The clinical manifestation may be the appearance of symptoms of damage to the central nervous system, and they are of a different nature in different patients. Multiple lesions occur in different areas of the central nervous system, and if they affect a clinically significant area, the patient develops one or another symptom.
Unfortunately, once it starts, multiple sclerosis cannot stop. This is a chronic disease that can neither be completely cured nor prevented. In any case, at the current stage of development of medical science. Therefore, when we say “early diagnosis,” we do not mean that we can completely cure the patient. We can stop the progression of the disease by choosing the right therapy at the earliest stages. This means that the patient will live with this disease, receive appropriate treatment and will not experience an increase in the severity of neurological symptoms.
So how can you not waste time? This is the most difficult question. After all, a person will not do an MRI of the brain and spinal cord just like that, for prevention. Unfortunately, there are no methods yet that would allow us to identify the very beginning of the disease, when there are no symptoms yet. I am sure that over time such methods will appear, because science does not stand still.
The first symptoms are associated with the fact that the inflammatory process starts when cells of the immune system affect any part of the central nervous system. But most often the disease debuts with the development of optic neuritis, when, against the background of complete health, vision in one eye begins to decrease or completely disappears, accompanied by pain when moving the eyeball. Of course, most often a person in this situation turns to an ophthalmologist. Competent ophthalmologists conduct an examination and, if they do not detect changes in the fundus, refer the patient for a consultation with a neurologist.
Another symptom that often occurs at the onset of the disease is various sensory disturbances: persistent tingling in the arm, leg, face, numbness of the tongue, half of the head. It is important that the patient does not attribute the occurrence of these symptoms to work stress or simply fatigue. If symptoms last more than 24 hours, you need to consult a neurologist. It will not necessarily be multiple sclerosis, but the doctor will already be able to distinguish damage to the central nervous system from problems of the peripheral nervous system at the first consultation.
And symptoms such as double vision or lack of coordination, tremor of the fingers should never be explained by a stressful situation or fatigue. These are already obvious signs of organic damage to the nervous system, when you definitely need to consult a specialist.
The quality of life of any person, including those with multiple sclerosis, depends on whether he can perform normal activities, go to work, start a family, and become a father or mother. And for a person with multiple sclerosis there are no exceptions here, because it affects people who are at their most active age. A person is trying to achieve something, moving up the career ladder, and at that moment he is faced with a disease. Therefore, our main task is to achieve minimal disability for the patient so that he can efficiently perform all his life functions, develop professionally, raise children, and so on.
There are many myths regarding multiple sclerosis. Much of what was previously considered completely contraindicated and inaccessible to such patients has disappeared into oblivion due to the development of diagnostics and changes in patient management tactics. One of the most common myths is that women with multiple sclerosis cannot have children. This is completely false, and many of the drugs that we use allow you to plan a pregnancy; they can also be used during lactation. If therapy is carried out correctly, such women give birth to healthy children.
Another myth: you can’t get vaccinated if you have multiple sclerosis. In fact, patients with multiple sclerosis and other autoimmune diseases can and should be vaccinated. It is especially important to say this now in connection with the COVID-19 pandemic. Of course, the timing of vaccination should be determined by neurologists, taking into account the nature of individual therapy.
By the way, multiple sclerosis itself is not a factor that increases the risk of contracting a coronavirus infection or complicates the course of the disease. But if the patient additionally has, for example, diabetes mellitus, cardiovascular diseases, obesity, or some other chronic diseases - in these cases, of course, there is a risk of a more severe course of the coronavirus infection. The number of comorbidities increases with age, so such patients are advised to stay at home to avoid infection.
If we talk about the effect of immunosuppressants and immunomodulators that our patients receive, most of these drugs do not aggravate the course of coronavirus infection, and those drugs that increase the risk of a more severe course of COVID-19 are prescribed under strict control, depending on the epidemiological situation in the city , on whether the patient has already had COVID-19, what form of multiple sclerosis he has, etc. All this is taken into account by doctors; there are recommendations for the management of patients during the COVID-19 pandemic. I would like to emphasize that it is important to resolve issues about changing or canceling therapy not on your own, but with your doctor.
For a long time, multiple sclerosis was not amenable to therapeutic interventions at all and was studied in experimental models. The first drugs were created only in 1995. They made it possible to extend the period of quality life, but, of course, they could not solve all the patients’ problems.
Over time, the line of drugs has expanded. They have different mechanisms of action, different modes of administration and different effectiveness. Nowadays, innovative drugs have appeared that can dramatically improve the quality of life of seriously ill patients, but they require constant use. There are drugs for immune reconstitution therapy (IRT), which are carried out in two short courses. After this, the patient can be out of therapy for six years or more, under the supervision of a doctor. We can assume that at this time we have cured him and this patient will not experience clinical exacerbations and changes on MRI. All appointments are made purely individually according to the clinical picture of the disease in a particular patient. There can be no self-prescription with a diagnosis of “multiple sclerosis”! So far, these drugs are recommended only for patients with highly active multiple sclerosis, for whom the risk of disability is much higher than the risk of developing possible side effects. You need to understand that with such drugs we interfere quite deeply with the immune system. This is by no means a harmless therapy. There is a risk of side effects, including serious ones, so we must be extremely careful here. But I am sure that with the development of medicine, drugs will become not only more and more effective, but also increasingly safer.
If previously we treated only relapsing-remitting multiple sclerosis, now we also treat primary progressive multiple sclerosis, in which neurological deficits are constantly increasing from the very beginning, and the main task is to stop this progression.
The latest drug, which was registered in December 2020, allows the treatment of secondary progressive multiple sclerosis, both with and without disease activity. That is, today we can specifically treat patients with multiple sclerosis with different types of progression. The main thing is to make the correct diagnosis, choose the right therapy, and correctly determine the prognosis factors.
We will not be able to completely cope with this disease until we know its etiology. Now therapy does not return the patient to normal, we simply change his immune system: we reduce the number of pro-inflammatory immune cells, increase the number of anti-inflammatory ones and thus stabilize his condition. We are still very far from understanding why the autoimmune process occurs, and so far it is not possible to create a drug that will return the immune system to normal. I hope that over time the situation will change, we will find out the cause of multiple sclerosis and learn how to treat it.
And today it is encouraging that we have drugs for immune reconstitution. They affect the immune system with a long-term prognosis, but at the same time do not affect the innate immunity necessary for protection against infections and malignancies. The balance between efficiency and safety is the main challenge we now face.
In Russia, since 2010, multiple sclerosis has been included in the so-called program of high-cost nosologies. Patients have the right to free drug supply with all drugs whose instructions indicate that they are designed for use in multiple sclerosis. This assistance is provided mainly from the federal budget.
The federal program makes multiple sclerosis therapy available throughout our country. In all regions, special centers have been created at departments or clinics. For example, in Moscow there is an outpatient neurological network consisting of five large inter-district departments within large clinical hospitals. Each district also has specialists in the field.
We strive, with the help of modern therapy, to provide the patient with a quality life, so that he is not confined to a wheelchair, locked in his apartment, and has the opportunity to communicate not only via the Internet. Unfortunately, despite the fact that we try to start treatment as early as possible and with the most modern drugs, it is not always possible to achieve a good result. The scenario for the development of the disease is individual and hardly predictable - this is generally characteristic of autoimmune processes.
It is important that the patient receives correct information about his disease and lifestyle. There are so-called white pages for patients, which are created, among other things, with the support of various foundations and pharmaceutical companies, in order to create a favorable information environment. We strive for the patient's active participation in the fight against the disease. Not only doctors and social services, but also close people and friends should help him with this. So that a person diagnosed with multiple sclerosis feels needed, in demand, and not lonely and hopeless.
Recorded by Natalia Leskova.
Multiple sclerosis in women
Multiple sclerosis is a disease that “prefers women”; women suffer from it three times more often than men. The disease even manifests itself in women in a special way. It's all about fluctuations in female hormonal levels, which can change not only the nature of the disease, but even treatment and prevention.
General symptoms
The disease got its name because of the “dispersal” of symptoms: they are varied and can manifest themselves in different ways (increase, decrease, disappear) during the day. Most often, vision, coordination, sensitivity are impaired, strength in the arms and legs decreases, and weakness and depression are added to all this. It is not surprising that with such complaints, patients most often go to an ophthalmologist, neurologist or therapist.
Multiple sclerosis is a chronic disease, most often occurring with exacerbations and remissions (complete or partial recoveries).
Causes of the disease
Multiple sclerosis is a disease in which one's own antibodies damage the membrane of neurons, which leads to disruption of the transmission of nerve impulses.