Schizophrenia is one of the most complex psychiatric pathologies, the complexity of which is due to its unclear etiology and unpredictable course. The exact reasons for its occurrence are unknown. Scientists only talk about factors that increase the likelihood of its development. Heredity is one of them. Let's find out whether schizophrenia is really inherited and how it happens.
In this article
- Scientists' opinions
- Statistical data
- Relatives of patients
- Cognitive abilities of patients' relatives
- Structural changes in the brain
- Influence of the male line
- Influence of the female line
- How to influence genes
- No predisposition
- Other risk factors
- Main symptoms
- When it appears
- What to do
Scientists' opinions
In the literature on schizophrenia, there are different data regarding its causes. There are even separate theories within the framework of which scientists conduct their research and try to confirm or refute certain hypotheses. Some of them:
- Dopamine. Increased production of dopamine, melatonin and serotonin leads to delusions and hallucinations in a person.
- Infectious. Chronic viral diseases, as well as streptococcal, staphylococcal and tuberculosis infections, reduce immunity and cause mental disorders.
- Neurogenetic. A defect in the corpus callosum, which connects the left and right hemispheres, leads to disruption of the coordinated functioning of the brain.
- Ecological. Environmental pollution negatively affects the development of the embryo, causes a lack of vitamins and ultimately increases the likelihood of developing psychiatric pathologies.
- Psychoanalytic. A bad relationship with an oppressive father or a strict mother, a cold atmosphere in the family, etc. can lead to the onset of the disease.
- Evolutionary. The increase in intellectual abilities due to technological progress does not coincide with the natural capabilities of the brain. Nature tries to adapt to changes, but sometimes fails.
- Traumatic. Psychiatric disorders can cause various types of trauma, including postpartum and operating room trauma.
- Genetic. If there is at least one person with schizophrenia in the family. others are more likely to develop it.
However, there may be disagreements within each of the listed theories. Some scientists claim the existence of 74 or even 100 genes that are responsible for schizophrenia, while other researchers are more reserved in their conclusions, believing that accurate data on this issue has yet to be revealed.
In general, doctors have found a set of genes that can affect the functioning of the brain. But it is quite difficult to draw a direct connection between them and schizophrenia. This is not the case when researchers took DNA, studied it, sorted the genes into dominant and recessive and found the exact chain that influenced the development of the disease. In any case, a conclusion about genetic causation will be an assumption, and not an exact scientific fact.
Today there are 3 main approaches to studying the hereditary factors of schizophrenia:
- Genetic, necessary for studying differences in gene structure.
- Pharmacogenetic, allowing the correct use of therapy, prescribing appropriate drugs and reducing side effects.
- A study of genesis aimed at studying the etiology of a disease.
In addition to studies in the genetics of schizophrenia, which do not always confirm hypotheses, scientists have statistics at their disposal that indicate that genetic factors should definitely be studied.
PsyAndNeuro.ru
Ideas about the genetic nature of schizophrenia have been debated for more than a century. Back in 1919, Kraepelin suggested a “hereditary predisposition” to the occurrence of schizophrenia: “I know of a fairly large number of cases in which siblings were simultaneously affected by dementia praecox.” However, the great psychiatrist also suggested other options for the etiology of schizophrenia, including “infections during the years of development of the body.” In the 1960s in the United States, the genetic theory of the etiology of schizophrenia was listed in textbooks along with psychoanalytic and other psychological theories. It has been argued that “the understanding of the relative role of genetic factors is still far from clear.” However, by the end of the 20th century, schizophrenia was perceived as “certainly a genetic disease...with an inherited risk of 80%-85%.” Some geneticists have even argued that "there is a strong likelihood that all or almost all cases of departure from direct genetic dependence can be explained by non-heritable changes in genetic structure or expression." In other words, according to those researchers, schizophrenia may be a 100% genetic disease, in the occurrence of which the role of environmental factors is minimal or absent.
By 2003, the Human Genome Project also ended, and there was no end to the optimistic expectations of researchers. It was expected that, using genetic analysis methods, the notorious “schizophrenia genes” would be discovered in the very near future. And by identifying these genes, it will be possible to fully understand the pathogenetic mechanisms and develop a new generation of highly effective drugs for the treatment of this disease. Such prospects inspired unprecedented optimism among researchers. Large-scale studies of more than 800 possible genes have been initiated, with more than $250 million in funding. However, the results were, to put it mildly, far from expected: “although the studies showed some clear results, other studies examining the role of the same polymorphisms found conflicting data.” Then the researchers conducted narrowly focused studies, with 25 and 86 genes, respectively, but even there “there was insufficient evidence indicating that the main polymorphisms of these genes are more associated with schizophrenia than polymorphisms of genes from the control panel, whose association with schizophrenia is not was supposed." Such discouraging results have led many scientists, in the words of geneticist Sullivan, to “abandon the genetic theory ... because it has only led us in the wrong direction, due to which much effort has been wasted.”
A small glimmer of hope has emerged with the rise of genome-wide association studies (GWAS). In the USA, the National Institute of Mental Health began to allocate more than $100 million a year for genome-wide research into schizophrenia. However, despite sampling data from more than 170,000 people obtained through the Psychiatric Genomics Consortium, the results were rather modest. It turned out that the number of identified polymorphisms with a possible association with schizophrenia exceeded 1500, and in the general population they occurred so often that their use for predictive purposes made virtually no sense. The correlation of the overall polygenic risk value with specific genes or sets of genes did not exceed the level of statistical error. Further complicating matters, many of the so-called “schizophrenia risk genes” have been linked to other psychiatric conditions, including bipolar disorder, depression, and even attention deficit hyperactivity disorder.
All this led, as Gershon et al. put it, to “disappointment in the air” among psychiatric geneticists. As geneticist Leo puts it, “The current trend in psychiatric genetics is to use huge samples to find genes with tiny effects.” The absence of any practically significant results from the colossal genetic studies of schizophrenia, which lasted throughout the first decade and a half of the 21st century, was regarded by some as one of the extremely painful defeats of modern science. Science journalist Wade caustically called the situation “the Pearl Harbor of schizophrenia research.” It's probably time to step back and rethink all the steps that led us to all this.
Inherited theories of the etiology of schizophrenia are based on family studies, studies of families with adopted children, and especially twin studies. Most calculations of hereditary risk scores have been based on the difference between concordance of schizophrenia between dizygotic (DZ) and monozygotic (MZ) twins. It is important to first understand these twin studies in order to understand why such high rates of hereditary risk have led to the widespread idea of schizophrenia as a predominantly genetic disease.
Back in 1961, Rosenthal published a now classic paper on the limitations of the twin method in schizophrenia research. Subsequently, other researchers confirmed his observations: if twin pairs were not confirmed in population registries, if there were errors in determining zygosity, if rather broad diagnostic criteria were used, the concordance rate in MZ was artificially increased. Other scientists have also noted that twins may not be representative of the general population because, compared with other people, they have a higher risk of birth injuries, lower birth weight and higher mortality. Thus, “schizophrenia may be concordant on the basis of birth trauma as much as on the basis of genetic predisposition.”
Another fundamental problem with twin studies is the underlying assumption that common external factors affect both twins from both MZ and DZ pairs in the same way. However, it is known that in about 15% of cases, one monozygotic twin receives more blood than the other (a condition called feto-fetal transfusion syndrome). Consequently, monozygotic twins are unequally exposed to hormones, drugs and infectious agents from the mother's blood. A similar phenomenon is not observed in DZ twins. In addition, twin studies assume that both MZ and DZ have the same social environment. However, numerous psychological studies have shown that MZ, but not DZ twins, spend more time together and form similar social bonds.
Another problem is that in twin studies, the influence of genes and the environment is assessed as independent forces that do not interact with each other. However, it is now known about the existence of gene-external environment interactions that occur in many diseases, including schizophrenia.
Most twin studies of schizophrenia have used special samples that are not representative of the general population. Only 6 studies from Scandinavian countries used nationwide twin registries. Taking their results together, pairwise concordance for schizophrenia in MZ twins is 28%, and for DZ twins – 6%. In addition, most twin studies did not use pairwise concordance*, but probandwise concordance; read more about the differences in methods for calculating concordance here. When calculating it, pairs in which both twins suffer from the disease are often counted 2 times (since the variable in the calculation formula is not the number of pairs of sick twins, but simply the number of sick individuals, which is then multiplied by 2), which increases the concordance rate, based on from which the hereditary risk indicator is also calculated.
To clearly demonstrate the problematic nature of twin studies, let us turn to the latest work to date, written by Hilker et al. Among MZ twins, only 12 out of 81 pairs (15%) had both twins suffering from schizophrenia. However, because the twins of some of these pairs were assessed separately, proband-by-proband concordance was determined by the authors to be 33%. This finding served as a starting point for constructing structural equations and threshold models of genetic risk, as in other twin studies of schizophrenia. The authors were aware that constructing such models implies that “twins are representative of the population,” that “both MZ and DZ twins are equally influenced by their environment,” and that “gene-environment interactions » are minimal. And as stated earlier, such assumptions were found to be incorrect. In the same study, the authors then report that the hereditary risk of schizophrenia in their data is 79%. There is clearly something fundamentally wrong with a modeling technique that produces hereditary risk values of 79% of 15% concordance among MZ twins. And yet, it was precisely on such calculations that theories about the genetic etiology of schizophrenia were originally based.
Although most estimates of hereditary risk for schizophrenia have relied on data from twin studies, some work has relied on family studies. Authors from Sweden and Denmark used national medical databases to determine how often children of people with schizophrenia have the same diagnosis. Based on these data, hereditary risk values of 64% in Sweden and 67% in Denmark were obtained. Researchers from Taiwan did a similar thing, but according to their data, the “heredity” of schizophrenia is determined by genetic factors only by 47%, and by 53% is determined by similar and different external factors.
We assume that schizophrenia, like almost all human diseases, certainly has some genetic background. We only question the view of schizophrenia as a predominantly genetic disease. Perhaps the “missing hereditary component” that arose during the transition from classical genetic to molecular genetic methods can be explained by the assumption that certain environmental factors may be built into the etiological structure of schizophrenia, which manifest themselves in the same way as genetic factors, but in essence they are not, which makes schizophrenia a “pseudogenetic” disease in its manifestations. We illustrate this with two examples: an infectious agent and a microbiome.
Toxoplasma gondii
may serve as an example of how the above hypothesis works.
T. gondii
is a widespread protozoan parasite that causes toxoplasmosis in its primary hosts, felines.
However, a large number of other mammals can be carriers of Toxoplasma. When a domestic cat becomes infected with this parasite, it sheds up to 50 million extremely tenacious T. gondii
. It is not known for certain how many oocysts are needed to infect a person, but, for example, pigs comparable in size to humans only need one.
Toxoplasmosis, like schizophrenia, runs in families, especially in families with domestic cats. Family members may eat the same contaminated food or use the same contaminated water source. Children can often become infected by playing in sand or soil contaminated with oocysts from cat feces. Like schizophrenia, Toxoplasma carriage can be transmitted from mother to child. Cases of vertical transmission have been documented, even if the mother was infected up to the 5th month before conception. During experiments on laboratory mice, it was shown that the offspring of one infected female, up to the 10th generation, were also carriers of Toxoplasma.
Regarding toxoplasmosis in twins, it has been shown that in the case of intrauterine infection, both MZ twins become carriers in 19 out of 20 cases. If infection occurs in childhood, carrier concordance is significantly lower.
The association between toxoplasmosis and schizophrenia has been shown in more than one meta-analysis. It has been reliably established that carriers of Toxoplasma have a 1.8-2.7 times greater risk of developing schizophrenia than the general population. No GWAS for schizophrenia has been able to produce similar results. In the United States, increased individual exposure to Toxoplasma has been partially associated with first episode psychosis, but not with established schizophrenia, which may be explained by the antiprotozoal properties of some antipsychotics. Moreover, one prospective study from Denmark found that shortly before the onset of psychotic and other psychiatric symptoms, a significant proportion of patients showed higher Toxoplasma seropositivity. Thus, the greater risk of T. gondii infection cannot be attributed to hospitalization or other similar events.
Therefore, if we take for granted the influence of T. gondii on a certain proportion of emerging cases of schizophrenia, the clinical and anamnestic picture will look as if we are dealing with a genetic disease. This does not mean that genes do not play any role in this process. On the contrary, the influence of polymorphisms of genes of components of the major histocompatibility complex on resistance to Toxoplasma infection has been known for many years. Interestingly, these genes showed some of the strongest associations in GWAS of schizophrenia. In addition, a study published this year showed a significant proportion of common polymorphisms associated with both the risk of Toxoplasma infection and the risk of developing schizophrenia.
Another source of “pseudogenetic” associations in schizophrenia is the human microbiome – a set of microorganisms located on the mucous membranes. The microbiome is largely inherited from the mother during and after birth, although other family members who come into contact with the child in the first months and years of life also contribute to its formation. The results of twin studies suggest a role for genetic factors, probably genetically determined characteristics of the immune system and receptors for the microbiota. However, it is shared environmental factors, rather than shared genes, that largely determine the family similarity of microbiomes.
Features of the microbiome have been shown to influence behavioral and cognitive traits in both animals and humans through a complex set of interactions, referred to for simplicity as the gut-brain-immune axis. With regard to schizophrenia, some studies have found marked changes in the microbiological composition of the gastrointestinal and oropharyngeal microbiota in individuals with schizophrenia compared to healthy subjects. In addition, an association has been established between the use of antibiotics in early life and the risk of developing schizophrenia in later years. Of course, there is also evidence that many antipsychotics themselves cause changes in the microbiome, but recent work has found that even in patients with a first episode of psychosis, the microbiome is already altered, although the role of drug therapy in this seems to be minimal. All this may indicate that changes in the microbiome may be one of the risk factors for the development of schizophrenia.
The bottom line is that schizophrenia may be a disease in the etiology of which external factors, infectious or otherwise, play a major role, but it is genetic factors that determine the degree of susceptibility to these factors. The hereditary risk in this case will be about 30%, but not 80%.
If we have indeed overestimated the role of genetic factors in the development of schizophrenia, then the failure of attempts to identify genes sufficiently associated with schizophrenia can be explained. There is also an explanation for the genetic paradox that lies in the persistence of schizophrenia in the population despite the very low birth rate of children from those suffering from it. From the beginning of the 19th century until the mid-20th century, patients with schizophrenia were kept in closed institutions, where the birth of children was an extreme rarity. But even after this, the fertility rates of people suffering from schizophrenia were at most one third of those in the general population.
Huge sums and resources have been spent on large-scale genetic research, while other promising areas of research, such as neuroinflammation, infectious agents, the microbiome, and others, have been grossly underfunded. Because of this, we probably lost a lot of time and indefinitely delayed the emergence of new, truly promising drugs for the treatment of schizophrenia. But it is the development of new, highly effective therapy that is, in fact, the point of application and the ultimate goal of fundamental research. We should try to move away from sterile, narrow genetic studies towards studies that study the influence of both genes and the environment and their interactions, and then perhaps we will have a chance to catch up.
Author of the translation: Kibitov A.A.
Source: Torrey EF, Yolken RH. Schizophrenia as a pseudogenetic disease: A call for more geneenvironmental studies. Psychiatry Res. 2019 Aug;278:146-150. doi:10.1016/j.psychres.2019.06.006. Epub 2019 Jun 4.
Statistical data
In general, schizophrenia is detected in approximately 0.5-1% of people, that is, no more than one person out of 100. As for the risks of the disease and the percentage, they are presented as follows:
- 1% is the first case in the family.
- 2% - an uncle/aunt, nephew or cousin is sick.
- 5% - the disease was in a great-grandmother or great-grandfather.
- 5% - a sibling suffers from the pathology.
- 10% - a brother or sister or 1st-3rd degree relatives are sick.
- 10% - the diagnosis was made to a grandmother or grandfather.
- 20% - the pathology is in the father or mother.
At the same time, the probability of developing pathology in a child from two schizophrenic parents is 45-60%. Among twins, the statistics are as follows: 13-17% for dizygotic twins, 47-48% for monozygotic twins.
As you can see, the closer the degree of relationship, the greater the risk of developing the disease. However, it is wrong to say 100% that having two parents with schizophrenia, the child will suffer from this pathology. There is a possibility, but not as high as many people believe.
Schizophrenia: heredity and its features – Izvilina
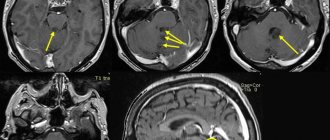
In those suffering from schizophrenia, central nervous system disorders are recorded. They are caused by damage to brain tissue by toxic and autoimmune processes that occur in the first years of life or during the perinatal period. At the same time, according to studies, similar central nervous system disorders were recorded in healthy relatives of the patient.
Given the relevance of the data obtained, experts believe that multiple disorders of impulse gene transmission may underlie schizophrenia.
Contrary to popular belief, pathology is not always transmitted to close relatives. Often, schizophrenia can occur only in grandchildren, bypassing sons and daughters.
How is schizophrenia inherited? transmission scheme
This is due to the following reasons:
- In men, the disorder manifests itself earlier.
- Schizophrenia usually appears after an event that has had a significant negative impact on the psyche of a child or adult.
- Since men perceive psycho-emotional trauma much more severely, their disease develops faster.
Statistics say otherwise. In fact, when only the mother in a family has schizophrenia, the chance that the disorder will be passed on to the child will be 5 times higher than if the father is sick. Boys are especially at risk.
However, there are some features:
- if schizophrenia was “activated” in a child of twins, then 50% of the second child will also have it, sooner or later;
- if both parents had schizophrenia, their children have a 50% chance of developing the disease;
- Identical twins have a 50% chance, fraternal twins are luckier - they get sick in 13% of cases.
When only one parent has schizophrenia, the chance of inheritance is 5-10%. If the disease is detected in a sibling, the manifestation of schizophrenia in other children varies from 6 to 12%. If a grandfather or grandmother had schizophrenia in the family, then the chance of transmission will be 5%. However, anyone with normal genetics also has a chance of getting this disorder. It is equal to only 1%.
A family history of schizophrenia may manifest itself as impaired cognitive function.
How to avoid being at risk
To do this you need:
- Lead a healthy lifestyle.
- It is necessary to give up alcohol and any substances that can affect the psyche.
- It is also advisable to establish a diet and engage in physical activity.
- It is required to undergo regular examinations with a psychologist.
Self-medication is strictly prohibited. It is necessary to share experiences, this will help to avoid apathy and further development of pathology. Stressful situations or too high loads should not be allowed.
With the right approach, schizophrenia is quite treatable and the patient can live a fairly long life with a clear memory and mind.
Relatives of patients
According to modern genetic research, not only specific pathologies are genetically determined, but also various aspects of personality, for example, a high level of anxiety or, on the contrary, excessive calmness and shyness. A tendency toward aggression, wariness, sensitivity to criticism, and the ability to react to new circumstances may also be inherited.
Similar data can be obtained from studies of identical twins who are raised in different conditions. Even with different upbringings, common traits of character and temperament can be traced. And this even applies to the love of risk and adventure.
In general, the genetic factor plays an important role in pathologies such as schizophrenia and autism. It is also subject to close study when analyzing various affective disorders and hyperactivity. At the same time, scientists find not only behavioral similarities, but also biochemical and immunological ones.
This means that the blood composition, the number of lymphocytes and other biological indicators in patients with schizophrenia largely coincide with similar data in their relatives, even if the latter do not have psychiatric disorders.
Scientists suggest considering 3 categories of relatives who have patients with schizophrenia in their family:
- People with schizoid traits - isolation, loneliness, focus on the internal rather than the external world.
- Persons with schizoid features and severe emotional defects.
- Individuals with schizoid traits with affective disorders (bipolar phase change, seasonal depression, etc.).
Statistics show that about 20-30% of first-degree relatives of people with schizophrenia complain of certain symptoms. In this case, there is no diagnosis, and therefore they talk about so-called “spectral disorders”. The symptoms are quite weak and more indicative of isolation, vulnerability and low emotional intelligence. They are also observed in many schizophrenics, especially before the onset of an attack.
Cognitive abilities of patients' relatives
Among relatives of patients with schizophrenia, if we talk about the cognitive (cognitive) sphere, the following patterns are observed:
- Altered psychomotor speed.
- Impaired visual and short-term verbal memory.
- Instability of attention.
- Unusual formation of judgments (abstractness).
- Difficulties in organizing an action plan.
- Difficulty in copying images.
But this does not apply to all relatives. Most people either do not have these signs or compensate for them with sufficient intellectual activity. However, it is wrong to exclude the presence of these patterns in the analysis.
Influence of the male line
In men, schizophrenia appears earlier and is accompanied by more obvious symptoms. Therefore, it is important for doctors to understand whether it is inherited more often from the father than from the mother. In general, the following patterns are observed:
- Men are prone to developing psychiatric pathologies already in childhood or adolescence.
- Such diseases progress rapidly in them.
- The impetus for the development of a disease or attack can be a minor factor.
- Men, in principle, are more susceptible to neuropsychic overload.
However, practice shows that despite all these facts, schizophrenia is often inherited from women. But due to the severity of the symptoms, it seems that men suffer from this psychosis more often. This leads to the formation of a stereotype about the male nature of the disease. But in reality, women get it no less often, it’s just that the first signs appear later - after about 6 years.
In addition, there are other factors that increase the risk of developing schizophrenia. Among them are alcoholism and drug addiction, which are more often observed among the stronger sex. Also, men are less likely to go to doctors, and therefore the pathology progresses for a long time without any medical intervention in this process.
All of these factors increase the risk of developing mental illness. However, this does not mean that it passes specifically from father to son. Although this possibility should not be excluded. It’s just that the mechanism of transmission of the disease still remains unknown.
Modern theories
However, not every medical history is as clear-cut as the one described above. Scientists are still studying the question of how schizophrenia is transmitted and is it inherited? Despite the outstanding achievements and progress in the fields of neuroscience and molecular genetics, the problem of the hereditary factor of schizophrenia has become even more confusing.
Scientists have identified not just one “defective” gene, but a whole complex – 74. Their various combinations and each gene separately, under the influence of many environmental factors, can contribute to the development of the disease. And there are quite a lot of such factors that are provocateurs.
- Unfavorable social and psychological environment in which the child grows up.
- Injuries of various types - traumatic brain, psychological, sexual, physical, received during childbirth.
- Viral diseases that a woman suffered from during pregnancy - flu, colds, herpes, meningitis or encephalitis.
- Drug or alcohol use.
- Nervous stress , emotional and physical fatigue.
One or more of the above factors can trigger the “explosion” of a “genetic bomb”. Scientists believe that the increased activity of “defective” genes disrupts the normal functioning of genes responsible for transmitting signals or impulses between nerve cells. There is a malfunction in the functioning of the brain, which, in turn, leads to the development of mental disorders.
Influence of the female line
The risk of getting schizophrenia through the female line, that is, from the mother, is 5 times higher than from the father. But the transmission mechanism, as in all other situations, is unknown. Scientists have only specific clinical cases. Therefore, it is impossible to say for sure whether a woman with schizophrenia will have children who are schizophrenic or not. Although you still have to exclude other risks in order to reduce the percentage of probability.
There is an assumption that a woman may be a carrier of a chromosomal mutation that will cause the development of schizophrenia in her child. At the same time, she herself may not get sick. This, for example, often happens with color blindness, which is more often detected in men, but the gene for this disease is often transmitted from women.
A provoking factor for the onset of schizophrenia can be an infectious or respiratory disease suffered by the mother during pregnancy. Also during this period toxicosis and alcohol consumption are dangerous. They, in principle, negatively affect the condition of the embryo. It turns out that there is a risk of brain damage, which can subsequently cause schizophrenia.
In this context, it is important to consider the social causes of pathology that are associated with women. We are talking about difficult conditions for the child’s development and the lack of full care for him. But in any case, schizophrenia becomes a consequence of many reasons, which should include biochemical pathologies, organic brain damage, etc.
Genetic predisposition
Genetic studies of schizophrenic disorders began in the 20s of the last century. The search and analysis of genes that are associated with schizophrenia is still ongoing. It is known that the disease is associated with disturbances in the biochemical functioning of the brain. Patients often experience increased dopamine levels and fluctuations in serotonin. Genes associated with the exchange of these mediators in the body are found on chromosomes 1, 6, 8, 13 and 22. Experts are trying to track specific forms of these genes that are most common in people with schizophrenia. Activation of schizophrenic genes can be detected at an early stage of embryonic development. However, the identified genetic changes are not specific to this disease; they can also occur in mental pathologies of other types, and even in normal mental conditions.
There is no single gene, the presence of which can guarantee the development of schizophrenia. Many genes are responsible for the occurrence of the disorder. No one can say for sure that a person who has been found to have “schizophrenic” forms of genes will definitely get sick. There is also no guarantee that the disease will not develop if there are no genetic defects. The likelihood of schizophrenia in each of monozygotic twins is higher than in dizygotic twins, but less than 100%. This means that this disease is transmitted polygenically, through the mother, father or through both parents at once, and is not purely genetic. The development of the disease also depends on the environment. An analysis of the general heritability of schizophrenia revealed that genetics influences 70–90%.
How to influence genes
So, inheritance of the pathology in question is an assumption that is not exactly confirmed by scientific data. Genetic conditioning is considered as one of the provoking factors. To date, there is no identified gene that would definitely lead to this disease. In most cases, we are talking about a set of genes that could hypothetically become the impetus for the development of schizophrenia.
But is the predisposition itself, when there is such a diagnosis in the anamnesis of relatives, a “time bomb”? Should a person whose grandmother, mother or sister suffers/suffered from this illness constantly check their mental health?
Consider the example of alcoholism. Not a single doctor can name its exact reasons either. There is always a group of factors, despite the fact that many researchers claim to have found the gene for this disease. Even if this is the case, it is not possible to influence it.
Moreover, alcoholism is almost 50% caused by the environment. If there is also a genetic predisposition, then this percentage becomes slightly higher. But influencing this, that is, preventing the disease, can only be done by influencing social factors: not visiting places where they drink a lot, leading a healthy lifestyle, coming for consultations with a psychologist, etc.
In almost all cases, there must be a push for the incorrect genes to express themselves. If this provoking factor is not present, perhaps a person, even with a large set of genes that hypothetically cause schizophrenia, will live a quiet life without any hints of psychiatric disorders.
Let us give another example directly related to the disease in question. Let's imagine identical twins whose genes are the same. If one of them develops schizophrenia, the risk of the other developing it is less than 50%. This means that there are other reasons that are not related to heredity.
Time bomb?
And this is where the fun begins. It is impossible to detect the presence of a “wrong” gene using genetic testing. In a specialized consultation, specialists will describe the client’s risks, and by examining the fetus in the expectant mother’s womb, they can indicate the presence or absence of a defect.
However, there are diseases caused by several genes, of which there are from two to ten. Let's look at this situation using the example of rheumatism. Is there any heredity for it? No! The whole point is this: to get sick, it is not enough to be a carrier of rheumatism genes; you also need to catch group A hemolytic streptococcus. That is, this is simply a feature of the immune system, which is easily affected.
What is the situation with schizophrenics if they have a different set of “damaged” genes? This means that for some it is, for example, ABC, for others it is AB, and for others it is only C and the like. There is one thing in common: their functions affect brain development, preventing the process from proceeding normally. And the more such suspicious genes there are, the higher the likelihood of developing a mental disorder. And one more thing: the risk is increased by 16 times by defects in genes on the third chromosome, and by 8 times on the sixteenth.
Despite many years of efforts by geneticists, they cannot create a profile of a schizophrenic. That is, there is no test yet that can answer the question of the possibility of getting sick.
As already mentioned, in order for “bad” genes to manifest themselves, they need some kind of push. If there is none, then the carrier, having them in large quantities, will not get sick. Exactly what external factors these should be is unknown.
Let's take identical twins, who have the same everything, including genes. But one of them has schizophrenia, and the other is completely healthy, and his risk of getting sick is 46%. Why not 100%, you ask? The answer is: some of the patient’s genes were locked by a methyl group, and because of this “lock,” they stopped functioning, and brain development was disrupted.
Where did this group come from? It is unknown, but it has been suggested that the influenza virus is to blame, since the boys’ mother, while pregnant, had it.
According to current data, the risk of schizophrenia in a child due to influenza suffered by the expectant mother increases by 1.5-7 times. However, this is not due specifically to the virus, but to an overly strong immune reaction of the woman’s body, which increased the amount of interleukin-8. But you need to know: not all such cases can provoke the development of mental illness in the offspring.
No predisposition
About 10% of patients with schizophrenia do not have a genetic predisposition. At least, none of the relatives in several generations can detect it. Doctors can study the anamnesis of all relatives that are provided. It is not a fact that signs of a mental disorder will be found, in principle.
This means that people who hypothetically should never get sick, according to proponents of the genetic theory, are also at risk of encountering this pathology. Moreover, 10% of patients, which statistics indicate, is a fairly high figure.
Statistics of the “genetic theory”
To date, psychiatry has accumulated enough information to come to certain conclusions on the question of how schizophrenia is inherited.
The highest rates were recorded in pairs of identical (monozygotic) twins. They have completely identical genes. If one of them gets sick, then the second has a 48% risk of developing pathology.
A case described in works on psychiatry (monograph by D. Rosenthal et al.) attracted much attention from the medical community back in the 70s of the 20th century.
The father of four identical twin girls suffered from mental disorders. The girls developed normally, studied and communicated with peers. One of them did not graduate from the educational institution, but three completed their studies at school successfully. However, at the ages of 20–23 years, schizoid mental disorders began to develop in all sisters. The most severe form - catatonic (with characteristic symptoms in the form of psychomotor disorders) was recorded in a girl who had not completed school. Of course, in such striking cases, psychiatrists simply do not have doubts whether this is a hereditary disease or an acquired one.
A descendant has a 46% chance of getting sick if one of the parents (or mother, or father) is sick in his family, but both grandparents are sick. In this case, a genetic disease in the family has already been virtually confirmed. A person who had both a father and mother with mental illness in the absence of similar diagnoses among their parents would have a similar percentage of risk. Here it is also quite easy to see that the patient’s illness is hereditary and not acquired.
If in a pair of fraternal twins one of them has a pathology, then the risk of the second getting sick will be 15-17%. This difference between identical and fraternal twins is associated with the same genetic makeup in the first case, and a different one in the second.
A person with one patient in the first or second generation of the family has a 13% chance. For example, the likelihood of a disease occurring is transmitted from the mother with a healthy father. Or vice versa - from the father, while the mother is healthy. Option: both parents are healthy, but one of the grandparents is mentally ill.
9%, if your sibling fell victim to a mental illness, but no other similar abnormalities were found in the closest relatives.
From 2 to 6% the risk will be for someone in whose family there is only one case of pathology: one of your parents, a half-brother or sister, an uncle or aunt, one of your nephews, etc.
Other risk factors
People who have a relative with schizophrenia are advised to rule out other risk factors. If you are a carrier of genes that cause schizophrenia, you should play it safe and take all possible measures to prevent pathology. Some of the risk factors were described above in the theories and hypotheses section. Let us list the psychological and social reasons. Among the first:
- Closedness, focus on your inner world.
- Passivity, suspicion, stubbornness.
- Tendency to talk at length.
- Difficulty in formulating thoughts.
- Inadequate emotional reactions.
The last paragraph deals with situations where unimportant events greatly affect a person, and serious tragedies do not cause any emotional response. These symptoms may indicate a person is susceptible to schizophrenia. If the child has them, he should be shown to a psychologist or psychiatrist.
Social factors, which refer to the influence of the environment, include:
- Uncomfortable living conditions - overcrowded city, large number of people in the apartment. All this leads to high levels of stress.
- Social status. If it is low, and a person does not have a good job and income, the likelihood of psychosis increases.
- Negative family relationships. We are talking about conflicts, excessive hostility, suspicions, constant criticism, etc.
The causes of schizophrenia can be listed almost endlessly: alcoholism, drug addiction, sexual or other violence, trauma, etc. In addition, it is worth understanding that this pathology is diverse. It takes a variety of forms - paroxysmal, paranoid, sluggish, etc. Some patients with such diagnoses live normal lives, while others die or become incapacitated.
However, in all cases it is recommended to start treatment as early as possible. To do this, you need to detect the first signs in time. A big role in this is given to relatives, through whose efforts it is often possible to bring a person for the first examination.
The likelihood of developing a disease associated with a chromosomal factor
There is no clear answer to the question of the transmission of schizophrenia from relative to relative.
A genetic disorder or hereditary predisposition are pronounced risk factors, but not a death sentence. Therefore, people who experience this problem should be observed by a psychologist or psychiatrist from early childhood, and should also avoid provoking factors in the development of the disease.
Even when both parents of a child are affected by schizophrenia, the possibility of him developing such a pathology still usually does not exceed a fifty percent probability.
Therefore, until evidence is fully supported by practical and experimental data, one can only speculate about whether schizophrenia is a hereditary disease or not.
Even though there are fairly accurate statistical data that the disease is transmitted along a chromosomal line, it is still very difficult to calculate the degree of its probability.
Many prominent scientists in this field have been engaged in relevant research, but there is no definitive data yet. This is explained by the fact that it is not possible to fully study the mental state and signs of schizophrenia in all relatives of the patient, his absent great-grandparents, or to identify the conditions for the formation and development of a teenager affected by the pathology.
Sometimes the disease can be transmitted from parents to children, but in such a mild form that it can be very difficult to say that a person has schizophrenia.
In cases where parents or children are in a very prosperous environment and do not suffer from any concomitant diseases, sometimes the disease manifests itself in the form of some odd behavior or even almost hidden carriage.
Main symptoms
Symptoms are determined by the type and form of the disease. However, there are a number of signs that are characteristic of almost all varieties of this pathology:
- Openness of thoughts. It seems to a person that all his thoughts are accessible to others.
- Problems with thinking. Often, schizophrenics are prone to lengthy reasoning. At the same time, they constantly get confused, confused and cannot fully formulate what they want to convey to others.
- Rave. The patient feels that his thoughts, actions and feelings are controlled by someone else.
- Hallucinations and pseudohallucinations. The latter differ from the former in that a person does not identify images, voices, sounds and smells with real-life objects and objects.
- Emotional disturbances. As a rule, patients have a tendency to apathy and pathological experiences.
There are also less obvious signs, which are called negative (negative) symptoms, indicating a decrease in mental activity:
- lack of initiative;
- decreased memory and attention;
- fast fatiguability;
- loss of interest in something;
- lethargy or lack of facial expressions;
- isolation and tendency to loneliness;
- inability to enjoy life.
In adults, loss of communication abilities, professional unsuitability and suicidal behavior are observed. In children, you may notice the following signs of the disease:
- Inexplicable fear. The child refuses to go into the room or go to this or that place, screams, resists and throws tantrums for no apparent reason. Often children with this diagnosis tell stories about scary creatures and even show the places where they are located.
- Strange fantasies. During stories about movie or comic book characters, the child becomes so immersed in his role that he cannot get out of it for a long time.
- Decrease in intelligence. He becomes less attentive, does not remember new information well, and his performance at school drops.
- Strange actions. The child constantly looks around, listens, or speaks in a whisper all the time. It is possible that he hears voices and does not understand that they are only in his head.
- Inappropriate emotions. Expresses them disproportionately to the situation. Cries, laughs, is happy or upset when there are no objective reasons for this.
- Manifestations of cruelty. The child becomes more aggressive, communicates less often with peers, and has a tendency to violence against animals or toys.
Some of these signs, in one form or another, can be found in healthy children with poor upbringing. It is important not to ignore them, since schizophrenia, which began early, leads to more severe consequences than the same pathology that occurs in an adult.
Can heredity cause schizophrenia?
Until recently, the mechanism of the disease was unknown, but thanks to the development of neurobiology, it is gradually becoming clearer. It turned out that schizophrenia is preceded by pathogenic factors such as schizoid heredity, unfavorable living conditions in childhood, socio-psychological factors, and disorders in the neurobiological apparatus. It is impossible to state unequivocally that schizophrenia is inherited, that the appearance of the disease depends on whether the father or mother suffered from it. At the same time, it is impossible to categorically state that schizophrenia develops as a consequence of brain injury in each specific case. Today, the neurobiological causes of the disease are being actively studied, but the only correct mechanism for the development of the disease has not yet been identified.
In psychopathology, the word neurosis refers to a family of mental disorders of mental origin, where the subject, unlike psychosis, retains a sense of reality. The meaning of neurosis is very diverse over time and depends on different trends in psychiatry and psychopathology.
Modern psychopathology is consistent with the negative definition of neuroses as a set of behavioral disorders that are not considered to have an organic pathogenesis. Freud, who insisted on the purely psychic origin of hysteria, which he believed was caused by mental ideas that the subject could not accept, based psychoanalysis on the psychogenic concept of neurosis.
Scientists have not been able to fully determine how much heredity influences schizophrenia. Basically, the low reliability of diagnostic results is associated with problems of taking into account genetic factors and the influence of the environment on the patient. As a rule, schizophrenia, even if it is inherited, is in its infancy, as an innate predisposition to the disease. The fact is that schizophrenia, caused by a schizoid mother or father, manifests itself depending on stress factors coming from the environment. The theory that schizophrenia is hereditary, passed on to the child by a mother or father, suggests that a person is simultaneously exposed to genetic, biological, environmental stress and psychological factors.
Although it seems that scientists have not been able to establish a direct connection between the disease and genetics, there is some recorded evidence suggesting an affirmative answer to the hypothesis. Studies have shown that among twins whose mother or father is ill, there is a high degree of predisposition to the disease. This clearly indicates that schizophrenia is inherited. Moreover, as a rule, it is passed on to the children by the mother or other close relatives. Inheritance is quite complex. For an illness to appear, a huge number of factors and pathological processes must come together so that they subsequently develop into schizophrenia.
From the editor: Symptoms, causes and consequences of delirium tremens
Scientists have discovered that not only schizophrenia is passed on to a person from their parents, but also a tendency to other disorders, such as, for example, biopolar. Recent studies conducted after studying the DNA of patients have shown that the mother or father can transmit schizophrenia due to random mutations in certain genes that cause the development of the disease. The mother may also pass on the predisposition during pregnancy. Studies have shown that the embryo often “gets” schizophrenia due to colds and infectious diseases experienced during the prenatal period of its existence. According to medical statistics, schizophrenia is more often diagnosed in children born in spring or winter, when influenza is most common, which, as it seems to scientists, is the cause of disruption of intrauterine development of the fetus.
When it appears
Medical practice shows that with age the risk of developing schizophrenia decreases. According to statistics, the disease manifests itself with the following frequency:
- 10-20 years - 17%.
- 20-30 years old - 39%.
- 30-40 years old - 26%.
- 40-50 years old - 14%.
More precisely, at first the risk becomes higher and higher. This continues until about 30 years of age. Subsequently, the likelihood of getting sick is much less. However, it can manifest itself either a few years after birth or in old age. The risk is less, but it still exists.
What to do
So, schizophrenia can be congenital (hereditary) and acquired. No doctor can give the exact reasons. If you have a genetic predisposition, you should not be afraid of the disease for the rest of your life. However, if possible, other risk factors should be removed.
Schizophrenia cannot be completely cured. But this does not mean that you can ignore it or, on the contrary, despair. In many cases, doctors manage to stop the symptoms of the disease permanently or for many years. The main thing is to start treatment immediately in order to prevent serious damage to the personality or its complete destruction.
Science does not stand still. Perhaps in 10-20 years scientists will find a way to completely rid a person of this dangerous disease. However, reversing the disease is possible only if the unhealthy personality has not supplanted the real one. With a serious schizophrenic defect, a person loses his legal capacity. There is a possibility of death.