All pregnant women carrying a child must undergo routine ultrasound examinations of the fetus in each of the three trimesters. This is a requirement of the Ministry of Health of the Russian Federation. Fetal ultrasound allows you to fully monitor the condition of the woman and child, while the examination is absolutely safe and most informative.
Appointment with a gynecologist - 1000 rubles. Comprehensive pelvic ultrasound - 1000 rubles. Ultrasound during pregnancy - from 1300 rubles. Appointment based on ultrasound or test results - 500 rubles (optional)
CLICK TO MAKE AN APPOINTMENT or ultrasound tests
Timing of planned ultrasound scans during pregnancy and indications for unscheduled examinations
The content of the article
Routine fetal screenings are carried out within the following framework:
- The first screening is from the 10th to the 14th week.
- The second screening is from the 20th to the 24th week.
- The third screening is from the 30th to the 32nd week.
However, most women undergo the procedure more often. The reasons for non-screening ultrasound are the following:
Up to ten weeks:
- The need to confirm the fact of pregnancy and determine the due date.
- There is experience of miscarriage due to miscarriage, habitual miscarriages, missed pregnancies.
- Pregnancy took place through the use of assisted reproductive technology
- There have been negative experiences with fetal pathologies in the past.
- There was a multiple pregnancy in the family.
- Determination of intrauterine or ectopic pregnancy.
After the first ultrasound, you need to undergo an unscheduled examination if you have:
- Nagging pain in the area of the reproductive organs - lower abdomen.
- Presence of bleeding or unusual discharge.
- The size of the uterus is inappropriate for the given period, the belly is too large.
- Suspicion of leaking amniotic fluid.
- The need to control insufficiency (weakness) of the cervix.
You also need to be examined to confirm or refute the conclusions of doctors from previous ultrasound examinations that showed pathologies.
General indications for all three trimesters:
- Bleeding, discharge.
- Stomach ache.
- A uterine size that is not appropriate for the current week is noticed during an examination by a leading gynecologist - then an ultrasound is necessary to exclude an undeveloped pregnancy
3.Diagnostics and treatment
Diagnosis of tumors is carried out using both MRI and CT
, and using special methods -
electromyography and electroneurography
.
This helps assess the condition of the patient's neuromuscular system. In addition, neuro-lumbar puncture
for histological analysis.
surgery is used to remove central neurocytoma.
using transcranial access. However, this is not always possible due to the deep location of the tumor. In this case, radiation therapy is used.
Today, an innovative technique is used to remove a tumor using a cyber-knife - targeted, high-precision irradiation of a tumor with powerful beams of ionizing flux.
. It is envisaged that a high dose of radiation accumulates exclusively in tumor tissues, making them nonviable, but without affecting healthy tissues.
Regarding the diagnosis and treatment of ganglioneuroma
, then there are certain features. A clear diagnostic sign can be an increased concentration of norepinephrine, dopamine and prostaglandins in the urine and blood serum. Treatment of the tumor in most cases is carried out conservatively, or more precisely, by administering a special medicinal solution designed to cause sclerosis of the tumor. If the desired effect is not achieved, it is surgically removed. It should be noted that there are cases of random disappearance of ganglioneuroma without medical intervention.
About our clinic Chistye Prudy metro station Medintercom page!
Objectives of ultrasound throughout pregnancy
The main task of fetal ultrasound
- monitoring the growth, development and well-being of the baby. But each trimester has its own characteristics and clarifying tasks.
In the first trimester, the doctor needs to:
- Determine the location of the fertilized egg. If the pregnancy turns out to be ectopic, urgent surgery will be required, otherwise the organ where the embryo is attached will burst over time. In this case, the woman will at least lose her tube, and there are also deaths.
- Specify the deadline. Knowing the due date will allow you to calculate the due date.
- Find out the exact number of fruits. This is important, since multiple pregnancies often occur with pathologies and end in early birth.
- Analyze extracorporeal circulation and calculate the amniotic fluid index.
- Diagnose non-compliance with the norms of fetal development. During this period, you can refuse a pathological pregnancy and have a medical abortion or vacuum aspiration.
In the second trimester, during a fetal ultrasound, the gynecologist will be able to:
- Examine the woman’s uterus to rule out threats of miscarriage.
- Study the features of the umbilical cord, its loops and the presence of entanglements.
- Inspect the amniotic fluid for its quantity and purity.
- An exploration of the maturity and texture of a child's place.
- Diagnose in detail all the formed organs of the fetus, record the number of heartbeats.
- Determine the sex of the child.
- Carry out fetal fetometry in the context of the current period.
- Determine the position of the fetus.
- Study fetal mobility.
In case of serious developmental disorders, a surgical abortion can be performed during this period. By law, such a procedure is available only if indicated.
The third trimester is considered crucial in terms of the quality of childbirth. Using ultrasound, a gynecologist-obstetrician can:
- Monitor placental blood flow and its effect on fetal development.
- Determine the size of the fetus and its correspondence to the given period.
- Study the location and “age” of the placenta
- Record the location of the fetus relative to the uterine outlet
- Consider the presence and number of entanglements of the fetus with the umbilical cord.
- Identify late-onset pathologies and current diseases of the fetus.
- Determine the condition of the amniotic fluid.
- Study the features of the structure and functioning of internal organs, in particular the brain and heart.
- Specify the due date.
The information obtained from ultrasound during this period is important for determining possible options for delivery. If the fetal position is abnormal, the doctor will prescribe a caesarean section. In case of placental abruption, threat of fetal suffocation, etc., artificial early labor can be performed with stimulation of the process.
Preparation for fetal ultrasound, procedure progress
No special actions are required from the woman to prepare for the ultrasound examination, since all internal organs are displaced by the uterus and do not interfere with the view. But you will have to adhere to several recommendations to make the pregnant woman feel as comfortable as possible.
The doctor will recommend:
- Avoid foods rich in allergens one week before the procedure. Allergies are dangerous not only for the woman - her poor health will certainly affect the behavior of the fetus.
- In a couple of days you need to give up fatty, fried, spicy and salty foods. These products stimulate the secretion of bile and affect the liver - it increases in size.
- For 24 hours, do not consume carbonated water and foods that cause gas formation in the intestines. Air bubbles obstruct vision, distorting echogenicity characteristics.
- Immediately before the ultrasound, control the amount of food and liquid consumed so that the natural urge to empty the intestines and bladder does not constrain the pregnant woman
Failure to follow these recommendations certainly affects the results obtained during the ultrasound, but not so significantly as to refuse diagnosis if you ate a piece of meat or drank a glass of soda the day before.
The procedure is painless. As usual, the woman lies on her back on the couch, and the specialist rubs her stomach, which was lubricated a minute earlier with the gels necessary as conductors. The procedure lasts on average from 10 minutes to half an hour.
Often in the first trimester, a transvaginal ultrasound is performed - a sensor with a condom on it is inserted into the pregnant woman’s vagina. This does not cause pain, the procedure lasts no more than a few minutes. Transvaginal ultrasound may be repeated in the second trimester if a detailed examination of the cervix is necessary.
Causes
Liquor accumulates due to the occurrence of two types of cysts of the transparent septum of the gray matter. Primary neoplasms are detected in almost all children who were premature. In such a child, the defect most often resolves on its own, does not cause any symptoms and is considered benign.
The disease in the fetus develops due to mechanical damage to the abdomen and various infectious pathologies.
Acquired cavities are considered extremely dangerous cysts. Secondary capsules with liquid contents arise as a result of injuries, concussions, inflammatory processes occurring in the brain, and hemorrhages. This type of cystic neoplasm is prone to proliferation, which can even lead to death.
What can a specialist see on an ultrasound?
First trimester
The first planned ultrasound examination is a mandatory part of screening a pregnant woman and, by law, must be carried out no later than the sixth day of the thirteenth week. Globally, it is aimed at excluding pathologies or risk factors for their occurrence. If you suspect any abnormalities after an ultrasound, you may need an additional examination of the amniotic fluid or a chorionic villus biopsy.
In detail, a study in the first trimester provides the following fetometric data:
- The size and weight of the fetus, which confirms or refutes the expected date. Only three values are taken into account: the distance from the head to the coccyx (KTR), between the parietal bones of the head (BPR), and the volume of the fertilized sac (FV).
- Data on the size and structure of the brain - whether its hemispheres are symmetrical, the presence of the necessary structures.
- Information about the work and structure of the fetal heart.
- Development of the digestive, nervous and cardiovascular systems in accordance with the current week of pregnancy.
- Are the fetal limbs normally developed?
- The presence of chromosomal abnormalities such as Down and Edwards syndrome.
Second trimester
The main purpose of ultrasound from the 20th to the 24th week is to examine the size and organs of the fetus to exclude anomalies and developmental deviations, as well as to monitor the condition of the pregnant woman’s organs to avoid premature birth. The data obtained in many cases helps to maintain pregnancy and improve the vital functions of the fetus using medication.
- Location and structure of the children's place. The specialist can see the presentation, low location (in these cases, measures are required) or normal. Compaction of the structure of the placenta (more than 4.5 cm) indicates hydrops fetalis, diabetes or rhesus conflict. Its thickness serves as an indicator of maturity - if it is less than 2 cm, then premature aging is diagnosed, due to which the fetus does not receive the nutrients it needs. If placental abruption occurs, a woman must be hospitalized urgently.
- The amount and purity of amniotic fluid. Their volume is constantly changing and if oligohydramnios is suspected, it is necessary to check this parameter at unscheduled ultrasounds. The reason for the insufficient amount of water may be leakage or lack of kidneys in the fetus. Polyhydramnios is caused by Rh conflict or infection. The latter is evidenced by the presence of flakes in the waters.
- Vessels, loops and entanglements of the umbilical cord.
- Uterine tone, the presence of myomatous nodes, the condition of scars after previous surgery.
- The cervix is measured to exclude isthmic-cervical insufficiency. Its length during this period should be 35 millimeters, at least 33 for the first pregnancy and 22 for repeated ones. The opening of the cervix is also controlled.
Fetometrics of the fetus:
- Dimensions: length of the femur and ulna, ridge, diameter of the head, chest, abdomen,
- weight in grams and height in millimeters. Based on these data, we can conclude that the physical development of the fetus corresponds to the current period.
- The study of facial bones is aimed at excluding Down syndrome pathologies such as cleft lip or cleft palate.
Internal organs of the fetus:
- The head section is examined for double contour, abnormal shapes, and integrity of the cranial bones.
- The brain is assessed by the size of the ventricles and the presence of tumors.
- The lungs are examined for maturity.
- The structure of the heart, blood vessels, and whether the heart rate corresponds to the norms are checked.
- The presence of abnormalities and defects in the kidneys, digestive tract and diaphragm is examined.
Third trimester
Routine ultrasound screening of the last trimester of pregnancy is carried out from the 30th to the 34th week. Its global goal is to determine the readiness of the fetus and the pregnant woman’s body for childbirth. The results of the study are the most voluminous, which is why the procedure lasts about 30 minutes.
Female reproductive organs:
- Uterus - its walls are examined for tone and thickness, the presence of fibroids and the condition of scars in case of previous operations.
- The length, patency, shape and maturity of the cervix are studied, especially in the context of previously diagnosed isthmic-cervical insufficiency. It must be closed, otherwise there is a risk of premature birth.
- Ovarian health is examined.
- Thickness and degree of maturity of the placenta - its walls must be at least 20 mm and no more than 45. During this period, it must mature to the first degree.
- The umbilical cord is examined for attachment to the placenta, the presence of loops and entanglements, and anechoic formations.
- The volume of amniotic fluid should be no more than one and a half liters.
Fetometrics of the fetus and its correspondence to the normal development of this period:
- Child's height and weight.
- Biparietal, fronto-occipital dimensions, head circumference.
- Size of the tibia, femur, humerus, forearm.
- Abdominal girth.
- Maturity of the lungs - during this period it should be the first.
- Nucleus of ossification of the lower part of the thigh (Beclara).
Internal organs of the fetus:
- Cistern, lateral ventricles and cerebellum of the brain.
- Facial bones are examined to exclude cleft lip, cleft palate and other pathologies. The lips, palate, nasal bone, eye sockets, and nasolabial triangle are examined.
- The structure of the spine is examined for hernias.
- The structure of the heart is studied.
- The structure and compliance with the normal sizes of the organs of the digestive and excretory systems are considered.
- The sex of the child determined in the second trimester is confirmed.
Possible fetal diseases:
- Diabetic fetopathy: polyhydramnios, large fetus, enlarged liver size, universal or intense swelling of the subcutaneous tissue.
- Nonimmune hydrops fetalis.
- Hemolytic disease: swelling of the placenta, due to which there is a double contour of the head, back and hip of the fetus, enlarged liver, hydrocele in boys and others.
Discussion
A description of the cavity of the septum pellucidum (SPP) was found in the work of Jacques Dubois (Silvius), dating back to 1671 [12]. The first reliable evidence of the presence of a cavity between the columns of the fornix (“ventriculus fornicus seu cavum Vergae”) was presented by the Italian neurologist and psychiatrist Andrea Verga in 1851. [13]. It is noteworthy that the drug was obtained from the brain that belonged to a patient who died from the effects of hydrocephalus. The first description of surgical treatment of a patient with CPT was given by W. Dandy in 1931 [14].
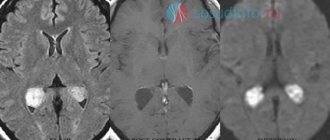
In Fig. Figure 1 schematically shows the anatomy of the areas in which median cysts form. It should be noted that it is customary to distinguish between the concepts of cavities and cysts [16]. Cysts of the RA, PV and PrP are understood as accumulations of fluid more than 10 mm wide with protrusion of the walls towards the lateral ventricles [17–21]. Currently, this is quite clearly recorded by computed tomography (CT) and magnetic resonance imaging (MRI) (Fig. 2) . It has also been shown that the RPP and PV are not part of the ventricular system, lack ependyma, have a different embryogenesis and do not normally communicate with the ventricles [22].
Rice. 1. Schematic representation of areas of potential formation of midline liquor cysts.
a — diagram of the location of formations involved in the formation of median cerebrospinal fluid cysts [12]; b — zones of formation of median cerebrospinal fluid cysts [15]. 1 — columns of the vault; 2 - anterior commissure; 3 - posterior commissure; 4 - end plate; 5-7 - corpus callosum; Cs is the region of the transparent partition, Cv is the region of the Verge cavity, Ci is the region of the cavity of the intermediate sail.
Rice. 2. Differential diagnosis of median cavities and cysts according to magnetic resonance imaging.
Explanations in the text.
Epidemiology. PPP is detected in the fetus up to 8.5 months of gestation in 100% of cases. PPP occurs in 60% of children in the first year of life and in 30% of children aged 1 to 10 years and usually has no clinical symptoms. In adults, PPP persists in 20% of cases, PT in 2%. In 0.04% of cases, cysts form. The presence of large CPP and CPV can be combined with other congenital anomalies of the central nervous system: agenesis of the corpus callosum, hypoplasia of the optic nerves, atrophy of the cerebral cortex, encephalo- and meningomyelocele, etc. [23, 24]. A higher incidence of CPP and CPV has been noted in patients with schizophrenia and other mental illnesses [12, 24, 25], as well as in boxers [26].
Classification. W. vanWagenen et al. identified 3 types of checkpoints [1]:
1) Non-communicating - represent a cavity isolated from other liquor-containing spaces.
2) Communicating, when, due to the rupture of one or more walls of the cyst, its cavity communicates with the lateral ventricles.
3) Secondary, or acquired, when there is an expansion of the RPP communicating with the lateral ventricles due to hydrocephalus (Fig. 3) [27].
Rice. 3. Classification of PPP according to size, determined by magnetic resonance imaging in the coronal projection [27].
The size of the PPP is assessed, followed by gradation from 0 (no visible cavity) to 4 (PPP with narrowing of the lateral ventricles).
Pathological physiology. Numerous histological studies of cyst walls have not revealed the presence of ependymal cells or villous plexus fragments capable of producing cerebrospinal fluid [28]. A possible mechanism for cyst enlargement is extravasation of cerebrospinal fluid from the lateral ventricles [29]. The production of cerebrospinal fluid into the cyst cavity may be carried out by the remains of embryonic cells of the arachnoid mater located in the walls of the cyst, but this assumption has not been confirmed histologically [30]. It has been suggested that cells capable of producing cerebrospinal fluid migrate into the PPP [31], or transform cells forming the walls of the cyst into those capable of producing cerebrospinal fluid [32], which leads to the transformation of the PPP into CPP. In this case, an increase in the size of the cavity occurs, compression of the surrounding nervous structures (limbic system, motor tracts, optic tracts) and veins, spontaneous rupture of the cyst with regression of symptoms, and formation of a “scar” in the wall with the formation of a true cyst [31]. As the size of the cyst increases, impaired venous outflow develops [29]. A risk factor for the transformation of PPP into CPP is “chronic” traumatic brain injury: the frequent presence of CPP has been described in professional boxers [26]. There are also suggestions about the valve mechanism of accumulation of cerebrospinal fluid in the cyst cavity [21, 33].
Clinical manifestations. Most often, the symptoms of CAT form the so-called “CAT syndrome” [34]: a combination of behavioral disturbances, ataxia, speech impairment, seizures and bilateral pathological foot signs. Features of headaches associated with CAT are postural in nature [35], provoked when performing the Valsalva maneuver. Without causing occlusive hydrocephalus and clinical manifestations on their own, CPP and CV can complicate the course of other pathological conditions, for example, cause occlusive hydrocephalus with the growth of intracranial neoplasms [36]. CPP complicates the performance of surgical interventions: endoscopic and bypass operations, installation of external ventricular drainage [37]. A case of the development of Korsakoff syndrome in a patient with CP with regression of symptoms after perforation of the cyst walls is described [38].
Additional research methods. The most informative method for diagnosing medial cavities and cysts is CT cisternography. By the nature of the contrast of the liquor-containing cavities, it is possible to assess in detail the presence or absence of communication between various parts of the ventricles of the brain and these additional cavities and cysts. The presence of a liquor circulation block is the basis for surgical treatment. An alternative method - MRI study of liquor dynamics - is less informative. It allows you to trace the flow of cerebrospinal fluid at the level of the Sylvian aqueduct, in the third ventricle, but does not make it possible to assess the communication of additional cerebrospinal fluid cavities with the ventricular system.
Surgery. Microsurgical cystoventriculostomy, cystoperitoneal shunting and stereotactic puncture and drainage of midline cerebrospinal fluid cysts are currently performed extremely rarely. All of these operations cause injury to the brain substance that is not comparable with clinical manifestations (microsurgical cystoventriculostomy) or are ineffective due to the small size of the stoma formed after the operation (stereotactic puncture and drainage of median cerebrospinal fluid cysts). The search for the optimal treatment method has shown that the best method is endoscopic fenestration of cysts [39]. The use of unilateral and bilateral access, occipital and frontal access, the preferable use of a flexible or rigid endoscope, and the need to install external ventricular drainage remain controversial [40—44] (Fig. 4) .
Rice. 4. Options for endoscopic fenestration of a septum pellucida cyst using neuronavigation [44].
a — entry into the cyst cavity was made at the second stage after ventriculopuncture of the lateral horn (arrows); b — direct puncture of the septum pellucida cyst (large arrow).
Detailed explanation of fetal ultrasound results, norms and pathologies
Since the goals and subjects of medical interest in ultrasound examinations of different trimesters differ, the abbreviations and abbreviations in the reports are different.
First trimester
Estimated date of birth (EDD) - in fact, this is the same as the exact date of pregnancy, only from a different angle. Determined by data on the menstrual cycle and the size of the fetus
- The cervical-neck space (CN) is the main criterion for ultrasound examination in the first trimester. The norm is from 1.5 mm at the 10th week to 2.7 mm at the 13th. If the indicator is increased, the pregnant woman needs to undergo further examination.
- The coccygeal-parietal size (CPR) is one of the main parameters for assessing the size of the fetus. Normally, it should range from 41 mm at week 10 to 73 mm at week 12
- Heart rate - (h/s, heart rate) normally for the first trimester should be 146-179 beats per minute, and this figure is lower the longer the pregnancy period
- Nasal bone – starting from the 12th week should be at least 3 mm, otherwise Down syndrome is suspected
- Biparietal size (BSD) should be from 14 mm at 10 weeks to 26 and higher at 13.
- The yolk sac is studied as an indicator of gestation-appropriate development. It grows in the first weeks and then decreases. Should be round in shape and 4-6 mm in diameter. If the shape is different, and the internal length of the incision is less than 2 mm at 8-12 and more than 6 mm after 10 weeks, a frozen pregnancy is stated.
Pathologies of the septum
Sometimes there are cases of pathological formations of the transparent septum, as well as various types of developmental defects, when a condition occurs that threatens health.
These types of pathologies include:
- septal cavity cyst;
- agenesis of the septum.
As is the case with other diseases of brain tissue, it is necessary to pay close attention to such disorders and be promptly observed by doctors in order to prevent serious complications.
Norms of fetal ultrasound indicators in the first trimester in the summary table
| Term | BPR | Yolk sac | Nasal bone | Heart rate | KTR | VP |
| 10 weeks | 14 mm | 4-6 mm, but not less than 2 | Yes, but not measured during this period | From 161 to 179 beats/min | From 41 mm | 1.5 to 2.2 mm |
| 11 weeks | 17 mm | 4-6 mm, begins to decrease | Yes, but not measured during this period | From 153 to 177 beats/min | 1.6 to 2.4 mm | |
| 12 weeks | Not less than 20 mm | Disappears | Not less than 3 mm | From 150 to 174 beats/min | up to 73 mm | 1.6 to 2.5 mm |
| 13 weeks | Approximately 26mm | Disappears | Not less than 3 mm | From 141 to 171 beats/min | 1.7 to 2.7 mm |
Second trimester
The ultrasound report from the 20th to the 24th week contains the following abbreviations:
- BPR – biparietal size of the fetal head;
- LZR – fronto-occipital size;
- BPR/LZR – cephalic index;
- AB – abdominal circumference;
- RS – heart size;
- DG – tibia length;
- DP – shoulder length;
- DB – thigh length;
- OG – head circumference;
- s/b or heart rate - heartbeat;
- IUGR – intrauterine growth restriction;
- DgRK – chest diameter;
- AFI - amniotic fluid index - an indicator of the amount of amniotic fluid;
- ICI - isthmic-cervical insufficiency - the cervix with this pathology is not long enough for full gestation.
Norms of fetal ultrasound indicators in the second trimester in the summary table
| Term | BPR | LZR | coolant | DP | DG | OG | Heart rate | DgRK | DB |
| 20 weeks | From 43 to 53 mm | From 56 to 68 mm | From 124 to 164 mm | From 26 to 34 mm | From 26 to 34 mm | From 154 to 186 mm | 120-160 beats/min | About 48mm | From 29 to 37 mm |
| 21 weeks | From 46 to 56 mm | From 60 to 72 mm | From 137 to 177 mm | From 29 to 37 mm | From 29 to 37 mm | From 166 to 200 mm | 120-160 beats/min | About 50mm | From 32 to 40 mm |
| 22 weeks | From 48 to 60 mm | From 64 to 76 mm | From 148 to 190 mm | From 31 to 39 mm | From 31 to 39 mm | From 178 to 212 mm | 120-160 beats/min | About 53mm | From 35 to 43 mm |
| 23 weeks | From 52 to 64 mm | From 67 to 81 mm | From 160 to 201 mm | From 34 to 42 mm | From 34 to 42 mm | From 190 to 224 mm | 120-160 beats/min | About 56mm | From 37 to 45 mm |
| 24 weeks | From 56 to 67 mm | From 71 to 85 mm | From 172 to 224 mm | From 36 to 44 mm | From 36 to 44 mm | From 201 to 237 mm | 120-160 beats/min | About 60mm | From 40 to 48 mm |
Third trimester
The last planned ultrasound examination is the most extensive and consists of measuring and studying the following fetal data:
- BPR – biparietal head size;
- LZR – fronto-occipital size;
- OG – head circumference;
- AB – abdominal circumference;
- DG – length of the tibia;
- DB – length of the femur;
- DP – length of the humerus;
- Height – 430 -470 mm;
- Weights – 1400 – 2400 grams;
- Beclair's nuclei - with normal development less than 5 mm;
- Thickness of placenta;
- The maturity of a child's place;
- Placenta placement, its presentation and the presence of abruption;
- AFL - the amount of amniotic fluid - 1-1.5 l is considered the norm;
- The length of the neck is considered normal to be from 30 to 35 mm.
Norms of fetal ultrasound indicators in the third trimester in the summary table
| Duration, weeks | BPR | LZR | OG | coolant | DG | DB | DP | Height | Weight | Placenta thickness | Placenta maturity |
| 30 | From 71 to 85 mm | From 89 to 105 mm | From 265 to 305 mm | From 238 to 290 mm | From 49 to 57 mm | From 52 to 62 mm | From 49 to 57 mm | 270 mm | 1400 g | 13.6 to 28.6 mm | 1st degree |
| 31 | From 73 to 87 mm | From 93 to 109 mm | From 273 to 315 mm | From 247 to 301 mm | From 51 to 59 mm | From 54 to 64 mm | 50 to 60 mm | Up to 390 mm | 1500-1600 g | 17.4 to 29.7 mm | 1st degree |
| 32 | From 75 to 89 mm | From 95 to 113 mm | From 283 to 325 mm | From 258 to 314 mm | From 52 to 60 mm | From 56 to 66 mm | From 52 to 62 mm | Up to 400 mm | Up to 1700 g | From 18.1 to 30.7 mm | 1st degree |
| 33 | From 77 to 91 mm | From 98 to 116 mm | From 289 to 333 mm | From 267 to 325 mm | From 54 to 62 mm | From 58 to 68 mm | From 53 to 63 mm | Up to 430 mm | Up to 1800 g | 18.8 to 31.8 mm | 1st degree |
| 34 | From 79 to 93 mm | From 101 to 119 mm | From 295 to 339 mm | From 276 to 336 mm | From 55 to 63 mm | 60 to 70 mm | From 55 to 65 mm | 430-450 mm | Up to 2400 g | 19.6 to 32.9 mm | 1-2 degree |
Pathologies visible on fetal ultrasound by trimester
In the first trimester, pathologies that arise due to chromosomal abnormalities are detected - frozen pregnancy and lack of embryo growth. In addition to them, signs of Down, Patau, Edwards, Cornelia de Lange, Smith-Opitz syndromes, as well as triploidy and omphalocele are clearly visible.
In the second trimester, in addition to the syndromes of the first trimester, Shershevsky-Turner, Klinefelter, hypertensive-hydrocephalic syndromes, as well as types of polysomy, polyploidy, deformations or absence of internal organs, heart defects, facial bone defects, hypertensive-hydrocephalic, multiple births, poly- or oligohydramnios, umbilical cord pathologies, fetal presentation, intrauterine growth retardation.
In the third trimester, infections of the fetus, defects of the brain, heart muscle, internal organs, intrauterine growth retardation, cleft lip, cleft palate, and fetal presentation may be detected.
The earlier fetal pathologies are detected, the better. If chromosomal abnormalities are diagnosed, the pregnant woman will likely be offered termination of pregnancy in the first and second trimester. Acquired pathologies are most often treated with medication during pregnancy and, if necessary, after the birth of the child.
Experts offer solutions to the problem, and future parents choose them, taking into account all the risks. Each situation is individual and there are no uniform schemes of action. But even if it happened that the pregnancy turned out to be problematic, you need to understand that the level of development of medicine and plastic surgery makes it possible to correct most abnormalities.
Therapy and prognosis of agenesis of the cerebral septum
Conservative treatment is carried out, mainly with anticonvulsants and corticosteroid hormones. Therapy is aimed at eliminating serious and dangerous symptoms that pose a danger to the child. There are no specific means of correcting the absence of a septum.
If agenesis is not complicated by concomitant brain defects, then the child’s development proceeds normally or with minor neurological impairments. However, in cases where there are complications in the form of other malformations of the brain, there may be consequences in the form of mental retardation, decreased learning ability and other serious abnormalities.
Where to get an expert fetal ultrasound in St. Petersburg
You can undergo such an examination only in modern clinics with high-tech equipment. Such a specialized medical center in St. Petersburg is located on Zanevsky Prospekt, 10. The latest device with Doppler, 3D, 4D, etc. functions is installed here. The examination is carried out by doctors of the highest category with extensive experience in maternity hospitals, antenatal clinics and gynecological clinics. The cost of the examination depends on the period and starts from 1000 rubles.
If you find an error, please select a piece of text and press Ctrl+Enter
Clinical manifestations
As the pathological formation increases, the patient suffers from:
- Tinnitus .
- Tremors, numbness of the limbs.
- Blood pressure surges .
- impairment , hearing impairment.
- Sensations of squeezing, squeezing of the head.
- Aching headache that is not relieved by antispasmodics.
The clinical picture that occurs as the disease progresses depends on the location and size of the defect. If the above symptoms appear, you should immediately consult a doctor, since further compression of nearby parts of the brain is fraught with serious consequences.