General information about the disease
Nerve impulses are transmitted from cell to cell along long fibers called axons. They are covered with a myelin sheath, which facilitates and accelerates the movement of the impulse. The development of multiple sclerosis begins when the body begins to produce antibodies against the myelin sheath and gradually destroy it. As a result, the process of transfer of excitation is disrupted. For some time, the nervous system compensates for the disruptions, but as the disease progresses, the severity of symptoms steadily increases.
Symptoms of multiple sclerosis can appear in both men and women. Males get sick somewhat less frequently, but it is in them that the pathology is more severe and less responsive to treatment.
Make an appointment
How does PPMS progress?
The course of PPMS is characterized by a gradual deterioration of a person’s condition, without pronounced periods of stability or improvement. In this case, progression occurs faster: if with relapsing-remitting multiple sclerosis without therapy, on average, 22 years pass before a person loses full ability to move independently, then with primary progressive multiple sclerosis it takes 10 years. Multiple sclerosis begins at a young age. The relapsing-remitting type of course is more often diagnosed in patients aged 20-30 years, and the primary progressive type - at the age of 30-40 years.
Common symptoms of MS
How the disease manifests itself, that is, its symptoms, depends on where exactly the lesion, or focus, appears in the nervous system. Symptoms can be very diverse - these are any dysfunction of the nervous system. Most symptoms can occur in both RRMS and PPMS. For example, these include: - Increased fatigue and sleep problems. One of the most common symptoms and is often the first “alarm bell” that something is wrong with the body. - Vision problems, such as differences in visual acuity between the eyes, black spots, blurred outlines, distorted colors. - Changes in sensation or other symptoms of discomfort in the arms or legs (skin tightness, goosebumps, burning, tingling). - Numbness in the arms, legs, and other parts of the body. - Poor balance, dizziness and other problems with coordination - these disturbances can be so severe that it is impossible to carry out actions purposefully. - Decreased muscle strength (it becomes difficult to lift a leg or arm, clench a fist, sit down and stand up). - Problems with urination - need to go to the toilet more often, or, conversely, less often; incontinence. - Difficulty speaking, articulating and swallowing. — Violations in the sexual sphere. — Depression and other emotional disorders.
Symptoms characteristic of PPMS
Primary progressive multiple sclerosis differs from other types of disease in the constant increase in symptoms. While the main symptoms are the same as those listed above, PPMS can be determined by the following criteria: - The appearance of the first symptoms in adulthood - A more rapid course of the disease and the onset of disability - The absence of periods of improvement, “remissions”. - Symptoms caused by damage to the spinal cord are more pronounced: impaired mobility, weakness, bladder and bowel disorders, sexual difficulties, fatigue. 80% of cases of PPMS begin with gradually increasing stiffness or weakness in both legs. Often the problem does not seem serious, but worsening symptoms should alert you, even if it is just a matter of catching your feet on the steps.
Diagnosis of PPMS – what next?
At this time, multiple sclerosis cannot be completely cured. However, for all types of MS, even for PPMS, there is already therapy available to delay the onset of more severe symptoms. There is a special group of drugs - MS course-modifying drugs (MS drugs). They are so named because they help slow down the progression of the disease, delay the onset of disability, and provide additional time during which a person remains himself, builds a career, family, and makes his dreams come true. The first and so far only PITRS for PPRS in 2021 was registered on the Russian market back in 2021. More information about treatment methods for PPMS can be found in the PPMS treatment .
RU/OCRE/1904/0038
https://scleroman.ru/2016/12/pprs/
https://rskleroz.ru/rs-diagnosis/pervichno-progressiruyushhij-tip.html
https://ru.wikipedia.org/wiki/%D0%9F%D0%B5%D1%80%D0%B2%D0%B8%D1%87%D0%BD%D0%BE-%D0%BF% D1%80%D0%BE%D0%B3%D1%80%D0%B5%D1%81%D1%81%D0%B8%D1%80%D1%83%D1%8E%D1%89%D0% B8%D0%B9_%D1%80%D0%B0%D1%81%D1%81%D0%B5%D1%8F%D0%BD%D0%BD%D1%8B%D0%B9_%D1%81% D0%BA%D0%BB%D0%B5%D1%80%D0%BE%D0%B7
Reasons for appearance
At present, it is not known exactly what exactly triggers the pathological mechanism. Some scientists blame the impact of a specific virus, others put hereditary factors first. Possible causes of multiple sclerosis include:
- brain injuries (concussions, bruises);
- damage to the spinal column;
- chronic mental and/or physical fatigue;
- stress;
- hormonal imbalances (thyroid disorders, diabetes mellitus, as well as changes that occur during pregnancy);
- metabolic disorders, obesity;
- foci of chronic inflammation in the body, etc.
Types and stages
Multiple sclerosis is divided into forms depending on the nature of the disease:
- remitting: exacerbations occur rarely, during the period of remission, brain functions are fully or partially restored;
- primary progressive: the disease begins gradually, the intensity of symptoms slowly increases, and functional recovery does not occur;
- secondary progressive: the patient notes rare exacerbations, between which the symptoms continue to slowly progress;
- progressive-remitting: at first the disease has a similar course to the relapsing-remitting form, but then becomes a stable progressive course.
The severity of symptoms allows us to distinguish the following stages of multiple sclerosis:
- acute: the first two weeks from the sudden onset of symptoms;
- subacute: includes the first two months from the onset of exacerbation;
- Stabilization stage: no exacerbations for 3 months or more.
Variants of the course of multiple sclerosis
The manifestations of multiple sclerosis are different and individual in nature, so the diagnosis of “multiple sclerosis” is announced at first only tentatively. The set of symptoms, the nature of their recurrence, the localization of disorders in the body, as well as the results of laboratory and instrumental studies (in particular, MRI) are taken into account. The subsequent development of multiple sclerosis is quite difficult to predict. Often, only a few years after the appearance of the first symptoms, the doctor is able to accurately diagnose “multiple sclerosis” and predict exactly how the disease will progress in the future.
Depending on the course, multiple sclerosis can be:
- relapsing;
- primary progressive;
- secondary progressive;
- progressive-remitting.
Main symptoms
Signs of multiple sclerosis depend on the location of the main part of the pathological foci. As new areas are affected, the symptoms increase and become more varied.
Damage to cranial nerves
Most often, multiple sclerosis affects the optic nerve, which is responsible for image perception. Often these symptoms are the first signs of the disease:
- a sharp decrease in visual acuity in one of the eyes;
- feeling of a veil, haze, black dots or spots in the field of vision that do not go away after blinking;
- narrowing of the view: blind spots appear in the field of vision (damage to the outer or inner half, as well as narrowing like a pipe - circular);
- a sudden change in the perception of one, several or all colors;
- constant feeling of a speck in the eye;
- blurred outlines of objects;
- pain in the eyeball, worsening with eye movement.
The changes persist for 1-2 weeks, after which they disappear completely or partially. Exacerbations occur periodically.
If the oculomotor and abducens nerves are involved in the process, a person may notice the following symptoms:
- strabismus;
- double vision;
- slight drooping of one of the eyelids;
- disorders of coordinated eye movement.
Less commonly, the disease affects other nerves, in particular the trigeminal or facial. In this case, the patient notes symptoms characteristic of their inflammation.
Cerebellar lesion
The cerebellum is the part of the brain responsible for the sense of balance and coordination of movements. If multiple sclerosis affects this area, a person experiences the following symptoms:
- sudden dizziness or imbalance (including loss of ability to skate, scooter, or bicycle);
- unsteadiness when walking: manifested by a short-term sensation of falling or falling to one side;
- change in handwriting for the worse;
- sensation of objects trembling or appearing double;
- Nystagmus: small vibrations of the eyeballs that are noticeable when looking up or to the sides.
Damage to the cerebellum is often the first sign of a developing disease.
Sensory disorders
Damage to the parts of the brain responsible for sensitivity causes the appearance of paresthesia - sensations that occur without any reason. It could be:
- tingling;
- burning;
- itching;
- feeling of skin tightness;
- crawling of goosebumps;
- decreased sensitivity, etc.
Often only one small area is affected: finger, nose, foot, etc. Typically, such problems pass quickly, and the patient does not take them seriously for a long time until the severity of the symptoms becomes much stronger.
The disease can also manifest itself as a violation of temperature, pain or vibration sensitivity, and both a decrease and an increase in sensations are noted.
Pelvic function disorders
Damage to certain areas of the spinal cord leads to specific disorders that force a person to consult a urologist:
- increased or decreased urination;
- sudden and strong urge to urinate;
- feeling of incomplete emptying of the bladder;
- potency disorders in men, anorgasmia in women.
Movement disorders
Movement disorders occur at any stage of the disease. They are represented by a wide range of symptoms, including:
- problems with fine motor skills (buttoning, sewing, etc.);
- muscle weakness of varying severity;
- decreased reflexes (detected during neurological examination);
- muscle cramps, often occurring at night.
Emotional, mental disorders
This area is not often affected by multiple sclerosis, but as the disease progresses, a person may complain of emotional lability, irritability, memory impairment, apathy, etc.
Multiple sclerosis is characterized by a wide range of pathological foci, which is why signs of the disease are rarely limited to any one area. Often, a person notices several different symptoms at once, which occur simultaneously or replace each other. The doctor’s main task in this case is to tie everything together and prescribe tests that will help confirm or refute the diagnosis.
Diagnostics
A neurologist diagnoses multiple sclerosis. Often the patient comes to him after being examined by a specialist in another field, for example, an ophthalmologist or urologist. The doctor carefully listens to the patient’s complaints, clarifies the time and circumstances of the occurrence of each symptom, and records information about previous and chronic diseases.
A detailed neurological examination can reveal decreased muscle strength, changes in reflexes and sensory disturbances. These data help to suspect the disease. The main examination to confirm the diagnosis is MRI. The procedure allows you to identify characteristic lesions in the brain or spinal cord. The use of special contrast makes it possible to identify even small affected areas.
In parallel, the following may be prescribed:
- spinal puncture with fluid analysis for specific antibodies;
- consultations with narrow specialists, laboratory and instrumental studies to exclude another cause for the appearance of a particular symptom.
BREAKTHROUGH IN MULTIPLE SCLEROSIS THERAPY
At least 150 thousand Russians live with this diagnosis, of which 10-15% are patients with a particularly disabling type of disease - primary progressive multiple sclerosis (PPMS).
Today there are a large number of alternatives for the treatment of relapsing multiple sclerosis, but for the primary progressive type, until recently there was no treatment. In October 2021, the first and so far only drug for the treatment of PPMS was registered in Russia - OCREVUS® (ocrelizumab), produced by .
Multiple sclerosis is a chronic autoimmune disease that damages the myelin sheath of nerve fibers in the brain and spinal cord. Of particular concern is the fact that this disease affects young people aged 20 to 40 years. Up to 90% of patients with this diagnosis suffer from increased fatigue. Vision problems occur in more than 25%, and depression is approximately twice as common. 15 years after the onset of the disease, more than 50% of people experience difficulty walking, and at least 80% report bladder dysfunction.
“We need to take the diagnosis of multiple sclerosis very seriously,” comments Alexey Nikolaevich Boyko , prof., MD, president of the Russian Committee for Researchers of Multiple Sclerosis (ROKIRS). “Unfortunately, very often doctors, especially primary care doctors, make an incorrect diagnosis. It is worth paying attention to the fact that even gradually increasing weakness in the legs can occur with a huge number of diseases - today there are more than 50 of them! Therefore, the big problem now is related to overdiagnosis. Today, Russian patients have the opportunity to delay the progression of disability and realize their plans: build a career, start a family, and have a normal quality of life. Previously, after a diagnosis of PPMS, the doctor could only prescribe symptomatic therapy - slightly reduce muscle tone, improve the general condition and refer for rehabilitation. It is important to understand that there is generally no cure for most chronic diseases. But to ensure that the progression of the process slows down significantly, and for many years the patient can maintain a normal quality of life, is the main goal of therapy.”
In PPMS, the patient's condition steadily worsens, without periods of complete recovery and remissions characteristic of relapsing multiple sclerosis (RRMS). On average, over 10 years, a patient loses the ability to move without outside support, cannot care for himself, and vision and speech are often impaired.
Nenad Pavletich , general director in Russia, notes that in 2008 the disease was included in the state program “Seven Nosologies”, but patients with PPMS did not receive treatment under the program because there were no registered drugs for this type of disease course. OCREVUS® will help significantly slow down the progression of the disease, and therefore improve the quality and life expectancy of people with multiple sclerosis.
Innovative developments in the field of anti-B cell therapy, to which the drug belongs, open up new prospects in changing the course of PPMS. Along with its effectiveness, ocrelizumab has a favorable tolerability and safety profile, which was confirmed in three large phase III studies in a population of patients with RRMS and PPMS, incl. at an early stage. In addition, the drug is also easy to use: it is administered by intravenous infusion of 600 mg every 6 months (the first dose is divided into two intravenous infusions of 300 mg each with an interval of two weeks).
Yan Vladimirovich Vlasov , Prof., Doctor of Medical Sciences, General Director of the All-Russian Public Organization of Disabled Persons with Multiple Sclerosis (OOIBRS), states the fact that a vital drug is not always available to the patient. In matters relating to a number of highly effective and high-cost drugs, the efforts of the medical, patient and scientific community are needed.
“We know our laws and rights,” says Yan Vladimirovich . — Unlike the archaic and mature societies of the West and the USA, our patient organizations are quite young. But youth also presupposes a certain activity, therefore they influence the laws, work closely with the authorities, and they listen to the patient. Our organization was able to ensure that the availability of expensive therapy for patients with multiple sclerosis was maximized. These patients are now receiving treatment free of charge. In addition, we were able to ensure that multiple sclerosis as a nosology was included in the list approved by Federal Law No. 323 Art. 3.
Today a new drug is registered in Russia. But this is just the beginning of the journey. Now we must bring it to the patient by conducting competent registration and information activities. Not long ago, we conducted research in which we found that patients who were diagnosed with multiple sclerosis 5 years ago were already 70% severely disabled. We hope that all patients who are indicated for appropriate innovative therapy will be provided with it as soon as possible. Therefore, our task is to reduce the time between registration and the actual availability of therapy for patients. This is especially critical for people with primary progressive multiple sclerosis, for whom waiting can be costly.”
For reference Based on the results of clinical studies in 2021, the US Food and Drug Administration (FDA) awarded OCREVUS® Breakthrough Therapy status, and in March 2021 approved it in two indications: for the treatment of RMS, and as the first and only drug for the treatment of PPMS. Russia became the ninth country in the world where the drug was registered, earlier than in the EU countries.
Treatment of multiple sclerosis
Treatment requires complex action. The earlier therapy is started, the greater the chance of slowing the progression of the disease and achieving stable remission.
The main purpose of the effect is to change the activity of the immune system and stop the destruction of nerve cell processes. Depending on the form and stage of the disease, the following are used:
- corticosteroids for temporary suppression of immunity (prescribed during exacerbation of the disease);
- immunomodulators for the prevention of exacerbations (used during the attenuation of symptoms);
- plasmapheresis: hardware purification of blood plasma from antibodies;
- interferons to inhibit destruction processes;
- drugs that suppress the immune system (with rapid progression of the pathology).
In parallel, symptomatic therapy is prescribed:
- antispasmodics;
- antidepressants;
- nootropic drugs;
- angioprotectors;
- painkillers, etc.
The selection of drugs depends on the type and severity of symptoms.
Outside of exacerbations, procedures are prescribed to stimulate the functioning of the nervous system and muscles:
- physical therapy and daily exercises for different muscle groups;
- physiotherapy (with the exception of warming procedures);
- psychotherapy;
- massage;
- Spa treatment;
- vitamins (especially vitamin D).
Make an appointment
Possible complications
As multiple sclerosis progresses, neurological damage becomes more severe and pronounced. In severe cases, the patient becomes bedridden, which leads to the development of bedsores and congestive pneumonia. Damage to the brain stem is fatal due to respiratory or circulatory problems. Frequent complications are:
- chronic pain syndrome;
- loss of control over urination and/or bowel movements;
- neuroses and depression, etc.
Multiple sclerosis (MS) is a widespread, chronic demyelinating disease of the central nervous system (CNS), affecting mainly young people, although childhood forms of this disease are also found, as well as its late onset. It is now known that in parallel with autoimmune inflammation in MS, neurodegenerative processes also occur, which begin to prevail over time. This leads to the accumulation of irreversible neurological deficits and, as a consequence, disability of patients.
In 1996, the International Classification of MS was approved, which was based on the types of its course [1]. Relapsing-remitting MS (RRMS) and chronic progressive forms were distinguished - primary progressive MS (PPMS), secondary progressive MS (SPMS), and relapsing-remitting progressive MS. SPMS usually results from transition from MS after 10–15 years of disease progression. But in some patients, immediately after the first clinical episode, there is a slow increase in neurological deficit without episodes of remission, which indicates a possible primary progressive type of disease (PPMS). As was evident from the above, PPMS itself was also divided into PPMS without exacerbations and with exacerbations (remitting-progressive MS).
Epidemiology and genetics of PPMS
The incidence of PPMS, according to various literature data, ranges from 7.9 to 21.7% of the total population of MS patients [2, 3]. At the onset of PPMS, patients are on average 10 years older than patients with RRMS; the average age of onset ranges between 37.3 and 42.7 years [3]. There is also an equal frequency of debuts in women and men and their rarity in childhood.
In 2005, the results of observation of the natural course of MS in 2837 patients conducted in the UK, Colombia and Canada were published [4]. In 12.4% of cases (352 patients), PPMS was diagnosed with an average age of onset of 40 years, with an almost equal ratio of men and women and an average disease duration of 17 years; in 75% of cases, after 7-8 years of the disease, a pronounced neurological deficit with EDSS=6.0 points was noted.
A comparative study of 1844 patients with PPMS and SPMS was conducted by French researchers [5]. During the study, it was revealed that the age of patients at the time of transition from RMS to SPMS is on average 40 years, and the onset of PPMS on average is 40 years. Despite the clinical differences in individual groups of patients, there was a similarity in the rate of disease progression and an increase in neurological deficit mainly due to damage in one functional system.
When studying the genetic aspects of the occurrence of PPMS, it was found that both PPMS and RRMS can occur in identical twins. Immunogenetic studies have shown that the risk of developing one or another type of MS is associated with the major histocompatibility complex class 2, namely the DR2 haplotype DRB1*1501 of the major histocompatibility complex class 2 on chromosome 6 [6–8]. A more detailed study of the genetic markers of PPMS revealed [9] that there is a violation of the expression of the T-cell proliferation gene (IL7R) in patients with PPMS.
Some features of the pathogenesis of PPMS
One review of studies on the natural history of MS [10] revealed that the rate and pattern of progression in PPMS and SPMS are similar, based on which it was suggested that the leading mechanism in the pathogenesis of PPMS may be axonal degeneration leading to neurological deficits. In connection with this, neuromorphological studies began to attract great attention.
A group of researchers led by T. Revesz [11] conducted a histological study of the demyelination focus of a patient with PPMS, during which a significantly lower content of inflammatory cells was revealed in comparison with the demyelination focus of a patient with SPMS. These data, combined with a previous MRI study, showed that PPMS has less focal white matter involvement.
Demyelination lesions in PPMS showed [12, 13] loss of oligodendrocytes and less severe axonal damage than lesions in RRMS [14]. Some researchers [15] drew attention to the fact that in the externally unchanged white matter of patients with both PPMS and SPMS, pronounced demyelination and diffuse changes with activation of microglia and axonal damage are observed, which once again indicates the similarity of the processes occurring in the brain tissue with these types of MS. Signs of demyelination were also noted in the cortical gray matter, although more significant changes were seen in the white matter, especially in MS patients, with a clear delineation of affected and unaffected areas.
Summarizing the above, there are clear differences between RRMS and PPMS: with PPMS, more pronounced pathological changes are noted in the form of diffuse axonal damage in the white matter and cortical demyelination, in contrast to RRMS, we are talking about local tissue damage in the focus of demyelination.
There is now sufficient convincing evidence to support the assumption that axonal loss underlies the irreversible and progressive nature of disability in MS. in vivo biomarkers of axonal injury.
.
The most widely used marker of axonal degeneration is the detection of increased concentrations of amyloid protein in axons in areas of demyelination. Another immunohistochemical marker of axonal damage is SMI32, an antibody that labels nonphosphorylated axonal neurofilaments. Normally, maturation of the axonal cytoskeleton is usually accompanied by an increase in phosphorylated neurofilaments. This process is induced by glial cells during myelination and leads to an increase in axon diameter. During the process of demyelination, axonal neurofilaments are dephosphorylated, resulting in structural changes within the axon itself. Other changes in the axon cytoskeleton are also noted - phosphorylation and release of the Tau protein, which is the main protein of axonal microtubules. It is the increase in the concentration of this protein that is detected in the cerebrospinal fluid of patients at the onset of the disease, both with RMS and with progressive forms [16]. All this indicates that the axon cytoskeleton is very vulnerable, and functional disorders over time, with chronic exposure to destructive factors, turn into structural lesions with disruption of synaptic transmission of nerve impulses.
To the above, we can add that in RRMS and PPMS, antibodies to myelin were detected in the serum and cerebrospinal fluid. This became the basis for the statement [17] that PPMS is a disease with antibody-mediated pathogenesis mechanisms.
To objectify atrophic processes in the central nervous system as a manifestation of neurodegeneration, MRI is currently widely used. Atrophic processes in patients with PPMS and SPMS using MRI are detected both in the brain and in the spinal cord already at the initial stages of the disease, and a connection between atrophic processes and the increase in disability of patients has been established.
The use of another new method, MR spectroscopy, and analysis of changes in the content of N-acetylaspartate (NAA) made it possible to detect neuronal loss in MS even in the apparently unchanged white and gray matter of the brain. One possible explanation for neuronal loss may be secondary Wallerian degeneration as a consequence of focal axonal damage.
The data obtained from studying the blood-brain barrier (BBB) in MS patients deserve special attention. In 2007, the results of a study of the state of the BBB in patients with PPMS and SPMS were published [18]. Signs of BBB failure were identified not only in active lesions, but also in chronic inactive lesions, as well as in externally unchanged white and cortical gray matter of the brain in both PPMS and SPMS.
MRI criteria for diagnosing PPMS
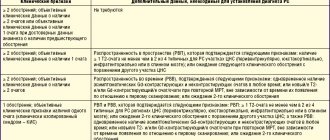
In all diagnostic systems, PPMS is identified as a separate form of MS. Due to the fact that there was previously no evidence that the neuroimaging characteristics of patients with relapsing-remitting forms of MS are significantly different from those of patients with PPMS, the MAGNIMS expert group concluded that the use of uniform criteria will significantly facilitate the diagnostic evaluation of patients with PPMS [19]. In 2009, MRI criteria characterizing the dissemination of the pathological process in space and time were proposed for the diagnosis of both PPMS and RRMS and were more clearly stated in the form of modified McDonald criteria (2010) [20, 21]. According to these criteria, dissemination of the pathological process in space in PPMS is determined by the presence of 2 of the following 3 criteria: the presence of one lesion or more in the brain in T2 modes, in at least one of the three localizations typical for MS (periventricular, subcortical, subtentorial); the presence of two or more foci in T2 modes in the spinal cord; positive examination of the cerebrospinal fluid for oligoclonal IgG antibodies.
The sensitivity of using the spinal cord criteria and testing the cerebrospinal fluid for oligoclonal IgG antibodies was analyzed retrospectively in a cohort of 95 patients with PPMS [22]. As a result of this study, the criterion for dissemination of the pathological process in space for the spinal cord was changed from 2 foci or more to 1 foci or more (it does not matter whether these foci are clinically significant or not), which significantly simplified this criterion and increased its sensitivity ( see table, see figure). But despite this, a more detailed verification of its specificity is required.
MAGNIMS (2016) MRI criteria for PPMS
MRI of the brain and cervical spinal cord of a patient with PPMS in PD (a, c) and T2 (b, d) modes. In the periventricular white matter of both hemispheres of the cerebrum, as well as in the spinal cord at the level of the C6 vertebra, foci of demyelination are detected (indicated by arrows).
As a result, the MAGNIMS expert group came to the conclusion [19] that the criterion of dissemination of the pathological process in space should be used for both RMS and PPMS, with an additional study of the cerebrospinal fluid for oligoclonal IgG antibodies in doubtful cases.
Main clinical features, course and prognosis
One of the main differences between PPMS and RRMS (besides the age of the patient at the onset of the disease) is the period during which the corresponding symptoms develop and the nature of their development. With RMS, relapses of the disease are observed, occurring quite rapidly (from several hours to several days), with signs of increasing neurological deficit and alternating with periods of remission. In PPMS, functional impairment initially develops slowly over several months and sometimes years, and is rarely characterized by any fluctuations.
A number of studies have shown that the most common symptoms at the onset of PPMS are caused directly by damage to the spinal cord and are manifested by motor disorders [23]. The frequency of onsets with signs of spinal cord damage in PPMS averages 38.9–88.7%. Involvement of other functional systems, for example, sensory disorders, constitutes an average of 15-32.5% of cases; signs of involvement of the brainstem or cerebellar structures are even less - 10.8-16% of cases. But the most obvious difference between the onset of RRMS and PPMS is the frequency of involvement of the optic nerves (in PPMS, less than 5% of cases) [24].
Previous studies of the natural history of MS clearly demonstrate that progressive forms of MS have a less favorable prognosis compared to RRMS. However, cases of fairly long periods of stabilization have also been described in PPMS. To date, for PPMS, as for MS in general, there are 2 main negative prognostic factors: the rate at which the patient reaches an EDSS score of 3.0 from the onset of the disease and the involvement of 3 or more functional systems at the onset of the disease [25].
Problems in treating patients with PPMS
Since the late 90s of the last century, drugs have been used quite actively and successfully to modify the course of MS, making it possible to reduce the activity of the disease both clinically and according to MRI data, which, of course, leads to a slowdown in the progression of disability in patients. A clear division into the types of course of MS helps to determine the prognosis of the disease already at the stage of diagnosis, as well as to choose the most correct tactics for managing the patient, since drugs that change the course of MS are effective mainly in relapsing-remitting course. As for PPMS, for example, in 2000, data were published regarding the ineffectiveness of therapy obtained during a clinical trial of the use of the drug interferon beta-1a (at a dosage of 30 and 60 μg intramuscularly) in patients with PPMS in comparison with placebo [26 ]. Later, in 2009, a group of authors [27] published similar information regarding interferon beta-1b. Attempts have been made to use the drug glatiramer acetate in patients with PPMS: no significant differences with the placebo group were found in any of the efficacy criteria [28]. Subsequently, hopes were placed on the drug fingolimod, due to the fact that a slowdown of atrophic processes in the central nervous system was recorded when used in patients with RRMS. However, the INFORMS study [29] noted the lack of therapeutic effect of this drug in the treatment of patients with PPMS.
One of the modern and very successful trends in the treatment of patients with MS is currently the use of monoclonal antibody drugs. This concerns primarily the drug rituximab (a chimeric anti-CD20 monoclonal antibody). An attempt to use it in patients with PPMS was made as part of the OLYMPUS clinical trial [30]. It was found that in younger patients, with a shorter duration of the disease and the presence of active lesions according to MRI at the beginning of therapy, positive dynamics were observed in the form of a decrease in the severity of inflammatory reactions (it is assumed that this may be associated with B-cell depletion).
In September 2015, encouraging data were published regarding another monoclonal antibody, the drug ocrelizumab (a humanized anti-CD20 monoclonal antibody) [31]. In the ORATORIO study, ocrelizumab showed its good tolerability and high efficacy in the form of a significant reduction in the risk of progression of disability compared to placebo.
The results obtained regarding the effectiveness of monoclonal antibodies give hope to a fairly large group of patients with PPMS for changing a previously negative prognosis to a relatively positive one. But, despite the positive trends in the pathogenetic therapy of MS, it remains obvious to everyone that, as with RRMS, treatment of patients with PPMS should begin in the early stages of disease development.
There is no conflict of interest.
Prevention
Prevention of multiple sclerosis is, first of all, general measures that are relevant for every person:
- good sleep;
- minimizing stress and fatigue;
- complete and proper nutrition;
- normalization of body weight;
- elimination of bad habits (smoking, drinking alcohol);
- regular walks in the fresh air and amateur sports.
To prevent relapses, patients who have already been diagnosed should refrain from overheating (visiting baths, saunas, hot baths) and insolation (prolonged exposure to the open sun and visiting a solarium).
When the first signs of trouble appear, even if they occur rarely and only for a short time, it is important to undergo examination by a specialist.
Relapsing (remitting) multiple sclerosis
With relapsing-remitting multiple sclerosis, unpredictable pre-acute attacks (relapses) are observed, against the background of which the symptoms of the disease worsen. After this, complete or partial restoration of the functions of the affected organs may occur, in some cases the functions are not restored. The next relapse may develop in a few days or weeks. Sometimes recovery from an attack may take longer - up to several months. In the intervals between attacks, the patient’s condition does not deteriorate. This pattern of the disease is typical for most patients in the initial stages of multiple sclerosis.
Relapsing-remitting multiple sclerosis is diagnosed in most patients at the onset of the disease. In 85% of patients, periodic exacerbations (relapses, exacerbations) are observed, during which new or existing objective symptoms of lesions of the central nervous system appear or intensify.
Neurological symptoms worsen during the day, but body temperature does not increase. The interval between the previous confirmed episode of exacerbation and the new one is called remission and is at least 30 days. During this period of time, symptoms completely regress or remain partially, causing progression of disability. During the remission period, objective neurological symptoms do not increase; changes in the patient’s well-being and neurological status are noted throughout the day. These changes are unstable in nature, their origin depends on a number of endogenous and exogenous factors.
Treatment at the Energy of Health clinic
Neurologists at the Energy of Health clinic offer comprehensive treatment for multiple sclerosis, aimed at eliminating symptoms, preventing relapses and stopping the progression of the disease. We use:
- the most effective drug treatment regimens used in leading clinics around the world;
- physiotherapy in accordance with indications and contraindications;
- physical therapy classes in the clinic and the preparation of a gymnastic complex for home warm-ups;
- restorative and therapeutic massage;
- help from a psychotherapist;
- organization of sanatorium-resort treatment.
Advantages of the clinic
Multidisciplinary medical is a full range of services for the treatment and prevention of various diseases. We offer our clients:
- modern diagnostic methods using high-precision equipment and effective techniques;
- selection of treatment in accordance with the individual characteristics of the body;
- a competent combination of medications, physiotherapy, massage and other non-drug techniques;
- minor surgical operations within the walls of the clinic;
- own day hospital with comfortable wards.
The extensive experience of our specialists allows us to achieve success even in the most difficult cases, and reasonable prices make high-quality medical services accessible to everyone.
Multiple sclerosis cannot be completely cured, but it can be successfully controlled. Remember, even minor neurological disorders may indicate the development of a serious disease. Sign up for diagnostics at Health Energy.
Types of PC
Each of them has its own course, symptoms and is treated according to its own scheme. If you are not yet sure what multiple sclerosis is, you can find out about it in this article .
Clinically isolated symptom (CIS)
CIS is understood as a situation where a person has some signs of damage to the central nervous system, but it is immediately impossible to unequivocally attribute them to the diagnosis of “multiple sclerosis.” In some cases, after a diagnosis of CIS, multiple sclerosis may develop some time later.
Relapsing-remitting (RRMS)
The most common type of multiple sclerosis. It is characterized by periodic exacerbations, followed by periods of complete or partial improvement (remission), and there is a partial or complete restoration of impaired body functions. It is important that with this type of MS, there is no gradual, smooth increase in symptoms between exacerbations.
Primary progressive (PPMS)
In this case, the disease develops evenly, symptoms steadily increase without periods of exacerbation and remission. This diagnosis is made in 10–15% of patients with multiple sclerosis. The rate and type of progression are quite unpredictable and vary from patient to patient. But during the course of the disease, periods of activity can still be observed (they can be noted, for example, by new, active plaques identified by MRI) and periods of inactivity. Most often, you can also notice periods of faster progression and slower progression, stabilization.
Secondary progressive (SPMS)
The relapsing-remitting course of the disease most often gives way over time to a secondary progressive course - this means that between exacerbations there is already some constant progression of symptoms. Over time, exacerbations appear less and less often, become less pronounced (or do not appear at all), but disability increases, recovery after relapses is not complete, and the disease continues to develop steadily. It is impossible to immediately determine what type of course each individual person will have - as in the case of symptoms, each person is unique. This can only be understood through constant observation by a doctor and with the help of modern diagnostic methods.
RU/OCRE/1904/0038
https://ru.wikipedia.org/wiki/%D0%A0%D0%B0%D1%81%D1%81%D0%B5%D1%8F%D0%BD%D0%BD%D1%8B%D0 %B9_%D1%81%D0%BA%D0%BB%D0%B5%D1%80%D0%BE%D0%B7
https://www.nationalmssociety.org/What-is-MS/Types-of-MS
https://www.kp.ru/guide/rassejannyi-skleroz.html