Multiple sclerosis significantly affects the state of the human visual system. A patient with this diagnosis often has damage to the optic nerve, called retrobulbar neuritis. What are the features of this ophthalmic pathology, how does it affect vision and what treatment methods does modern medicine offer, read in our article.
In this article
- Multiple sclerosis: what is this disease?
- What symptoms may indicate MS?
- How does an autoimmune disease affect our visual system?
- Why does vision suffer in MS?
- Retrobulbar optic neuritis as a symptom of MS
- Specificity of retrobulbar neuritis in multiple sclerosis
- How is retrobulbar neuritis diagnosed?
- Is it possible to cure optic neuritis in multiple sclerosis?
- The main directions of therapy for descending neuritis
- Treatment of retrobulbar optic neuritis in MS
- Are there preventive measures?
- When will a cure for multiple sclerosis be invented?
Multiple sclerosis: what is this disease?
Multiple sclerosis (MS) is an autoimmune chronic pathology accompanied by damage to the upper layer of nerve fibers in the brain (brain and spinal cord).
Human nerves are covered by the so-called myelin sheath, whose task is to protect thin fibers from negative influences. When the structure of this surface layer is destroyed, plaques—defective areas—are formed. As a result, the signal transmitted from the brain centers to the organs reaches poorly or does not reach at all, which leads to disruption of many body functions, including visual.
The concept of “autoimmune pathology,” which is often used to describe multiple sclerosis, means that abnormalities in the functioning of the body’s own immune system lead to the development of the pathological process. Simply put, the immune system mistakes its own cells for foreign ones and begins to destroy them. Some cells are replaced by others, resulting in the formation of scar connective tissue in place of the nerve fibers.
Many people mistakenly associate the term “multiple sclerosis” with memory problems in older people. In fact, the disease we are talking about involves a different type of disorder and often develops at a young age. Most often, the disease is detected in patients in the age range of 15-40 years, although there are cases where multiple sclerosis was found in two-year-old children.
Statistics show that the incidence rate of multiple sclerosis is approximately 25 cases for every 100 thousand people. And this is the second most common cause that leads to neurological disability at a young or young age.
Why does multiple sclerosis occur and is there an effective treatment?
Multiple sclerosis (MS) is a chronic (ongoing) and complex disease in which your body's immune system mistakenly attacks itself. This is called an autoimmune response.
In MS, the immune system attacks and damages the fatty material (myelin) that insulates the nerves of the central nervous system (brain, spinal, and optic nerves). This is called demyelination. Healthy myelin acts like the coating on an electrical cord. It protects nerve fibers and allows them to transmit impulses (messages) quickly and efficiently.
Demyelination causes inflammation and scarring (multiple sclerosis means “many scars”). The formation of these scars, known as plaques or lesions, affects the ability of nerves to transmit messages between the brain and other parts of the body.
Symptoms of the disease
The symptoms of multiple sclerosis are varied and unpredictable, depending on which part of the central nervous system is affected and to what extent. No two cases of multiple sclerosis are alike.
Symptoms can vary from day to day, and symptoms can also interact with each other. Symptoms of multiple sclerosis can be both visible and invisible to others.
Some of the most common symptoms of multiple sclerosis include:
- Motor control. Difficulty walking, balance or coordination, muscle spasms or tremors, muscle weakness, slurred or slow speech, difficulty swallowing, dizziness or dizziness.
- Fatigue. Extreme fatigue, often combined with increased sensitivity to heat, which can affect your physical, emotional and mental abilities.
- Sensory problems. Visual disturbances (eg, blurred or double vision or changes in depth perception, partial or complete loss of vision), altered sensations such as paresthesia, numbness, neurological pain, sensitivity to heat, cold, or discomfort.
- Bladder and bowel dysfunction, including urinary incontinence (leakage from the bladder or bowel), the need to urinate more or less frequently, urge to urinate, frequent urge to urinate at night, constipation or diarrhea.
- Cognitive symptoms, including brain fog, impaired memory and concentration, changes in processing speed and ability, and impaired cognitive function.
- Personality and emotional changes, anxiety, depression and difficulty sleeping.
MS is a chronic disease that requires constant adjustment, treatment, monitoring and sustainability. Likewise, it affects others differently at different times.
Features of treatment
There are no medications to treat multiple sclerosis; they are used to modify the course of the disease. The therapy currently used is used to:
- minimize relapses;
- reduce inflammation;
- prevent the formation of new damage;
- minimize brain atrophy;
- restore lost functions;
- Minimize the impact of symptoms on your daily life.
There are several things a patient can do on their own to keep their brain as healthy as possible:
- keep your weight under control;
- maintain a healthy diet;
- stop smoking;
- limit alcohol consumption;
- maintain a sufficient level of physical activity;
- Learn some ways to manage stress.
Multiple sclerosis can be stressful because it is unpredictable, but stress can in turn increase the risk of relapse. Therefore, the last point is extremely relevant to reduce the rate of disease progression.
Forecast
The progression of MS and a person's prognosis cannot be predicted in the early stages with great accuracy. People with early stages of multiple sclerosis are advised to try to lead a normal lifestyle, exercise frequently and eat a healthy diet. However, any specific diet for multiple sclerosis has not been shown to negatively affect the course of the disease. If you have multiple sclerosis, monitor the symptoms that occur during exercise to adapt to them and learn to reduce your effort level accordingly.
Although there is no cure for multiple sclerosis yet, researchers are making promising progress and discoveries in treatment and management every day.
What symptoms may indicate MS?
Symptoms can vary markedly from person to person with multiple sclerosis. Moreover, at different stages of the pathological process they can be different in the same person. This is explained by the fact that the symptoms directly depend on which areas of the brain and central nervous system are affected by abnormal changes.
Most of the symptoms that occur with multiple sclerosis can be attributed to neurological and ophthalmological symptoms.
- The patient has serious visual impairment (usually unilateral).
- Pain may occur when moving the eye.
- The sensitivity of tissues changes - a person may feel tingling, itching, numbness.
- Constant feeling of tiredness, fatigue.
- Changes in muscle tone.
- Poor coordination, loss of balance, unsteadiness when walking.
- Disturbances in the genitourinary system - urinary incontinence, decreased libido, erectile dysfunction.
- Emotional lability, neuroses.
Any of these symptoms, and especially their combination, is a good reason to consult a specialist.
Multiple sclerosis (MS) is a disease with multifocal damage to the central nervous system (CNS). As is known, the classic manifestations of MS are signs of damage to the pyramidal, sensory and cerebellar systems, involvement of the cranial nerves and also pelvic disorders [1-3]. These clinical symptoms occur in various combinations, reflecting the localization of demyelination foci in the brain and spinal cord. Nevertheless, there are “typical” and “atypical” symptoms for MS [3]. If typical symptoms help a clinician diagnose MS, then atypical ones force them to look for other causes of their occurrence, and MS becomes a diagnosis of “exception”. One of the “atypical” manifestations of MS is extrapyramidal movement disorders. In the literature there are rare descriptions of spastic torticollis [4, 5], chorea, dystonia [6], and tremulous hyperkinesis in MS [7]. A few articles are devoted to myoclonus [8-12]. In our clinical practice, we encountered such an unusual manifestation of MS as spinal myoclonus. Because this is a very unusual manifestation of MS, it may be of interest to specialists.
Patient A.
, 33 years old, works as an engineer, left-handed. From the life history: the patient’s heredity is not burdened. At the age of 10, he noted the development of weakness and a feeling of numbness in the left extremities, for which he was hospitalized in the neurological department of a children's hospital with a diagnosis of “Acute cerebrospinal circulatory disorder.” As a result of the treatment, the symptoms completely regressed within six months, after which nothing bothered the patient.
About 3 years ago, at the age of 30, the patient noticed periodic “twitching” in the left hand, forearm and shoulder. Such twitchings were observed 2-3 times a week, with purposeful movements, were spontaneous and became more frequent with excitement. The patient was unable to restrain or reduce these violent movements by any means or effort of will. Bright lights and loud sounds also had no effect on the twitching. Since the severity of violent movements, according to the patient, was not significant, he did not seek medical help. Over time, twitching in the left hand began to occur more often, sometimes regardless of active movements; they already bothered the patient at rest and persisted during sleep. The increase in the amplitude of violent movements forced the patient to leave work and seek medical help. Twitching increased during emotional stress and decreased after drinking alcohol. Other external factors did not influence them. The patients had no attacks with loss of consciousness.
When examining the patient's somatic status, no pathology was found. During a neurological examination, a slight disturbance of the associated movements of the eyeballs without double vision and nystagmus was recorded, and a slight smoothing of the right nasolabial fold was observed. Hyperesthesia of the feet on both sides from the level of the ankle joints, hypoesthesia of the left little finger of the hand and the lower third of the inner surface of the left forearm were detected, and the patient did not make active complaints about changes in sensitivity. Vibration and muscle-joint sensation was intact, muscle strength was sufficient. Tendon reflexes from the upper extremities were normal, with a vague predominance on the left; the knee and Achilles reflexes were brisk. Plantar reflexes were of the flexion type; abdominal reflexes were absent. The patient performed the finger-nose test on the left with kinetic tremor, without an intention component. Tandem walking was not impaired. Dysdiadochokinesis, Babinski asynergia and pelvic disorders were not detected.
Violent movements were recorded in the shoulder girdle on the left and left arm - jerky twitching in the form of a sharp alternating contraction of the muscles of the shoulder, forearm, wrist extensors and finger flexors, which led to the periodic occurrence of either moderate (20-25°) extension in the shoulder, or flexion in the elbow (10-15°), then to simultaneous extension in the wrist joints and flexion of the fingers. Hyperkinesis manifested itself especially clearly when stretching the arms forward and holding them in this position, with a frequency of up to 10 per minute. At rest, rare hyperkinesis of the above-described nature, but of significantly lower amplitude, was detected. Hyperkinesis prevented the patient from making precise movements; he was unable to write his last name. Sharp noise (clapping hands), tapping (on muscles, tendons) and light did not cause an increase in myoclonus.
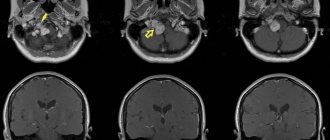
Laboratory tests of blood and urine were normal. According to the results of magnetic resonance imaging (MRI) of the brain and spinal cord, multiple foci of demyelination measuring 3-7 mm, hyperintense on T2-weighted images (T2-WI) and hypointense on T1-weighted images (T1-WI), localized in white matter of the cerebral hemispheres, periventricular and subcortical regions, corpus callosum. A similar single lesion was observed in the right hemisphere of the cerebellum (Fig. 1)
.
Figure 1. MRI of the brain.
Multiple foci of demyelination, hyperintense on T2-weighted images. a - localized in the white matter of the cerebral hemispheres, periventricular and subcortical regions; b - a similar single focus is recorded in the right hemisphere of the cerebellum; c — lesions periventricular and in the corpus callosum; d — MRI after 3 months, compared with previous results, the appearance of new foci of demyelination was revealed; the focus at the posterior horn of the right lateral ventricle accumulates contrast agent. At the level of the C2 segment, 2 intramedullary lesions without clear contours were identified, slightly hyperintense on T2-weighted images and isointense on T1-weighted images, measuring 4x6 and 4x7 mm. The presence of a similar lesion at the level of segments C4-C5 and C5-C6 of the cervical spinal cord could not be excluded (Fig. 2)
.
Figure 2. MRI of the spinal cord.
At the level of the C2 segment, 2 intramedullary lesions are identified without clear contours, slightly hyperintense on T2-weighted images; the presence of similar lesions at the level of segments C4-C5 and C5-C6 of the cervical spinal cord cannot be excluded (indicated by arrows). Electroencephalography revealed no pathology. During involuntary contractions of the muscles of the left arm, no pathological changes were recorded on the EEG. Needle electromyogram (EMG) revealed discharges from several motor units of the m. extensor dig. com.
on the left (segment C7), discharge duration 70 ms and amplitude 1400 μV.
When conducting research in other muscles innervated by other segments, no answers were obtained (Fig. 3)
.
Figure 3. Needle EMG. Discharge with m.
extensor dig. com. lasting 70 ms and amplitude 1400 μV (responses were not obtained in other muscles from other segments). Stimulation EMG revealed a disturbance in the conduction of the motor fibers of the left arm at the elbow level (tunnel syndrome); no changes were found in the nerves of the left arm.
Thus, the patient was examined during an episode of deterioration in neurological status. This episode occurred in a young man (33 years old) with no previous or concomitant infection/fever. The detection of 2 or more signs of multifocal damage to the central nervous system during examination and the identification of lesions typical for MS on neuroimaging (subcortical, periventricular, infratentorial and in the spinal cord) [13] allowed us to settle on the diagnosis of “probable multiple sclerosis”. An episode that occurred in childhood (weakness and numbness on the left side) may have been the first attack of MS (although it is not documented). If this is so, then we are dealing with the onset of MS in childhood. The patient received standard pulse therapy with glucocorticosteroids and on the 3rd day of treatment noted a decrease in the frequency of twitching. Objectively, myoclonic hyperkinesis was recorded in the left hand, which was more postural in nature and appeared with a frequency of 8-10 per minute; twitching was not detected at rest. After 1 month, myoclonus stopped completely.
To verify the dissemination of the pathological process over time and establish a reliable diagnosis of MS, the patient underwent a repeat MRI examination of the brain after 3 months. Compared with previous MRI results, new foci of demyelination were noted on the left in the periventricular region and at the posterior horn of the right lateral ventricle; when contrast was administered, the last lesion accumulated contrast agent (omniscan) (see Fig. 1)
. According to the McDonald criteria [13], the patient was diagnosed with relapsing-remitting MS. After 3 months, no hyperkinesis was detected in the hand.
Considering the presented observation, it should be noted once again that spinal myoclonus (SM) is a rather rare form of hyperkinesis. They can be divided into segmental and propriospinal [14-19]. This division is based on the segmental structure of the spinal cord and the connections of the segments through the propriospinal tract. Spinal segmental myoclonus (SSM) is an involuntary movement involving hyperkinesis of muscles innervated by one or more adjacent segments of the spinal cord [17, 20–22].
In the above observation, myoclonus was localized in one arm. If we analyze the entire kinetics of the existing hyperkinesis, then the movements that constituted the hyperkinesis, namely shoulder extension (m. deltoideus, m. supraspinatus)
;
flexion at the elbow joint ( m. biceps brachii, m. brachialis, m. brachiradialis
);
extension of the hand ( m. extensor carpi radialis longus, m. extensor carpi radialis brevis, m. extensor dig. com.
);
flexion of the fingers ( m. flexor digitorum superficialis
) was provided by muscles innervated by several adjacent segments C5-C7 [23]. Accordingly, the patient had SSM.
In most cases, SSM are symptomatic, and they are based on lesions in the spinal cord caused by some primary disease - infection [24-26], tumor [27], arteriovenous malformation [28], syringomyelia [16], acute disseminated encephalomyelitis [29], vertebral pathology [28], iatrogenesis [125], etc. [10, 30-35]. Let us recall that the observed patient had foci of demyelination at the level of segments C2, C4, C5, C6 of the cervical spinal cord, and it was these foci that could cause the occurrence of myoclonic twitching of a segmental nature (see Fig. 2)
.
Clinically, SMS are most often irregular or can be rhythmic with a frequency of 0.2-8 Hz and an intensity of 1-600 per minute [10, 16, 22, 30, 32, 36]. The amplitude is also varied - from barely noticeable contractions of individual muscles or groups of muscles to intense movements in the joints [8]. The topic of segmental myoclonus in MS is very poorly covered in the literature due to the rarity of this condition. J. Jankovic and R. Pardo [10] describe 5 patients with MS who exhibited segmental hyperkinesis of stem origin in the form of palatal myoclonus. Myoclonic hyperkinesis in a patient with MS in the case we observed was periodic, non-rhythmic, with an intensity of up to 10 times per minute and led to visual violent movement in the joints of the left hand.
Propriospinal myoclonus (PSM) is the second type of SM, which differs from SSM by the involvement of a larger number of muscle groups in hyperkinesis; along with the limbs, twitching is also observed in the trunk [15-19, 32]. This occurs due to the spread of pathological impulses along the propriospinal tract, and many segments of the spinal cord are successively involved in hyperkinesis [14, 19]. Unlike SCM, propriospinal twitches often do not have a specific etiology. Some authors [17] associate their occurrence with neck trauma, tumor, viral myelitis and psychogenic factors. The literature describes a case of Lyme borreliosis, which manifested itself clinically in the form of PSM [37]. With PSM, rhythmic or nonrhythmic axial flexion movements are observed, involving the neck, body, and limbs in hyperkinesis, with a frequency of about 1-6 Hz. Hyperkinesis usually occurs spontaneously, in a horizontal position on the back and can be provoked by cutaneous stimulation of the abdominal area or by inducing tendon reflexes [17, 19]. In the described patient, only one arm was involved in hyperkinesis, the trunk and lower limbs remained intact, which rather indicates the segmental nature of the lesion, without massive involvement of the propriospinal tract.
There is a single description of PSM in MS [11]. A patient with MS periodically, after previous sensitive sensations in the neck (tingling), developed spontaneous irregular twitching in the right shoulder and arm. Violent twitching spread to the trunk and hip flexors on the right side. On MRI, the authors identified lesions in the cervical segments C2, C3, C4. The authors explained the development of PSM by the fact that lesions in the white matter could lead to disinhibition of spinal activity, but they assumed that the cause could also be the hyperexcitability of the demyelinated axon, which in such a damaged state is capable of spontaneously or reflexively generating impulses of pathological muscle activity.
Both types of MS are characterized by the persistence of hyperkinesis during sleep and relative resistance to external stimuli - they do not increase under the influence of auditory, visual, tactile stimuli or motor activity [10, 14, 16, 27, 30], although there are descriptions of cases in the literature SSM with disappearance during sleep and sensitivity to external stimuli [22, 31, 32]. It is believed that as the disease progresses, a reaction to external influences may appear [15]. For SM, the postural component is more pathognomonic—increased hyperkinesis in a certain position, as well as worsening twitching during fatigue and emotional stress [31, 32]. The SMS observed in the patient under study persisted during sleep, were not dependent on auditory and visual stimuli, but increased due to emotional stress and fatigue, and decreased with alcohol intake.
The next important distinguishing feature of SM is the absence of pathological activity on the EEG. Joint EEG-EMG should exclude the presence of cortical hyperexcitability preceding muscle contraction [10, 16, 30]. In the case under consideration, the EEG did not show any foci of hyperexcitability, which made it possible with a high probability to exclude the cortical nature of hyperkinesis.
Surface EMG in SM reveals rhythmic or semirhythmic discharges that are usually synchronous with a stereotypical duration and frequency. EMG studies of SMS demonstrate discharges lasting more than 100 ms (up to 1000 ms) and limited to one or two adjacent myotomes. With SCI, myoclonic discharges can last from 50 ms to 4 s, they are formed from the abdominal and cervical segments and spread slowly rostrally and caudally, while the cranial muscles remain intact. PSM is characterized by a delay between discharges and their sequential propagation, which is due to the slow conduction of the impulse along the propriospinal tract [17, 30]. In the case we are describing, the duration of the discharge was 70 ms, which does not really correspond to the description of segmental myoclonus presented in the literature, but is more characteristic of propriospinal ones. However, neither clinically nor neurophysiologically we observed the spread of forced muscle contractions, which most likely excludes the propriospinal nature of myoclonus.
The observation we described demonstrates a clear picture of SSM in MS. The absence of epileptic activity on the EEG, the presence of discharges in the muscles of the left arm (segment C7), the involvement in hyperkinesis of the muscles of the left upper limb, the innervation of which is provided by 3-4 adjacent segments, and, finally, registration of foci of demyelination in the spinal cord, namely at the level of the segments C2, C4, C5, C6 of the cervical spine - all this confirms the spinal segmental nature of myoclonus. The cause of SSM most likely was foci of demyelination in the spinal cord. The disappearance of hyperkinesis after hormone therapy strengthens our hypothesis about the genesis of violent movements.
There are various hypotheses for the mechanism of development of SM [8, 21, 26, 31, 32, 38-40]. Considering that myoclonic hyperkinesis in the observed patient appeared occasionally at rest and manifested itself most clearly when maintaining a posture, the most likely variant of the development mechanism is based on the rupture of intersegmental connections by foci of demyelination in the spinal cord [18]. This could lead to local dysregulation of the gamma motor neuron loop with the subsequent emergence of spontaneous neuronal impulses in the spinal cord segments and the formation of myoclonic hyperkinesis. The location of the lesions relative to the gray matter of the spinal cord may have been important.
Thus, the main reference points for diagnosing SSM in the above observation can be: 1) involvement in hyperkinesis of a limited group of muscles innervated by several neighboring segments of the spinal cord; 2) the absence of influence of external stimuli (auditory, visual, tactile) and active movements on the severity of hyperkinesis; 3) preservation of hyperkinesis during sleep, their intensification under the influence of fatigue and emotions, the appearance of myoclonus in a certain position; 4) absence of hyperexcitability on the EEG; 5) pathological EMG activity of muscles in limited myotomes with an intensity of 70 ms.
Treatment of SSM, in particular in MS, involves treatment of the underlying disease - stopping the exacerbation with the use of glucocorticosteroids. If there is no effect, clonazepam is considered the drug of choice at a dose of up to 6 mg per day [10, 17, 18, 22, 30]. Baclofen therapy may improve nocturnal myoclonus in the legs [10]. The literature contains mention of the effectiveness of topiramate and levetiracetam in SM. Tetrabenazine is used when there is no effect from other drugs [10, 30]. It is possible to use drugs in combination, such as tizanidine, clonazepam and baclofen [38]. There are descriptions in the literature of the positive effect of botulinum therapy for SM [17, 18, 30].
In conclusion, we note that the above observation demonstrates SSM as one of the rarest manifestations of MS. The basis of this “atypical” symptom of MS was a focus of demyelination located in the spinal cord of the cervical region.
How does an autoimmune disease affect our visual system?
In multiple sclerosis, symptoms from the visual organs are observed. Moreover, it is often blurred vision, eye pain and other ophthalmological symptoms that prompt a person to see a doctor, where he is diagnosed with MS.
This disease may be characterized by a variety of visual symptoms.
- Decreased visual acuity (from slight to pronounced, with only light perception retained).
- Blurred vision.
- Pain in a moving eye may be combined with a headache.
- Changes in visual fields: the appearance of spots before the eyes, concentric narrowing.
- Increased photosensitivity.
- Changes in color perception - the patient distinguishes shades worse, sees flickering highlights.
- Impaired spatial, “volumetric” vision.
Often, a complex of such symptoms indicates a disease that often accompanies MS - retrobulbar optic neuritis.
Why does vision suffer in MS?
The eyes, as an organ of vision, are closely connected to the brain, where the visual cortex is located, responsible for processing visual data. The optic nerve is a critical pair of cranial nerves that transmit visual signals from the retina to the brain. The quality of vision directly depends on the proper functioning of the optic nerve. It is natural that damage to the membranes of the thin filaments of the nerve substance of the brain negatively affects the condition of the retina and optic nerve.
Neuritis is an inflammatory process in the optic nerve. In the general classification, ascending and descending neuritis are distinguished. The first is called papillitis, and with it the inflammation is concentrated inside the eyeball. Descending neuritis is retrobulbar, and with it inflammation can spread along the entire length of the nerve from the eye to the area of the intersection of nerve fibers, the so-called chiasm.
Diplopia
This is the name for the effect of double vision, which occurs due to uncoordinated functioning of the muscles responsible for the movement of the eyeballs. Discoordination of the eye muscles leads to a displacement of the visual axis of one eye, as a result of which the image falls not in the center of the retina, but in another area, which leads to the effect of double vision.
This problem often develops as a result of muscle weakness and is especially pronounced when there is a lot of strain on the eyes. Although there is no special treatment for this condition, it cannot be ignored. Diplopia may indicate the development of multiple sclerosis or other diseases.
Retrobulbar optic neuritis as a symptom of MS
Experts note that retrobulbar neuritis often remains the only symptom of MS for many years. According to statistics, this diagnosis is made in approximately 15% of patients with the initial form of the disease. As the autoimmune disease progresses, retrobulbar neuritis is detected in half of all patients.
If the manifestations of the inflammatory process do not greatly interfere with a person, he may not visit doctors for a long time. This leads to late diagnosis of the disease, when the effectiveness of treatment will be much lower than at an early stage.
Experienced ophthalmologists who see signs of retrobulbar neuritis in a person must initiate a full diagnostic examination and send the patient for consultation and diagnosis, including to a neurologist.
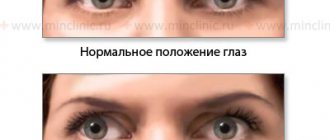
Double vision
This phenomenon is scientifically called diplopia and occurs when the paired eye muscles responsible for eye movement are weakened and cannot work synchronously. Discoordination leads to the fact that the image in a person’s eyes splits. The problem is aggravated by high eye strain or long periods of work at the computer.
Diplopia interferes with driving a car and leading a normal lifestyle, but usually does not require special treatment. However, if you notice diplopia, you should definitely get examined, as it can be an early sign of MS.
Specificity of retrobulbar neuritis in multiple sclerosis
Descending optic neuritis in multiple sclerosis can manifest itself with the same symptoms as other types of neuritis. But at the same time, experts identify a number of features that are characteristic of the inflammatory process that develops against the background of MS.
- Remitting course of the disease. Patients with multiple sclerosis are characterized by a wave-like course of neuritis, in which periods with acute, pronounced symptoms are followed by complete disappearance or significant weakening of the symptoms of the disease. After a period of remission, a relapse often occurs again.
- Short-term decrease in visual acuity. Inflammation of the optic nerve is often accompanied by a sharp deterioration in vision: the patient begins to see less clearly or has difficulty distinguishing the contours of objects, and a feeling of fog and blurriness may occur. At the same time, a feature of optic neuritis against the background of MS is the fact that such symptoms can be short-term, and after 7-20 days, visual acuity and clarity are completely restored. Experts note that with no other types of retrobulbar neuritis does a complete and such rapid restoration of visual functions occur. At the same time, during the period of further exacerbations, vision restoration occurs more and more slowly and is no longer complete. Such specificity of clinical manifestations of neuritis often leads to late diagnosis of multiple sclerosis. Since vision is restored quite quickly after the first sharp fall, many patients believe that there is no reason to see a doctor. In fact, it is during this period that it is important to contact a specialist who will correctly diagnose and prescribe treatment. At an early stage, there is a high chance of preserving vision and slowing the progression of the disease.
- Daily fluctuation of visual acuity. Optic neuritis in MS is characterized by changes in visual acuity at different times of the day. In particular, patients with multiple sclerosis see more clearly and clearly in the morning than in the evening. In this case, the range of fluctuations in diopters can be 0.05-0.2 diopters. Often, a decrease in visual acuity is observed after playing sports, physical activity and eating hot food.
- Localization of blind spots in the center. Scotomas characteristic of optic neuritis in multiple sclerosis are usually localized in the area of central vision. They may appear as dark circles or spots before the eyes. Often, scotomas in MS are accompanied by a narrowing of the visual field in the periphery. During periods of remission, when vision is restored, the scotoma from the center of the visual field usually disappears.
- Unstable loss of areas of the visual field. Optic neuritis often leads to loss of certain parts of the visual field. The specificity of the disease that develops in multiple sclerosis is that the loss of visual fields is changeable and unstable. Simply put, blind spots can appear and disappear, appearing in one place or another.
- Temporary disturbances in color perception. Impaired color perception in retrobulbar neuritis associated with MS also has its own characteristics. Like some other symptoms, decreased color sensitivity is often temporary. The patient may notice that he has begun to distinguish colors worse, but after a short time normal color perception returns to him. Another characteristic feature of the pathology is that the patient’s sensitivity to all colors is impaired.
- Pain in the eyes. Almost always, retrobulbar neuritis in MS is accompanied by painful sensations in the eyes and swelling of the eyelids. The most pronounced pain occurs when the patient tries to look up or presses on the eyeballs. Eye pain in multiple sclerosis can last from several hours to several days and is explained by irritation of the optic nerve sheaths that occurs when muscle tendons are pulled. Painful sensations can occur either in parallel with the loss of visual function or precede it.
- Damage to the optic nerve on one side. Retrobulbar optic neuritis in MS often affects only one eye. Cases of bilateral neuritis have also been encountered in practice, but they are more rare.
- Nonspecific damage to the fundus and nerve disc. During an ophthalmological examination, there are often no specific changes observed in the fundus and optic nerve head that could indicate MS with 100% accuracy. Moreover, at an early stage of the disease, the condition of the fundus is often normal.
- Damage to the optic nerve in MS is accompanied by double vision. Diplopia often occurs as a sign of damage to the brain stem. Nystagmus may also indicate the same disorder (it is characteristic of 70% of cases). It is possible to develop exophthalmos, in which the eyeballs protrude forward, or ptosis.
- Pallor of the optic disc in the temporal zone. Optic nerve atrophy and disc pallor usually begin in the temporal half.
- Unusual reaction of the pupils to light. Damage to the optic nerve can be externally manifested in the dilation of the pupils under the influence of light (usually, in bright light, the pupil, on the contrary, narrows). Also, a sign of pathology can be hippus - a paroxysmal condition in which the pupil rhythmically narrows and dilates.
Diagnosis of multiple sclerosis
Diagnosis of multiple sclerosis is somewhat difficult, especially in the early period. This is due to the variety and nonspecificity of symptoms.
The first stage of diagnosis is a thorough collection of complaints and clarification of the medical history. Noteworthy is the undulating course of the disease, signs of multifocal damage to the nervous system, and the variability of clinical manifestations.
At the stage of physical examination, cerebellar and pyramidal functions are assessed, the fundus and visual acuity are examined.
Laboratory diagnostics include a general blood test, a general urinalysis, a biochemical blood test, and an analysis of cerebrospinal fluid (cytosis and an increase in immunoglobulins in the cerebrospinal fluid are noted).
The most informative instrumental research method for making a diagnosis is magnetic resonance imaging, which makes it possible to identify foci of destruction of the myelin sheath in the central nervous system.
MRI results are evaluated taking into account the clinical picture. The method of studying evoked potentials is also used, which consists of recording the electrical response of the brain to the influence of external stimuli (visual, auditory, somatosensory).
The examination of patients is aimed not only at confirming the diagnosis, but also at excluding other diseases that have similar symptoms.
How is retrobulbar neuritis diagnosed?
Diagnosis of optic neuritis involves a thorough examination of the patient using various methods.
- Collecting anamnesis, interviewing the patient. At the first appointment, the doctor finds out from the patient what symptoms have been bothering him and for how long; Do you have any relatives suffering from multiple sclerosis? Have you had any vision problems before and what kind.
- Ophthalmological examination. Taking into account the patient’s complaints, the doctor usually conducts a study of visual acuity using special ophthalmological tables, assesses the quality and characteristics of color vision, examines the fundus of the eye, and studies the condition of the optic nerve head; checks the pupillary response to light stimuli, determines the visual fields for the presence of scotomas, concentric narrowing.
- Consultation with a neurologist. When the optic nerve is inflamed, the ophthalmologist often refers the patient to a neurologist for consultation, even in the absence of neurological symptoms. An examination by a neurologist is mandatory if the suspected cause of neuritis is multiple sclerosis.
- MRI of the head. Imaging can help detect signs of brain damage that are characteristic of MS, or identify other possible causes of descending neuritis, such as tumors. Before an MRI, the patient is usually injected with a special dye solution that ensures the optic nerve is clearly visible in the images.
- OCT. Another diagnostic procedure that allows you to confirm or refute the presence of retrobulbar or other neuritis. OCT is a painless examination method that can be performed in a matter of minutes. During the diagnostic process, the patient must look at a special mark while the tomograph scans the retina of the eye, allowing it to examine the structure of the optic nerve, the thickness of the fibers and the inner layer of the retina. In MS, neurons in the brain become inflamed and change their structure. Changes in brain neurons influence changes in the retina and optic nerve. Experts have found that in MS, there is usually a decrease in the thickness of the inner layer of the retina. This symptom can be detected during OCT. Also, during optical coherence tomography, a specialist can assess the speed of passage of the visual signal from the retina to the brain, which also allows making certain diagnostic conclusions.
- Blood tests and other studies. Descending neuritis can be caused, in addition to MS, by inflammation in the visual organs, general infectious diseases, pathologies of internal organs, and Devic's syndrome. In the latter case, a blood test to detect specific antibodies helps to find out the cause.
The main task of diagnosis is to establish what disease or pathological condition provoked damage to the optic nerve. Indeed, with retrobulbar optic neuritis, treatment will directly depend on those pathological processes in the body that provoked inflammation.
Moreover, treatment of any optic neuritis should primarily consist of treating the underlying pathology.
Chapter 5. Visual impairment and eye movements
Loss of vision
It may occur as a result of damage to the visual pathway running from the retina to the posterior parts of the cerebral hemispheres. Due to the high sensitivity of the visual system, the appearance of even such a minor symptom as “veils before the eyes” may indicate the presence of a condition that threatens the patient’s vision and life, therefore, the doctor’s most serious attitude to the patient’s complaints is required.
Approach to the patient
Anamnesis. The most important question to clarify is how quickly the visual impairment developed - acute, subacute or chronic. It is also important whether, in the patient’s opinion, the visual impairment affected one or both eyes (it is not always easy for the patient to determine this). Other areas of investigation include identifying associated symptoms (eye pain, headache), predisposing diseases (hypertension, diabetes mellitus, multiple sclerosis, AIDS), exposure to medications and toxins, and family history (visual status of relatives).
Examination. It is important to find out the mono- or binocular nature of the visual impairment, to identify loss of visual fields (central scotoma, hemi-anopsia, etc.). Assessing visual acuity and visual fields in each eye is of paramount importance. Next, the cornea, lens, choroid, fundus, and pupillary reflex are examined to assess the condition of the retina and optic nerve (a decrease in the pupil’s reaction to light is an indicator of optic nerve dysfunction). A detailed neurological examination to identify pathological processes in the retro-orbital zone completes the study.
Assessment of visual fields makes it possible to distinguish damage to the anterior part of the visual analyzer (optical media of the eye, retina, optic nerve to the chiasm) from the posterior one (optic tract, lateral geniculate body, radiatio optica and visual representation in the occipital lobe cortex). Damage to the anterior part of the visual analyzer can lead to mono- or binocular impairment; damage to the posterior parts of the visual analyzer leads to similar changes in the visual fields of both eyes. In Fig. Figure 11-1 shows the most common loss of visual fields, the image is differentiated depending on the damage to one or another part of the visual pathway.
In table Table 11-1 presents typical causes of non-traumatic visual impairment. The differential diagnosis, based on history and examination, should be limited to a single category (eg, acute monocular visual impairment). New information gleaned from the history and examination may further narrow the diagnosis, but this requires additional testing.
Central scotoma (optic neuritis, toxic or metabolic optic neuropathy) Arcuate scotoma (ischemia of the optic nerve or a reaction to increased intraocular pressure - glaucoma) Loss of the upper half of the visual field (anterior ischemic optic neuropathy; thrombosis of the branch retinal artery) Centrocecal scotoma (neuritis optic nerve; toxic, metabolic or congenital optic neuropathy) Narrowing of the visual field (retinal degeneration, optic nerve compression)
Chiasma Bitemporal (compression of the chiasm by a tumor) hemianopsia
Posterior visual pathway Homonymous hemianopsia (significant unilateral lesion of the posterior segment of the visual analyzer) Right-sided upper quadrant hemianopsia (unilateral severe lesion of the temporal part of the radiatio optica) Preservation of only (bilateral lesion of the central part of the visual cortex) visual field - “tubular vision”
Rice. 11-1. Loss of visual fields caused by damage to the anterior, chiasmal or posterior portions of the visual pathway.
Table 11-1 Most common causes of visual impairment
SHARP
Monocular
Anterior visual pathway: ischemia or vascular occlusion (anterior ischemic optic neuropathy), temporal arteritis, central retinal artery or vein occlusion; immunological cause (optic neuritis, papillitis); retinal disinsertion.
Binocular
Anterior visual pathway (less common): bilateral anterior ischemic optic neuropathy.
Posterior visual pathway: infarction or hemorrhage into the brain; hemorrhage into the pituitary gland.
SUBACUTE OR CHRONIC
Monocular
Anterior visual pathway: compression by a tumor (optic nerve sheath glioma or meningioma); predominantly unilateral manifestation of binocular visual impairment.
Binocular
Anterior visual pathway (NB may be asymmetrical and therefore appear monocular): clouding of the cornea, lens (cataract), or vitreous; retinal degeneration; retinal vasopathy (hypertensive, diabetic); deficiency of nutritional factors (vitamin B12 deficiency), poisoning (methanol, ethambutol, quinine); infectious lesions of the retina (toxoplasmosis); congenital optic neuropathy (Leber's disease); increased intraocular or intracranial pressure (glaucoma, disc edema, pseudotumor cerebri).
Posterior visual pathway: primary or metastatic brain tumor or other space-occupying process (abscess); immunological factors (multiple sclerosis); infections (progressive multifocal leukoencephalopathy), parasellar tumor (pituitary adenoma, craniopharyngioma).
Additional examination: slit lamp (eye damage); perimetry (assessment of changes in visual fields); measurement of intraocular pressure (glaucoma); MRI of the head (infarction or hemorrhage in the brain, tumor, demyelination, compression damage to the tissues of the orbit, optic nerve, chiasm) electroretinography (retinal degeneration); fluorescein angiography (damage to retinal vessels); lumbar puncture (multiple sclerosis, pseudotumor cerebri); visual, auditory and somatosensory potentials (multiple sclerosis) ESR (temporal arteritis).
Eye movement disorders
Diplopia
The most common symptom of eye movement disorder. The cause may be damage to the oculomotor nerves (III, IV, VI), the neuromuscular synapse, and the external muscles of the eye.
Dysfunction of the oculomotor nerves. With isolated damage to the oculomotor nerves, the following signs are revealed:
III nerve - diplopia horizontally and vertically; restriction of upward and downward movements of the eyeball; ptosis of the upper eyelid; the pupil is dilated, there is no reaction to light.
IV nerve - vertical diplopia when looking down; at rest, the eye is slightly raised upward, compensatory tilt of the head.
VI nerve - horizontal diplopia; inability to turn the eye outward; at rest the eyes are turned inwards.
The most common causes of isolated damage to the oculomotor nerves: diabetic and idiopathic vasopathy, together accounting for about 1/2 of all cases. Other common causes: aneurysm (especially the III nerve), tumor (especially the IV nerve), trauma (especially the VI nerve). More rare causes: sinusitis, syphilis, herpes zoster, increased intracranial pressure (IV pair), DBST or vasculitis, meningitis, sarcoidosis.
For isolated lesions of the third nerve, it is most important to distinguish between infarction due to vasopathy, which impairs the innervation of the pupil, and compression of the posterior communicating arteries by the aneurysm, which almost always reduces the pupillary reflex. MRI, MR angiography, or cerebral angiography may be needed to differentiate the two diseases.
Neuromuscular transmission disorders. Myasthenia gravis manifests itself in more than 60% of patients with ocular symptoms, diplopia and (or) ptosis, and isolated ocular symptoms are observed in more than 90% of patients. The pupil reaction is always normal. A test with Edrophonium chloride (10 mg intravenously) is diagnostically significant. [In Russia, a proserine test is usually carried out. — Approx. ed.
Ocular myopathies. Diplopia as a result of damage to the extraocular muscles can be a consequence of the inflammatory process (orbital myositis), infiltration (thyroid ophthalmopathy), and tissue displacement (orbital trauma). The diagnosis is confirmed by pressure testing on the eyeballs, in which the mechanical resistance of the anesthetized eyeball is assessed. Other eye movement disorders include: Nystagmus: rhythmic eye movements; Nystagmus itself is not a pathological symptom, but can appear when there is a disorder in the relationship between central and peripheral vestibular functions.
Internuclear ophthalmoplegia is a disorder of combined movements of the eyeballs due to damage to the medial longitudinal fasciculus in the brain stem.
Supranuclear gaze palsy - loss of voluntary control of horizontal or vertical eye movements; occurs when descending connections from the cerebral cortex to the brainstem are disrupted.
Is it possible to cure optic neuritis in multiple sclerosis?
If multiple sclerosis has led to the development of neuritis affecting the optic nerve, the prognosis of treatment will largely depend on early diagnosis.
To date, there is no specific therapy for MS that could completely rid a person of this disease or restore the integrity of the nerve fiber sheaths. If descending optic neuritis is diagnosed in MS, treatment of this pathology will be symptomatic and also aimed at suppressing the activity of the immune system.
It is almost impossible to completely cure ophthalmological pathology while maintaining the underlying autoimmune disease, but if the disease is diagnosed in a timely manner, before irreversible changes, there is a chance to preserve and restore vision, reduce the number of exacerbations and reduce the severity of symptoms.
Treatment
Treatment of multiple sclerosis is aimed at solving several problems:
- stopping the active immunoinflammatory process,
- decreased activity of the immune system to nerve fiber sheaths,
- slowing down the development of the disease, stopping the appearance of new “plaques”,
- combating symptoms that significantly impair the quality of life.
To solve problems, medications and physiotherapy are used.
Complex drug therapy
During treatment, it is important to take immunomodulators and anti-inflammatory drugs. The following drugs are especially well known:
- Interferons beta. The drugs have an immunomodulatory effect on the main components of immune reactions.
- Medicines based on glatiramer acetate. Medicines in this group are capable of replacing myelin antigens and triggering the process of inhibition of T1 lymphocytes. In this case, T2 lymphocytes, on the contrary, are activated. Due to this, the drug has a neuroprotective and anti-inflammatory effect.
- Fingolimod. Modulator of sphingosine-phosphate receptors on lymphocyte membranes. Significantly reduces the number of “autoaggressive” T cells circulating in the blood.
- Natalizum. Slows down penetration through the blood-brain barrier and reduces the activity of T-lymphocytes in areas of axonal damage. The inflammatory process is significantly slowed down.
During exacerbations, when the disease is accompanied by obvious attacks, adrenocorticotropic hormone and corticosteroids (methylprednisolone) are used. Thanks to these drugs, it is possible to quickly reduce the movement of immune cells to the spinal cord and brain. But these drugs are only good as short-term therapy. They are not suitable for long-term use, as they can cause addiction.
If the disease is accompanied by signs of depression, the doctor may prescribe amitriptyline or melipramine. However, the prescription of these drugs is done extremely carefully - only after a detailed examination. Unfortunately, many patients already have urinary retention, and amitriptyline and melipramine can significantly aggravate the situation. An alternative for such patients can be all kinds of selective inhibitors without anticholinergic properties, but with an excellent ability to reuptake serotonin. These drugs include trazadone, sertraline, fluoxetine, and paroxetine.
Also, in the presence of depression, agomelatine has been widely used in recent years. This is a drug with a melatonergic mechanism of action. It normalizes circadian rhythms (oscillations).
If you have problems with urination, targeted therapy is needed to solve this problem.
If the main problem is urgency, tolterodine oxybutynin, amitriptyline, nifedipine are used.
If concerns are associated with emptying the bladder, the blocker terazosin helps. But it is important that when taking the drug there is careful monitoring to ensure that orthostatic hypotension does not develop.
Some patients may also be additionally prescribed medications aimed at reducing external sphincter tension. Among them are diazepam, tizanidine.
The above drugs are used in tablet and injection forms.
Hypobaric oxygenation
Oxygen saturation is a big help for patients with multiple sclerosis. This is possible through the hypobaric oxygenation procedure.
Hypobaric oxygenation is especially relevant for patients in whom multiple sclerosis is accompanied by cardiovascular diseases and diabetes.
Hypobaric oxygenation is carried out in a pressure chamber. Oxygen is supplied under high pressure. During the process of hypobaric oxygenation, adaptation and regeneration mechanisms are activated.
Massage
An excellent way to reduce discomfort and pain in patients with different types and stages of sclerosis is massage. Massage is especially useful for solving the following problems:
- Relaxes muscles and relieves spasticity.
- Activation of blood circulation.
- Preventing bedsores. Relevant for people who have to spend most of their time in bed.
Diet therapy for multiple sclerosis
- A common principle for all patients with multiple sclerosis is to limit sources of fast carbohydrates in the diet. The main ones are sugar and baked goods made from refined flour.
- The remaining principles of nutrition largely depend on what specific problems the patient has in each particular case.
- If chewing is difficult, it is recommended to eat pureed foods.
If you have constipation, you should use more liquid foods (if there are no problems with the urinary system at the same time) and products with bifidobacteria.
The main directions of therapy for descending neuritis
Many patients are concerned about the question - if there is no specific treatment for MS, what kind of therapy is carried out for retrobulbar neuritis.
- Experts note that treatment is aimed at achieving several main goals:
- slow down the activity of the immune system, which destroys the body’s own cells;
- change the course of multiple sclerosis;
- eliminate or reduce the severity of ophthalmological symptoms; prolong periods of remission, ease periods of exacerbation.
To achieve these goals, predominantly medicinal methods are used.
Treatment of retrobulbar optic neuritis in MS
The correct diagnosis and established cause of neuritis allow the patient to be prescribed treatment. If experts have determined that the symptoms of optic neuritis are caused by multiple sclerosis, then the treatment regimen may be approximately as follows.
- Glucocorticoid drugs, in particular methylprednisolone, are prescribed in the acute period of the disease. They have a powerful anti-inflammatory effect, eliminate symptoms of damage to the optic nerve, slow down the progression of immune system cells to the brain, and reduce the amount of antibodies in the blood. Corticosteroids are used primarily to relieve signs of neuritis during an exacerbation. As a rule, the medicine is administered intravenously at the dose prescribed by the doctor for three to seven days. Subsequently, oral administration of the same glucocorticoids is prescribed with a gradual reduction in dosage. It must be taken into account that damage to the optic nerve continues not only during the period of exacerbation, but also in the remission stage, therefore, ophthalmologists often prescribe courses of maintenance hormonal therapy outside the acute phase of the disease.
- Anti-inflammatory non-steroidal drugs are used to reduce the inflammatory process.
- Immunomodulators or immunosuppressants allow you to suppress the activity of the immune system and thereby reduce its destructive effect on the membranes of nerve fibers. Since there is no specific treatment for multiple sclerosis, drug effects on the immune system become one of the main therapeutic methods.
In addition to the methods listed, the treatment regimen may include dehydration therapy, the administration of vitamin B12, and drugs with antioxidant effects.
Fundus pathology
Age-related macular degeneration
Age-related macular degeneration is one of the leading causes of central vision loss in the adult population.
Increasing people's life expectancy and improving the quality of diagnostics make this disease the first place among the causes of persistent vision loss. The causes of the onset and progression of this disease have not yet been well studied, and at present all efforts of doctors are aimed only at stabilizing the pathological process and visual functions.
The disease includes a set of pathological changes in the central zone of the retina associated with age, which can be divided into stages or forms. Depending on the form and course of AMD, various treatment options are offered. All treatments for AMD are based on early and accurate diagnosis, so in the early stages of the disease, adequate treatment can stop the progression and prolong active writing and reading activities for our patients for years.
Non-exudative forms of AMD are the initial stage of the disease, a period of precursors. As a rule, there is no decrease in visual functions. At this stage, dynamic monitoring, antioxidants and retinoprotectors in the form of nutritional supplements are important.
Atrophic forms of AMD develop slowly, but inevitably lead to loss of central vision. As a rule, the disease is detected in both eyes, possibly with varying degrees of severity. Currently, periodic courses of vascular and retinoprotective (improving retinal nutrition) treatment are carried out as treatment. Patients are advised to wear sunglasses when outdoors.
Exudative forms of AMD are characterized by a severe course and a sharp decrease in vision. At first, before the loss of central vision, patients notice the curvature of the contours of objects, straight lines, and text. It is increasingly difficult to do small work close to the eyes (sewing, knitting, reading and writing). The reason lies in the rapid growth and high activity of newly formed vessels located under the retina. Newly formed vessels have a thin permeable wall, which ultimately leads to the appearance of edema (fluid accumulation under the retina) and hemorrhage in the central zone of the retina. In the final stage of AMD, there is a loss of central visual functions due to the development of atrophy or scarring; peripheral vision, as a rule, remains unaffected. All efforts in the treatment of the exudative form of AMD are aimed at combating newly formed vessels. Currently, the use of anti-VEGF drugs is widely used.
Epiretinal macular fibrosis
Epiretinal macular fibrosis can be either a primary retinal disease or a consequence (complication) of other eye diseases (inflammatory, vascular, trauma, etc.).
Most often, primary epiretinal macular fibrosis occurs after 50 years, but recently there has been a trend towards “rejuvenation”. The disease begins with the appearance of a membrane (thin film) on the surface of the retina, usually in or near the central zone. The contracting membrane causes wrinkling and deformation of the underlying retina, and as the membrane thickens, severe deformation and even partial flat retinal detachment occurs.
At the initial stages of development, epiretinal fibrosis is asymptomatic. This condition does not require intervention; dynamic observation is sufficient. As it progresses, curvature of the outlines of objects and straight lines and a noticeable decrease in visual acuity may appear. In such cases, it is advisable to perform surgical intervention - separation and removal of the membrane.
In rare cases, the membrane may peel off on its own, leading to the disappearance of all symptoms.
Idiopathic macular hole
An idiopathic macular hole is a perforating tissue defect in the center of the retina. Typically occurs over the age of 60 years. The reason lies in the traction of the detached posterior hyaloid membrane fixed to the center of the retina. The disease develops in stages, and in the early stages it is asymptomatic. In later stages, the patient notices a black spot in front of the eye, often discovered by chance when closing the healthy eye. Peripheral vision is not affected. To make a diagnosis, examination of the retina is often sufficient; optical coherence tomography may be required to document the diagnosis and clarify the stage. At the first stage of the disease - the threat of macular hole formation - no treatment is carried out, since spontaneous reverse development may occur at this stage. At later stages, surgical intervention is indicated - posterior vitrectomy with elimination of the traction factor.
Central serous chorioretinopathy
This is a common pathology of the fundus, affecting mainly young patients. This disease is idiopathic and still much about the causes and development of this disease remains unclear. Vision usually does not suffer much. Patients often complain of blurred vision in one eye, the appearance of curvature of the contours of objects and straight lines. Diagnosis does not present any difficulties, however, to determine further treatment tactics for the patient, fluorescein angiography is indicated. It is the results of this examination that determine whether you will be offered simple observation and conservative treatment, laser treatment or intravitreal administration of an anti-VEGF drug.
Diabetic rhinopathy
Damage to the organ of vision in diabetes mellitus occupies a special place, as it significantly affects the quality of life of people. Moreover, of all the clinical manifestations of diabetic eye damage, retinopathy poses the greatest danger, being the main cause of progressive and irreversible vision loss up to blindness, which occurs 25 times more often in patients with diabetes than in the general population.
The main factor in the development and progression of DR is chronic hyperglycemia, i.e. high sugar level.
Currently, most European countries use a classification according to which there are three main forms of retinopathy:
- non-proliferative retinopathy;
- preproliferative retinopathy;
- proliferative retinopathy.
Reduced visual acuity in diabetic retinal damage occurs as a result of three reasons. Firstly, due to the presence of maculopathy (swelling of the retina in the central zone), central vision may suffer. Secondly, at the stage of proliferative retinopathy, hemorrhages that arise from newly formed vessels cause a sharp deterioration in vision. Third, the formation, proliferation, and contraction of fibrovascular tissue leads to tractional retinal detachment, resulting in severe and often irreversible vision loss.
Timely detection of the earliest manifestations of eye diabetes is a top priority, since in the later stages of the process treatment is no longer promising.
However, in the initial stages of eye diabetes, pathological changes in the retina are not accompanied by visual disorders, so patients themselves seek medical help, as a rule, late. In this regard, great responsibility is placed on the work of dispensary ophthalmological observation and on the shoulders of the patient himself, whose serious attitude and responsible approach will help reduce the existing risk of vision loss due to eye diabetes.
There are two main directions in the treatment of diabetic retinal lesions:
The most stable compensation for diabetes mellitus and direct treatment of diabetic retinopathy.
Laser coagulation of the retina is the only effective treatment for diabetic retinopathy. Laser photocoagulation for diabetic retinal damage is aimed at stabilizing the process, and an increase in visual acuity is not always achieved. In severe proliferative retinopathy with the development of recurrent vitreous hemorrhages and tractional retinal detachment, laser coagulation is futile. In such cases, surgical treatment – vitrectomy – may be indicated.
For persistent maculopathy, regimens for intravitreal administration of an anti-VEGF drug are being developed.
Coates' retinitis
Coats disease is a congenital disorder that typically appears in childhood in boys and affects one eye. Most cases are diagnosed before age 20, with a peak incidence at the end of the first decade.
The reason for treatment may be strabismus, leukocoria or a red sore eye in an advanced form. Older children and, less commonly, adults may complain of decreased visual acuity in one eye.
Diagnosis is usually made by examining the fundus; cycloscopy may sometimes require fluorescein angiography.
In mild cases of the disease, dynamic observation is sufficient - examinations every six months. With a progressive course, numerous repeated sessions of laser coagulation are indicated and more careful monitoring is required, since relapses of the disease are possible within 5 years after complete regression. At an advanced stage of the disease with the development of retinal detachment, surgical treatment is indicated.
Eales disease
The disease has been known since 1880, when the occurrence of recurrent vitreous hemorrhages in young people in good health was first described.
Eales disease is a chronic inflammation of the vessels of the retinal periphery, accompanied by repeated hemorrhages and a gradual decrease in vision. The disease predominantly affects middle-aged males and is usually bilateral.
Patients complain of the appearance of floating spots or decreased visual acuity in one eye. In severe cases, repeated hemorrhages lead to tractional retinal detachment and secondary neovascular glaucoma.
There is no drug treatment for Eales disease. Hormone therapy is usually not effective. The only effective treatment method is timely laser coagulation of the retina, which allows to stabilize the pathological process and preserve the remaining vision.
In some cases, when retinal detachment occurs, there is a need for surgical treatment.
Fundus examination - cycloscopy should be performed annually. A case of relapse of the disease tens of years after the apparent stabilization of the process has been described.
Thrombosis of the central retinal vein or its branches
This condition is an acute circulatory disorder in the central retinal vein or its branches, threatening irreversible vision loss.
The disease usually occurs in people over 50 years of age against the background of arterial hypertension, diabetes mellitus, atherosclerosis, thrombophilia and other blood diseases.
Typically, patients note a unilateral, painless, sharp decrease in vision that occurs against the background of high blood pressure, after physical or emotional stress, after overheating, or drinking alcohol. Typically, patients can clearly indicate when their vision has decreased. Depending on the localization of the process, there may be complaints about the appearance of a spot in front of the eye, the appearance or increase of floating “spots”, loss of visual fields, and distortion of the contours of objects.
Treatment should be started immediately. This is an emergency condition requiring urgent hospitalization in a hospital. The best effect will be observed with timely and comprehensive treatment of the patient; the prognosis for vision will largely depend on visual acuity at presentation. To dissolve a blood clot occluding a vein, thrombolytic drugs are used, which are effective only in the first seven days from the onset of the disease. There will be no effect from their use in the future.
Another direction of complex treatment is the maximum reduction of intraocular pressure, resorption therapy and antioxidants. If there is diffuse edema in the center of the retina, the issue of lattice laser coagulation is decided. Recently, intravitreal administration of an anti-VEGF drug has been successfully used as a method of treating macular edema.
If there is a threat of the appearance of newly formed vessels as a result of prolonged retinal ischemia and the development of neovascular glaucoma, as a complication of thrombosis of the central retinal vein, panretinal laser coagulation of the retina should be performed, which is carried out in several sessions. The goal of laser treatment is not to improve visual function, but to prevent the development of neovascular glaucoma.
Central retinal artery occlusion
The disease is an acute blockage of blood circulation in the central retinal artery by a thrombus. Typically occurs in people over 60 years of age. The development of this disease is based on various reasons, the main ones being:
- arterial hypertension;
- atherosclerosis;
- heart valve pathology;
- tumors;
- eye injuries;
- systemic diseases.
As a rule, patients note acute unilateral and painless loss of vision, developing within a few seconds. Sometimes episodes of transient vision loss occur before complete loss of vision.
The prognosis for future vision is usually unfavorable. In most cases, visual acuity remains at the level of light perception. The exception is in the case of additional blood supply to the area of the central fovea of the retina of the cilioretinal artery, when visual acuity can be restored to the original level, but nevertheless there are significant losses in the visual fields.
There is no proven treatment for visual acuity, but it is an ophthalmic emergency and theoretically, timely dislodgment of the clot can prevent the development of irreversible visual changes. Attempts to dislodge a blood clot make sense in the first 48 hours from the onset of the disease. Therefore, in this case, it is necessary to urgently contact an ophthalmologist for help, and at the stage of first aid, massage the eyeball, the purpose of which is to first cause collapse of the lumen of the vessel, and then sharply expand it. If necessary, the patient can massage the eyeball independently using the following technique.
- The patient's head should be kept low to avoid orthostatic relative deterioration of the retinal blood supply.
- Using your fingers, press through the closed eyelid onto the eyeball.
- The eyeball is pressed into the orbit, first weakly, then with increasing force, and after 3-5 seconds it is suddenly released.
- After a few seconds the process is repeated.
Anterior and posterior ischemic neuropathy
A disease that is most common in older people. It is based on partial or complete infarction of the optic disc or its retrolamillary part, caused by occlusion of the vessels supplying the optic nerve.
Risk factors for development are arterial hypertension, diabetes mellitus, hypercholesterolemia, collagenosis, antiphospholipid syndrome, hyperhomocysteinemia, sudden hypotensive conditions, etc.
The onset of the disease most often manifests itself as a sudden unilateral loss or significant decrease in vision without any previous visual disturbances. Decreased vision is usually detected upon awakening, indicating a likely association with nocturnal hypotension.
Medical care is aimed at restoring and improving blood circulation in the system supplying the optic nerve and preventing the development of complete atrophy of the optic nerve.
Congestive optic disc
A congested optic disc is characterized by edema that develops against the background of increased intracranial pressure. The stagnant disc is almost always bilateral. Typically, visual disturbances appear only at the stage of optic atrophy (advanced), so often a congestive optic disc is a diagnostic finding during an examination by an ophthalmologist.
Clinical manifestations of increased intracranial pressure may include headache, sudden nausea and vomiting, impaired consciousness, transient episodes of blurred vision and double vision.
Causes of increased intracranial pressure:
- Obstruction of the ventricular system (congenital or acquired)
- Volumetric intracranial formations, including hematomas
- Meningitis, subarachnoid hemorrhage, previous injuries accompanied by diffuse cerebral edema
- Severe systemic arterial hypertension
- Idiopathic intracranial hypertension
- Hypersecretion of cerebrospinal fluid by a tumor of the choroid plexus of the brain.
All patients with stagnant discs should be examined by a neurologist and neurosurgeon to rule out intracranial masses.
Optic neuritis
Optic neuritis is damage to the optic nerve due to an inflammatory, infectious or demyelinating process.
Demyelinating neuritis is most common in multiple sclerosis. The onset of the disease is manifested by subacute unilateral vision loss. Sometimes vision loss is accompanied by dotted white or colored flashes or sparks. There is often pain when moving the eye or discomfort that precedes vision loss and usually lasts for several days. In most cases, defects appear in the field of vision.
The deterioration of visual functions lasts from several days to two weeks; further vision recovery occurs within six months. With repeated attacks, optic nerve atrophy develops.
Although some patients with optic neuritis do not have evidence of clinically detectable systemic demyelinating disease, the following series of observations indicate a close association of optic neuritis with multiple sclerosis.
In patients with optic neuritis and an initially normal MRI of the brain, the risk of developing multiple sclerosis over the next 5 years is 16%, and in patients with established multiple sclerosis, optic neuritis develops in 70% of cases.
Considering all of the above, when diagnosing optic neuritis, the doctor will definitely refer you to an MRI of the brain.
The proposed treatment with hormonal drugs and interferon can speed up recovery by up to 2-3 weeks. However, treatment does not affect final visual acuity.
Optic neuritis in infectious diseases is much less common. The cause may be diseases of the paranasal sinuses. This neuritis is characterized by repeated episodes of unilateral vision loss, severe headaches and signs of sinusitis. In this case, treatment is carried out jointly with an otolaryngologist. Therapy – local and systemic use of antibiotics.
The main cause of parainfectious optic neuritis is a viral infection. In addition, it can develop after vaccination. This form of neuritis occurs much more often in children than in adults. The disease usually develops 1-3 weeks after a viral infection and decreased vision is accompanied by neurological symptoms (headache, attaxia).
Treatment, as a rule, is not required due to the favorable prognosis, which involves rapid recovery of visual functions. However, with severe or bilateral damage, hormonal therapy is indicated.
Chorioretinal inflammatory diseases (chorioretinitis)
The causes of chorioretinitis can be infectious or non-infectious.
Among the infectious causes of chorioretinitis, the most common is toxoplasmosis. The causative agent of the disease is an intracellular parasite that lives in the intestines of cats.
Most often, the disease is detected in young, healthy adults who come to the doctor with complaints of decreased vision, floaters in front of the eye, and photophobia. When the inflammation is localized in the central zone of the retina, central vision is significantly affected.
In addition to toxoplasmosis, the infectious cause of chorioretinitis can be: toxocarosis, cytomegalovirus, herpes virus, secondary syphilis, candidiasis, histoplasmosis, tuberculosis.
If the diagnosis is reliably established and confirmed by laboratory research methods, treatment is carried out by an infectious disease specialist.
Hereditary dystrophic and degenerative diseases of the retina
Retinitis pigmentosa is a group of hereditary dystrophic diseases of the retina, characterized by subjective night blindness and loss of peripheral vision. Almost a quarter of all patients retain high visual acuity and the ability to read throughout their lives. However, annual examination is necessary to detect any significant decline in visual acuity, which may be due to a potentially treatable cause such as cystoid macular edema or cataracts.
Stargardt disease is the most common form of genetically inherited retinal dystrophy that occurs in adolescence. The onset of the disease occurs at the age of 10-20 years. There is a bilateral gradual decrease in central vision. Most patients maintain average visual acuity in at least one eye.
Best's disease is a rare hereditary degenerative disease of the retina. The disease usually progresses slowly through five stages and ends with macular atrophy and loss of central vision. In general, the prognosis is fairly good, as most patients retain sufficient vision for reading in at least one eye throughout their lives. If there is significant vision loss, it usually occurs slowly and begins after age 40.
Albinism is a group of genetically inherited diseases, which are based on a violation of the synthesis of the melanin pigment and which can be characterized by either isolated eye damage (ocular albinism) or systemic damage to the eyes, skin and hair.
Important clinical signs are
- Low visual acuity
- Pendulum-shaped horizontal nystagmus
- Red tint of the iris.
There is no pathogenetically based treatment for hereditary retinal diseases. There is an opinion and several experimental and clinical studies indicating positive dynamics and stabilization of the degenerative process of the retina with periodic use of drugs - tissue bioregulators.
Retinal disinsertion
This is the separation of the retina from the underlying pigment epithelium layer. The main types of retinal detachment: rhegmatogenous, exudative, traction.
Rhegmatogenous retinal detachment occurs secondary to a perforating retinal tear, as a result of which fluid from the vitreous body enters under the retina. Retinal tears are a common condition, most often occurring in myopia, pseudophakia, and after injury. In many cases, the ruptures are bilateral and multiple, occurring against the background of degenerative anomalies, developmental anomalies, and trauma.
Many ruptures are asymptomatic; sometimes ruptures are manifested by floating cloudiness in front of the eye and flashes of light, without affecting visual acuity. However, if a retinal detachment develops, there is progressive loss of visual field.
About 60% of all ruptures occur against the background of specific changes - peripheral degenerations. These are pathologically thin areas of the retina in which breaks spontaneously form. Peripheral retinal degenerations that predispose to retinal detachment (ethmoidal, “trace cochlea”, degenerative retinoschisis) as well as breaks are subject to laser coagulation in order to prevent rhegmatogenous retinal detachment.
Rhegmatogenous detachments are subject to surgical treatment, and the postoperative prognosis for vision depends on the duration of the disease and the extent of the detachment. If the retinal detachment does not involve the central (macular zone) and is fresh, the postoperative prognosis for vision restoration is relatively high.
Exudative retinal detachment is a detachment of the retina due to intraretinal or subretinal fluid leakage. By definition, such a detachment is not associated with a retinal tear. Look for signs of an underlying cause of fluid exudation, such as inflammation, vascular changes or tumors. Depending on the causes of exudation, etiopathogenetic treatment is used.
The main causes of tractional retinal detachment are: proliferative diabetic retinopathy, retinopathy of prematurity, penetrating trauma to the posterior segment of the eye. This is the most severe complication of the underlying disease, leading to blindness. In such cases, surgical treatment is indicated.
Are there preventive measures?
If inflammation of the optic nerve is associated with multiple sclerosis, then doctors recommend, in addition to mandatory treatment, to adhere to some preventive measures. The goal of prevention in this case is to prevent periods of exacerbation.
To control risk factors for this disease, it is important to follow several recommendations.
- avoid any infections or injuries;
- control your emotional state, avoid stress;
- avoid prolonged exposure to the sun, overheating or hypothermia;
- stop smoking and consuming other toxic substances.
It is impossible to cure multiple sclerosis and the neuritis that accompanies it, but taking pathological conditions under control, relieving symptoms, slowing progression, and preserving vision is possible with early diagnosis, correct treatment, and compliance with preventive measures.
Treatment of multiple sclerosis
Treatment of multiple sclerosis is aimed at preventing or slowing down disability, improving quality of life, and preventing the development of complications.
From the moment of diagnosis, all patients are prescribed course-modifying drugs for multiple sclerosis (MCD). This group of drugs includes glatiramer acetate, interferons, and monoclonal antibodies.
Symptomatic therapy is also indicated for patients. Glucocorticoids, drugs that improve blood microcirculation, nootropics, muscle relaxants, antidepressants, laxatives, and anticholinergics are prescribed.
For multiple sclerosis, physiotherapy and exercise therapy are recommended, as well as diet (limiting the consumption of animal fats, predominance of polyunsaturated fatty acids in the diet, sufficient intake of vitamins and minerals).
Early diagnosis of multiple sclerosis and adequate treatment with specialized drugs can slow down the negative manifestations of the disease and delay the onset of critical damage to the nervous system. The prognosis of the disease in case of refusal of treatment is extremely unfavorable. Thus, after 15-20 years, 2/3 of patients have difficulties with self-care, and 1/3 of patients are not able to move independently. Thanks to the advent of special drugs that slow down the progression of multiple sclerosis, it has become possible to prevent exacerbations, reduce the severity and prevalence of symptoms, which significantly slows down disability.