Stroke - symptoms, stages of stroke development
Among the stages of a stroke, it is worth highlighting the following stages:
- Transient ischemic attack;
- The second stage is a small stroke;
- The third is a completed stroke.
At the first stage of ischemic stroke, periodic disturbances associated with ischemia of areas of the brain appear. At the same time, there are also clinical signs that manifest such a stroke: the symptoms are mainly caused by an acute reversible disturbance of blood flow, as well as concomitant pathologies. These include:
- Hypertension;
- Hypertensive crisis;
- Thrombophilia;
- Varicose veins of the lower extremities and pelvis;
- Infectious endocarditis.
As a rule, stroke associated with thrombosis or embolism manifests itself without the stage of transient ischemic attack, while hypertensive variants have signs of reversible ischemia. Among them, headaches, a feeling of heat and facial flushing, nausea and vomiting, tachycardia, disturbances in the perception of auditory or visual information, and sweating are especially common. These signs are common to a large number of diseases, especially the circulatory system. Therefore, the importance of treatment at the stage of transient ischemic attacks is enormous.
Content
Minor stroke stage
In a condition such as a minor stroke, the symptoms are caused by ischemia of a region(s) of the brain. This is provoked either by thrombosis, or by the same arterial hypertension during a crisis. The predisposing factor is atherosclerosis of cerebral vessels and autoimmune lesions of the arterial wall.
At this stage, clinical symptoms become especially pronounced. Early signs of a stroke include:
- Speech disorders;
- Impaired motor function (hemiparesis, monoparesis or tetraparesis);
- Visual impairment, loss of visual function;
- Nausea and headache, vomiting;
- Loss of sensation in some areas of the body;
- Nonspecific symptoms listed above.
These disorders should be explained as follows: stroke and cerebral infarction provoke the death of nerve tissue cells, therefore the performance of functions of higher nervous activity is limited. Ischemia or hemorrhage most severely affects the cortex. It is divided into zones, the death of neurons in which causes so-called focal symptoms. It includes loss of sensitivity and motor function. If the size of the damage is small, then monoparesis may develop, that is, the inability to perform motor acts with one limb.
The wider size of the defect causes the development of hemiparesis - a violation of motor function in one half of the body. If the lesion affects a large area, then complete paralysis occurs. At the same time, the amount of damage to the somato-sensory areas of the cortex responsible for sensitivity and movement in each clinical case is separate.
Another sign is pain during a stroke. At the same time, the brain and spinal cord itself do not have pain receptors, therefore this sensation occurs due to damage to the soft tissues of the head and bones of the skull (hemorrhagic traumatic form), as well as due to a hypertensive crisis (ischemic form). At the same time, hypertension also causes a hemorrhagic form, which is characterized by pain in the crown and back of the head. They should be associated specifically with an increase in pressure, and not with the generation of brain tissue itself. Thrombosis of cerebral vessels occurs without pain, and therefore patients often do not seek help, especially if it is impossible to take the person to the hospital. In practice, any cases of impairment of motor function, speech, vision and hearing should be observed in a medical facility, because these signs can help establish a diagnosis of stroke.
Nausea and vomiting are characteristic signs of compression that characterizes the disease stroke. Moreover, these symptoms are characteristic of different locations of damage. Nausea is accompanied by dizziness, weakness and leads to vomiting. It does not bring relief and may occur several times.
Impaired consciousness during a stroke is an early sign. This is observed due to brain damage and disruption of the nutrition of areas of nervous tissue. They can manifest themselves as usual drowsiness, lethargy and coma. It is worth understanding that there is no such disorder of consciousness as drowsiness: here it is used for a correct analysis of the concepts and symptoms by which it is worth diagnosing the pathology at the initial stage. Sudden drowsiness is a sign that characterizes the development of precoma or coma. During precoma, the patient may respond to stimuli and speech, while coma is a complete loss of consciousness. If possible, it should not be allowed, trying to keep the patient conscious. This is needed to track new signs that will indicate the development of the process. Therefore, with a pathology such as stroke, treatment should be based not only on protocol manipulations and components of pharmacological therapy: it is important to take into account new symptoms, changing the tactics for correcting the condition and maintaining vitality.
Accomplished stroke
At this stage, the above signs are no longer important, because, as a rule, they are characteristic of an inpatient department. By this time, the patient has already been taken to a medical facility by ambulance and is in the intensive care unit. What is most important here is the tendency for the old signs of stroke to remain the most important and progress to disturb the condition. New symptoms do not appear except for those that characterize complications. With a pathology such as a stroke, the consequences of this clinical stage are far-reaching, because, in fact, there is no way to eliminate brain damage.
Long-term symptoms of stroke
This category of stroke symptoms is not particularly important for diagnosis and is provided only as an informational guide to complications and their development. Brain function should recover over several weeks or months. The patient continues to have difficulty fully controlling movement, speech, memory, vision, or hearing. It is also possible that these signs will last a year after the stroke, or will remain forever. Since the damage is localized at the level of the most highly differentiated cells, it is impossible to restore or replace them with new neurons (by the way, this does not happen in the body). Therefore, after a stroke, the patient has a set of symptoms that cannot be corrected. Based on this, it is worth understanding that recovery after a stroke is not complete, and therefore some functions will be lost forever.
Main causes of strokes
An immediate danger to cerebral circulation is posed by spasms, disruption of the integrity of vessel walls, and occlusion processes provoked by blood clots or cholesterol deposits. Most people have several main risk factors for developing pathology:
- physical inactivity: lack of physical activity causes systemic damage to the body;
- endocrine diseases: often lead to increased platelet production and excessive blood thickening;
- obesity: a platform for the development of many cardiovascular and metabolic disorders;
- chronic hypertension: due to increased load, blood vessels quickly wear out and become fragile;
- atherosclerosis: the lumen of the arteries gradually decreases due to plaque deposits in them;
- genetic predisposition: some people inherit a weak vascular system.
In young people, stroke is usually caused by congenital lesions of the cerebral vessels, consequences of traumatic injuries, and some systemic diseases, including severe hypertension.
In women during menopause, the risk of stroke increases due to age-related hormonal changes. Their bodies produce less estrogen, which protects blood vessels from damage. As a result, heart problems develop faster, weight increases, thyroid disorders occur more often, and cholesterol levels rise. One of the characteristic signs of menopause is an increase in the level of platelets in the blood. Combined with other changes and in the absence of a healthy lifestyle, the risk of stroke becomes more real.
Alcohol and tobacco smoking also systematically lead to vascular disorders: they destroy their structure, increase permeability, reduce tone and elasticity. These habits are dangerous for men and women of any age.
Vomiting in hemorrhagic stroke
Cerebral vomiting is also characteristic of severe brain damage as a result of hemorrhages - hemorrhagic strokes. With a hemorrhagic stroke, an intracerebral hematoma (a limited accumulation of blood in some area of the brain tissue) can form in the cerebral hemisphere.
Symptoms of hemorrhagic stroke. Violent cerebral manifestations develop - against the background of a hypertensive crisis, a headache appears or significantly intensifies, often in one half of the head, repeated vomiting without preceding nausea is typical, then the patient loses consciousness, the face becomes bluish or red, and breathing is hoarse.
After some time, a convulsive attack may develop with a predominance of seizures in one half of the body. The pupil of the eye on the side of the stroke dilates, but on the other side remains normal.
Patients always exhibit rigidity of the neck muscles: it is impossible to bend the head forward so that the chin touches the chest (due to significant tension in the neck muscles) and rigidity of the leg muscles: it is impossible to lift a straight leg by the heel (also due to severe tension in the leg muscles). These are signs of irritation of the meninges with blood, i.e. meningeal syndrome.
If a person regains consciousness, then his limbs turn out to be paralyzed: if on the right, then speech impairments are noted, if on the left, then the patient has severe mental disorders (does not know how old he is, where he is, does not recognize his loved ones, considers himself completely healthy and so on.).
With a hemorrhagic stroke in the brain stem, patients do not live for more than 2 days and die without regaining consciousness. With sub-arachnoid hemorrhage from an aneurysm, a catastrophe most often occurs after physical exertion: lifting weights, trying to break a stick over the knee, nervous stress, accompanied by a short-term rise in blood pressure.
Precursors and symptoms of stroke
A few days before the onset of a stroke, both men and women are likely to experience the following strange sensations:
- sudden drowsiness during the daytime during normal rest periods;
- spontaneous attacks of tachycardia or slowing of heart rate;
- severe dizziness in the absence of active movements and changes in body position;
- nosebleeds for no reason.
A stroke may be preceded by a transient ischemic attack: a sharp or increasing headache with disturbances in vision, hearing, coordination of movements and sensitivity of body parts. It usually lasts for several hours, then the state of health gradually returns to normal. The attack is caused by a passing disruption of the blood supply to the brain tissue. This process is similar to a stroke, but unlike it, a transient attack ends safely. Blood circulation is restored, and necrosis of the affected cells does not occur.
Common symptoms of a developing stroke:
- attack of unbearable headache;
- visual disturbances: changes in color perception, spots and darkened areas before the eyes, double vision, flickering of “midges”, narrowing of the field of vision;
- changes in coordination of movements and facial expressions: inability to walk normally, gesticulate, paralysis of the facial muscles on one side, numbness of the limbs;
- Severe nausea, abdominal cramps or single vomiting are also likely.
Sometimes patients mistake such attacks for migraines, severe fatigue, or the consequences of stress. Preferring to simply take a painkiller, rest and lie down, they often lose time to save themselves.
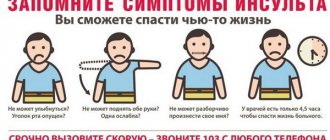
How to determine the onset of a stroke
It is impossible to distinguish a transient ischemic attack from an irreversible acute circulatory disorder without medical assistance. Both situations require hospitalization. Serious attacks can be identified using a simple test:
- The patient needs to symmetrically extend both arms forward, then alternately touch his nose with each palm. The inability to do this, sudden disturbances in the trajectory of movements, and a distorted body are signs of an attack.
- When looking in the mirror or at your interlocutor, you should smile broadly, stick out your tongue far, and say a few words. A possible stroke is indicated by distorted or paralyzed corners of the mouth, deviation of the tongue to the side, and slurred speech.
- You must try to write on paper or type any text on the keyboard. During a stroke, this is very difficult to do; the result is a meaningless set of letters.
One or more alarming symptoms is a reason to urgently call for medical help or go to the hospital. The first 3 hours after a stroke are most important for restoring blood circulation and preventing irreversible brain damage. A doctor is also necessary in cases where health has recovered on its own.
First aid for strokes
You should not try to give patients tea, coffee, water, try to give them food, give them a massage, or offer them medications that they have not taken before. Those suffering from chronic blood pressure disorders or heart disease can be offered their usual medications to prevent acute attacks of hypertension and arrhythmia.
Adequate measures that are important to take before the arrival of the medical team:
- Sit or help the patient lie down in a comfortable position, put a pillow, a cushion of clothing or a towel under the head.
- Unfasten the belts, loosen the collar, ties, unfasten the buttons on the neck and chest, freeing your breath.
- Provide fresh air flow by opening doors and windows in the room.
- Measure the victim's blood pressure and pulse.
In the absence of independent breathing and consciousness, it is allowed to perform an indirect cardiac massage by rhythmically pressing on the chest. But only if you have the necessary skills.