Symptoms of Myasthenia Gravis
Symptoms of myasthenia gravis are very diverse, which often leads to late diagnosis of the disease and erroneous diagnoses.
Drooping of the upper eyelid (ptosis)
Often the first manifestations of the disease are ptosis. It can be either one-sided or two-sided. May be asymmetrical and change throughout the day. More often in the morning and after rest it is less pronounced, and in the evening and after exercise it intensifies. Maybe on one side or the other.
Double vision can occur periodically when the condition worsens, or it can be constant when the disease is severe. It also intensifies with any physical activity, bright light, or heat. Decreases in the morning and after rest.
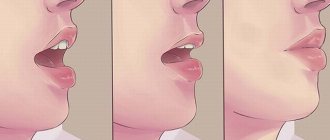
Weakness of the facial muscles is one of the most common symptoms of the disease. The muscles of the upper half of the face are most affected, which leads to difficulty closing their eyes; sometimes patients with severe disorders cannot even close their eyes completely. It can also be difficult to puff out your cheeks; facial expressions and smiles change. When trying to smile, only the upper lip rises, while the lower lip and the corners of the mouth remain motionless. There may be difficulty chewing, especially hard foods, and sometimes patients have to support their jaw with their hand while eating.
Impaired swallowing and changes in voice are also quite common symptoms; the voice becomes quiet, with a nasal tint, difficulties may arise when pronouncing the sounds “r”, “b”, “p”, “d” and “t”, choking occurs when taking food. The severity of symptoms can also change; they intensify during exercise and decrease after rest. Eating hot food often leads to a worsening of the condition. Severe disturbances can lead to changes in appetite and weight loss. And with severe lesions of the laryngeal muscles, patients speak almost in a whisper. Sometimes, when the condition worsens, it is necessary to resort to tube feeding if the patient cannot swallow on his own.
Weakness of the muscles of the neck and limbs are very common symptoms in the generalized form. Moreover, the muscle groups that are responsible for straightening the limbs suffer more. Weakness increases in the early stages with prolonged static load and repeated small movements (combing and styling hair, washing, knitting, working on a conveyor belt). In more severe cases of the disease, even with single movements. Patients may find it difficult to dress, wash, get up from a chair, and have difficulty climbing stairs. Weakness of the neck muscles can be so severe that the head hangs and it is difficult for the patient to lift it. Often, in severe cases, outside help is required.
Breathing disorders are the most formidable and dangerous symptom of myasthenia gravis. It is difficult for the patient to take a breath; there may be an accumulation of thick and viscous saliva, which is difficult to spit out and swallow. Shortness of breath can occur with exertion, and in more severe cases, at rest.
With myasthenia gravis, some patterns are observed:
- individual muscles are predominantly damaged;
- change in the severity of symptoms (all symptoms can vary greatly over several days, hours; the condition can worsen with exercise, menstruation, concomitant diseases, changing weather conditions);
- improvement of the condition after rest and taking medications that improve the conduction of nerve impulses.
Sometimes a patient's condition can suddenly deteriorate sharply - a crisis occurs. During a crisis, severe muscle weakness is observed, swallowing and breathing are impaired. This condition requires emergency care.
There are 3 types of crises: myasthenic, cholinergic and mixed.
Myasthenic - is essentially a pronounced increase in the symptoms of myasthenia. Movement disorders increase, and breathing disorders of varying severity are noted. This type of crisis develops with inadequate treatment of myasthenia gravis, insufficient doses of drugs, and excessive physical activity.
Cholinergic - associated with an overdose of drugs used in the treatment of the disease (Kalimin, proserin). It also manifests itself as increased muscle weakness, breathing problems, swallowing problems, and the formation of large amounts of liquid saliva.
Mixed - this type is most often encountered in practice, since when the condition worsens, patients independently increase the dose of drugs, which leads to their overdose and worsening of the condition. The symptoms are similar: a significant increase in muscle weakness, difficulty swallowing, and breathing.
To treat crises, plasmapheresis, glucocorticoids, and intravenous immunoglobulin are used.
Severe breathing disorders often require artificial ventilation, when the patient cannot breathe on his own, the machine does this for him.
In order to avoid such severe complications, it is very important to strictly follow the doses of medications prescribed by your doctor and the intervals between taking them.
Causes of the disease
Skeletal muscles begin to work when they receive a nerve impulse. The transmission of impulses from nerve to muscle occurs in a special formation called a synapse. The synapse has receptors to which acetylcholine attaches - this is a special substance that is released at the synapse when it receives a nerve impulse. The connection of acetylcholine with receptors serves as a signal for muscle contraction. This happens normally.
With myasthenia gravis, the number of active receptors is reduced, the muscle cannot work normally, and fatigue occurs. Damage and inactivation of receptors are caused by antibodies produced by the patient's immune system. Normally, the immune system produces antibodies to protect against foreign cells, but with myasthenia gravis this mechanism is disrupted, and instead of protecting, the immune system begins to attack its own tissues. The exact reasons for the malfunction of the immune system are still not known. Presumably the root cause may be infection, metabolic disorders, stress, pregnancy and childbirth, etc. Myasthenia gravis can be combined with other autoimmune diseases. Myasthenia gravis is not inherited.
Causes
Currently, doctors and scientists have not been able to find the exact cause of myasthenia gravis. Among the most common theories explaining the biomechanism of the development of the disease, the thymogenic one is popular. It is believed that antibodies are produced in the thymus (thymus gland). It plays an important role in the formation of children's immunity, but as they grow older, it undergoes reverse development up to complete atrophy. Many patients with myasthenia gravis have an enlarged thymus gland or a tumor in its tissue, which indicates a high probability of a connection between these pathologies.
There are a number of risk factors that increase the likelihood of developing myasthenia gravis:
- hereditary tendency;
- various genetic mutations;
- some types of infections (especially viral origin);
- acute or chronic stress;
- presence of other autoimmune diseases;
- tumors of internal organs (liver, kidneys, lungs, etc.);
- frequent physical overexertion;
- constant and prolonged exposure to high temperatures (for example, staying in a hot country);
- endocrine pathologies.
Forms of Myasthenia
There are different classifications of myasthenia gravis.
According to the type of flow, they are distinguished:
- Myasthenic episodes;
- Myasthenic conditions;
- Progressive;
- Malignant;
According to the prevalence of the process:
- Ocular, in which exclusively the eye muscles are affected.
- Bulbar - manifested by voice and swallowing disorders.
- Generalized, in which various muscle groups are affected and it, in turn, is divided into various forms: without bulbar disorders, with bulbar disorders, with breathing disorders.
By severity of violations:
- Lightweight;
- Moderate;
- Heavy;
Diagnostics
In making a diagnosis of myasthenia gravis, it is of great importance whether the patient has had episodes of weakness and fatigue in the past, which completely or partially resolved on their own or with nonspecific treatment. Most often, the eye muscles are affected - double vision occurs, the eyelids droop; facial muscles - facial expressions and smile change. Less commonly observed are problems with swallowing, voice, and weakness of the muscles of the limbs and neck.
The presence of a mediastinal tumor is also important, which is sometimes detected by chance during radiography, CT or MRI. Although the mere fact of the presence of a tumor does not confirm the diagnosis of myasthenia gravis. To make a diagnosis, a neurologist must conduct a full examination. Muscle strength, sensitivity, coordination of movements, swallowing, voice, etc. are assessed. Special tests are carried out to detect muscle fatigue. In mild cases, muscle weakness is detected when certain movements are repeated; in severe cases, the presence of weakness can be seen even without load.
Proserine test
One of the most important criteria for making a diagnosis is a test with Proserin. The drug is administered subcutaneously or intramuscularly in a dose of 1 ml to 2 ml, depending on the patient’s body weight. The result is assessed 40-90 minutes after administration of the drug.
Complete restoration of muscle strength is observed in a small number of patients; the majority experience incomplete improvement; this is regarded as a positive test. If there is a slight improvement, the test is considered doubtful, and if there is no effect, it is considered negative.
Blood analysis
All patients with suspected myasthenia gravis need to determine the level of antibodies to the acetylcholine receptor in the blood serum. To do this, blood is taken from a vein. This indicator is very important for making a diagnosis and assessing the effectiveness of treatment. Normally, the antibody level does not exceed 0.45 nmol/l. In specialized centers, antibodies to non-muscle-specific tyrosine kinase, titin and ryanodine receptors, which are often detected in the blood of patients with a thymus tumor, are also determined. But there are also seronegative forms, when antibodies are not detected in the blood
Electromyography
A very important method in diagnosing myasthenia gravis is electromyography, which detects disturbances in the conduction of impulses from nerve to muscle. The doctor places electrodes on the muscle and stimulates it with electrical impulses, this allows you to identify muscle fatigue.
The forms of myasthenia gravis are very diverse, so when conducting an examination of each patient, the doctor individually chooses which muscles to examine. The most affected muscle is selected. It makes no sense, for example, if eye movement is impaired, to examine the muscles of the arms. It is recommended to conduct the examination without taking medications, as the result may be unreliable. This examination method is often combined with a proserine test.
Computed or magnetic resonance imaging of the mediastinum
In the development of myasthenia gravis, the condition of the thymus gland plays a significant role; its enlargement or even tumors are often detected. Therefore, patients with myasthenia gravis are necessarily prescribed CT or MRI of the mediastinum.
In some cases, for a more accurate diagnosis, the level of thyroid hormones and glycosylated hemoglobin are examined. Since diseases of the thyroid gland and diabetes mellitus may cause symptoms resembling myasthenia gravis.
Symptoms
Muscle weakness caused by myasthenia gravis increases in sore muscles with repeated stress on those muscles. Since symptoms usually improve with rest, muscle weakness may come and go. Symptoms of myasthenia gravis progress over time and usually peak several years after the onset of the disease. Although myasthenia gravis can affect any of the striated muscles, certain muscle groups are involved more often than others.
Eye muscles
In more than half of patients who develop myasthenia gravis, the first symptoms are related to vision:
- Drooping of one or both eyelids (ptosis)
- double vision (diplopia), which may be horizontal or vertical
In approximately 15 percent of patients with myasthenia gravis, the first symptoms affect the muscles of the face and larynx and will include:
- Change in speech. Speech becomes quiet or through the nose, depending on which muscles are affected by the disease.
- Impaired swallowing. The patient can easily choke while eating food, water, or medications. In some cases, it is possible for water to come out of the nose while drinking water.
- Chewing disorder. The muscles involved in the chewing process may stop working during eating, especially when the load on these muscles is required (for example, chewing steak).
- Poor facial expressions. People around you may notice that the patient’s smile has disappeared and there is no facial reaction to emotions - this happens when the facial muscles are damaged.
Muscles of the limbs and neck
Myasthenia gravis can cause weakness in the neck, arms, and legs, but it usually occurs in conjunction with muscle weakness in other parts of the body, such as the eyes, face, or throat. The disease usually affects the arms more often than the legs. If the legs are involved, the gait becomes a waddle. If the neck is involved, then it is difficult for the patient to keep his head straight. Therefore, if symptoms appear, such as difficulty breathing, swallowing, weakness in the limbs, visual impairment, then you must consult a doctor.
Treatment of Myasthenia Gravis
Various drugs and treatment methods are used in the treatment of myasthenia gravis. The choice of therapy depends on the form and severity of the disease.
The use of drugs that block the cholinesterase enzyme (Proserin, Kalimin, Pyridostigmine bromide) is aimed at improving the conduction of impulses from the nerve to the muscle and, accordingly, reducing muscle weakness. Proserin lasts only 2-4 hours, so it is used for testing and in cases where a quick onset of action of the drug is necessary. Kalimin (Pyridostigmine bromide) begins to act only after 45-60 minutes, but the effect can last up to 6-8 hours. Therefore, kalimine is more often used for continuous use. The interval between doses of the drug should be at least 5-6 hours; more frequent use can lead to an overdose. An overdose is manifested by drooling, muscle twitching, dizziness, etc.
Doses of all drugs are selected individually in consultation with a doctor.
These drugs help to temporarily improve the condition, but do not act on the cause of the disease. Therefore, they are used in milder cases of the disease.
If the effect of taking Kalimin is insufficient or the condition worsens, especially in the presence of swallowing and breathing problems, drugs are prescribed that affect the functioning of the immune system and reduce the production of antibodies (glucocorticoids and cytostatics).
Glucocorticoids (Prednisolone, Methylprednisolone) are effective in most patients, so they are considered the most basic drugs in the treatment of severe forms with swallowing, breathing and ocular disorders. Their use allows you to achieve quick results.
The dose of the drug is selected individually, depending on the severity of the patient’s condition. On average it is 1 mg/(kg/day). The drug is taken once a day in the morning, daily or every other day. The effect is assessed after a few days. As the condition improves, the dose of prednisolone is gradually reduced to a maintenance dose, which sometimes has to be taken for a long time.
If the effect of hormonal drugs is insufficient or pronounced side effects are observed: increased blood pressure, blood sugar, ulcerative lesions of the stomach and intestines, etc., cytostatics (Azathioprine, Sandimmune, etc.). Doses of these drugs are selected individually under the control of a blood test.
Potassium preparations
Potassium is involved in the conduction of nerve impulses and helps improve the condition of patients with myasthenia gravis. potassium chloride powder or tablets, 1 g 3 times a day with meals. (Kalinor retard, Potassium normin, Kalipoz). To increase the level of potassium in the blood, potassium-sparing diuretics are also used: Spironolactone (Veroshpiron).
RADIATION THERAPY - usually given to elderly patients with serious underlying medical conditions for which surgery cannot be performed.
NON-SPECIFIC THERAPY is most often carried out in spring and autumn, when exacerbations usually occur, in courses of 2-3 months. Treatment helps improve the functioning of the nervous system and increase the body's resistance. It includes drug treatment and hardware methods (ILBI, blood ozonation, etc.), the full range of which is presented at the First Neurology clinic.
Treatment
Doctors use a variety of treatments, alone or in combination, to reduce the symptoms of myasthenia gravis.
Medications
- Cholinesterase inhibitors. Medicines such as pyridostigmine (Mestinon) improve communication between nerves and muscles. These drugs do not treat the cause of the disease, but they can improve muscle health and muscle strength. Possible side effects include gastrointestinal disturbances, increased salivation and watery eyes, and frequent urination.
- Corticosteroids. These drugs have a suppressive effect on the immune system, reducing the production of antibodies. But be aware that long-term use of corticosteroids can lead to serious side effects, such as thinning bones, weight gain, diabetes, an increased risk of certain infections, and an increase and redistribution of body fat.
- Immunosuppressants. Your doctor may also prescribe other drugs that suppress the immune system, such as azathioprine (Imuran), cyclosporine (Sandimmune, Neoral), or mycophenolate (Cellcepta). Side effects from immunosuppressant medications can be serious and may include an increased risk of infections, liver damage, infertility, and an increased risk of cancer.
- Plasmapheresis. This procedure uses a filtration process similar to dialysis. The blood passes through a machine that removes antibodies that block the transmission of signals from nerve endings to muscle receptors. However, the benefits of plasmapheresis usually only last a few weeks. Repeated procedures may result in difficulty accessing the vein, sometimes requiring catheterization into the subclavian vein. In addition, there is a risk of a drop in blood pressure after this procedure, as well as bleeding due to the use of anticoagulants during the procedure.
- Intravenous administration of immunoglobulin. This procedure provides the body with normal antibodies that reverse the compromised immune system response. This procedure has a lower risk of side effects than plasmapheresis and immune suppression therapy, but its effects may take a week or two to begin and last no more than 1 to 2 months. Side effects, which are usually mild, may include chills, dizziness, headache and swelling.
Surgery
15 percent of people who have myasthenia gravis also have a tumor in the thymus gland. In such cases, surgical treatment and tumor removal are recommended. For patients with myasthenia gravis who do not have a tumor in the thymus, removing the gland is a controversial treatment option.
Surgery is not recommended by most doctors if:
- Symptoms are mild
- Symptoms are related to the eyes only
- Age over 60 years
Lifestyle
- It is necessary to eat when there is good muscle strength. Meals should be taken in small portions and sticky foods should be avoided and preference should be given to soft foods. It is advisable to take breaks when chewing food.
- It is necessary to use precautions at home. Grab bars and railings should be installed in areas where support may be needed, such as near the bathtub.
- Use of electrical appliances and power tools. Where possible, conserve muscle strength and use electrical appliances
- It is necessary to plan things depending on muscle strength and, if necessary, resort to the help of other people.
Pregnancy with Myasthenia Gravis
Pregnancy with myasthenia gravis is not contraindicated. Patients with myasthenia gravis are able to safely carry a pregnancy to term. The only limitation for pregnancy with myasthenia gravis is an insufficiently compensated condition with severe symptoms.
In 1/3 of patients, deterioration of the condition may be observed, more often in the 1st trimester and the first month after childbirth.
Taking medications must be continued during pregnancy (Kalimin and Glucocorticoids). With the exception of cytostatics (Azathioprine, Sandimmune, etc.), pregnancy while taking them is undesirable.
It is advisable to plan pregnancy during the period of remission. During pregnancy, patients must be observed by a neurologist for timely correction of treatment.
Artificial termination of pregnancy in myasthenia gravis is contraindicated, as it almost always leads to an exacerbation of the disease.
Childbirth in the absence of obstetric indications, preferably through the natural birth canal. Sometimes during childbirth additional administration of Kalimin (Proserin) and Oxytocin is required. If there are indications for cesarean section, preference is given to epidural anesthesia.
20% of newborns may experience symptoms of myasthenia gravis, this is due to the transfer of antibodies from the mother. Symptoms: lethargy of the child, weak cry, ptosis, breathing problems, as a rule, can persist from 2 to 4 weeks and disappear as the antibodies are destroyed. This requires careful monitoring of the newborn, in some cases the use of drugs (Kalimina) is required.
Recommendations for a patient with Myasthenia gravis
Myasthenia gravis is a serious disease that requires increased attention and has many features and restrictions, which, if not observed, can easily provoke a deterioration of the condition.
With myasthenia gravis, significant physical activity and prolonged exposure to the sun are contraindicated. Deterioration can also be caused by staying in a sauna or steam room.
Many medications are contraindicated:
- Magnesium preparations;
- Curare-like muscle relaxants;
- Neuroleptics and tranquilizers (except tofisopam);
- Diuretics (except spironolactones);
- Many antibiotics: aminoglycosides (gentamicin, streptomycin, kanamycin, tobramycin, sisomycin, amikacin, etc.), fluoroquinolones (norfloxacin, ciprofloxacin, ofloxacin, etc.);
- Fluorinated corticosteroids (Dexamethasone, Dexazone, Polcortolone);
- Quinine derivatives;
- Penicillamine;
- B-blockers;
- Calcium channel blockers;
- Carbamazepine;
- Oral contraceptives;
- Narcotic analgesics.
Prevention
There is no specific prevention of the disease. Basic preventive measures are aimed primarily at people who already have myasthenia gravis and are aimed at preventing worsening. The following rules must be followed:
- provide complete and balanced nutrition;
- avoid heavy physical activity at home or at work;
- eliminate all bad habits: smoking, drinking alcohol;
- avoid exposure to ultraviolet radiation: avoid prolonged exposure to the open sun, use creams with a high SPF filter, wear closed clothing, do not visit solariums;
- eliminate stress and mental strain as much as possible;
- ensure yourself adequate sleep at least 8 hours a day;
- consult a doctor in a timely manner for any diseases, including infectious diseases;
- categorically exclude drugs containing magnesium.
Read also
Rehabilitation
Restoration of the body after diseases of the central and peripheral nervous system, operations on the brain and spinal cord, conditions after removal of the mammary gland due to a tumor, consequences...
Read more
Perinatal encephalopathy
Perinatal encephalopathy is a frequently encountered concept in the practice of pediatricians and pediatric neurologists! What it is? Literally, “perinatal encephalopathy” means “damage to the brain in the perinatal...
More details
Neurogenic bladder
In a healthy person, the process of urination is carried out in the form of a voluntary reflex act, and we can control it. However, this is not the case with this disease. Patients are extremely...
More details
Arnold-Chiari malformation
Due to the availability of the study and the high resolution of MRI, we quite often come across the conclusion - Arnold-Chiari anomaly. What is meant by this concept? Arnold-Chiari malformation...
More details
Sudden memory loss/transient global ischemia
Transient, that is, temporary memory loss occurs in elderly patients and people suffering from migraines. At the same time, memory for past and present events disappears. But the person is conscious, accessible...
More details
About the reasons
Currently, the causes of myasthenia gravis are not fully understood. Sometimes it is impossible to say unambiguously why a particular patient developed a disease. It is generally accepted that the following factors play a significant role:
- Family predisposition. Very often it turns out that the diagnosis of myasthenia gravis has already been made to the patient’s close relatives.
- Frequent stress, disorders in the immune system, the harmful effects of viruses, bacteria and other microorganisms. These factors “shatter” the immune system, and the body begins to synthesize antibodies against its own tissues, in particular, against the receptor proteins of the postsynaptic membrane. This leads to a delay in the transmission of signals from nerves to muscles, even blocking impulses.
- Myasthenia gravis can be a consequence of certain diseases. For example, when the thymus gland (thymus) grows, antibodies to synapse receptors also begin to be produced.
When malignant neoplasms appear in the ovaries, respiratory organs or mammary glands, they speak of Lambert-Eaton myasthenic syndrome. Muscle weakness, sometimes mistaken for myasthenia gravis, occurs with Charcot-Marie disease, dermatomyositis (destruction of connective tissue), various forms of myopathies, ALS syndrome (amyotrophic lateral sclerosis) and many other pathologies.
Soft tissue MRI
- Cost: 6,000 rub.
More details
The difficulty of diagnosis is that patients with myasthenia gravis at the onset of the disease may not have any clear complaints and symptoms. Neuroimaging (or MRI) shows no significant abnormalities in the structures of the central nervous system. Only in 30% of patients the thymus becomes enlarged or neoplasms are detected in it. When examined, the muscles are also not changed in any way; pathology can only be detected by microscopic examination.