What does an MRI of the brain look like?
A classic example of an MRI scan of the brain is shown in the pictures below. Magnetic resonance imaging is performed in the transverse (or axial - figure below) and longitudinal (or sagittal - figure above) planes.
The study is performed in several modes. The main ones are T1 and T2. Images obtained in these modes are often also called T1-weighted or T2-weighted images. The images shown above were taken in T1 mode.
The main difference between these modes is how liquid and air are displayed in the pictures. In T1 mode, tissues containing a large amount of water have a darker color, while in T2 mode they are bright, light. This is easy to understand by looking at the pictures above - the eyeballs are visualized in the form of light paired rounded formations; on one side they are bright and light, on the other - dark. Therefore, the picture on the right was taken in T1 mode, the picture on the left in T2. There is also a difference in how the gray matter of the brain is displayed in these modes. In T2 mode it is lighter than white matter.
In fact, there are many more modes - FLAIR, DWI, STIR and so on. One mode is used to suppress the signal from fat-rich tissues, another is used to study the distribution density of protons in tissues, and a third is used to evaluate the Brownian motion of water molecules. That is why a full course of MRI diagnostics for doctors lasts more than one month.
Symptoms
The set of symptoms depends on the location of the lesions and the depth of damage to the brain tissue. Symptoms:
- Pain syndrome. Characterized by chronic headaches. Unpleasant sensations intensify as the pathological process deepens.
- Rapid fatigue and exhaustion of mental processes. Concentration deteriorates, the volume of operative and long-term memory decreases. It is difficult to master new material.
- Flattening of emotions. Feelings lose their sharpness. Patients are indifferent to the world and lose interest in it. Previous sources of pleasure no longer bring joy and desire to engage in them.
- Sleep disturbance.
- In the frontal lobes, foci of gliosis disrupt the control of the patient’s own behavior. With deep violations, the concept of social norms may be lost. Behavior becomes provocative, unusual and strange.
- Epileptic manifestations. More often these are small convulsive seizures. Individual muscle groups contract involuntarily without threat to life.
White matter gliosis can manifest itself in children as a congenital pathology. The lesions cause dysfunction of the central nervous system: reflex activity is disrupted, vision and hearing deteriorate. Children develop slowly: they get on their feet late and begin to speak.
Normal and abnormalities on MRI of the brain
How do you know if there are signs of disease in the pictures? The most important thing is to remember what the brain of a healthy person looks like. The doctor, studying the photographs of patients, constantly compares them with normal photographs stored in his head. To understand how this happens, look at the pictures below:
Here are two pictures taken in the same mode. The photo below is normal. What disease, in this case, is in the top picture? To understand this, you need to compare these images. The difference is clearly visible - in the top image there is a tumor on the right side of the brain. The difference is even more noticeable if you compare the left and right sides of the same photo.
Let's mark it with a red circle. Visually, it is a node, heterogeneous in color and different from the gray and white matter of the brain. In such cases, in order to accurately determine the boundaries of the tumor and determine its type, the study is repeated with contrast. The introduction of a contrast agent into the blood through the cubital vein leads to the accumulation of the contrast agent in the tumor tissues - normal healthy tissues practically do not accumulate it. And we get the following picture, shown in the figure on the right. The bright color of the tumor corresponds to the accumulated contrast - now you can not only tell where the tumor is, but also roughly determine that it is a benign tumor, since it has clear boundaries (malignant tumors grow into surrounding tissues, which is why the boundaries will be blurred and not so clear ).
Thus, interpretation of the results of MRI of the brain is carried out by comparing the obtained images with the norm. If there are no differences, we can say that the patient whose images are examined by the doctor is most likely healthy. Everything is compared - shape, size of anatomical structures, localization, symmetry, amount of cerebrospinal fluid in the cavities of the brain, and many other parameters. Each disease, be it stroke or multiple sclerosis, has its own characteristic symptoms.
Diagnostics
Focal changes in the brain are difficult to diagnose in the initial stage. Detection of pathology is made difficult by the rather sparse symptoms.
Ultrasound diagnostics with Doppler sonography reveals abnormalities in the vessels of the brain (asymmetry, increased venous blood flow, stenosis, atherosclerosis). CT scan (computed tomography) determines previous heart attacks, accumulation of fluid in cavities and thinning of tissues (atrophy of brain structures).
The most reliable and accurate results can only be obtained by examining magnetic resonance imaging (MRI) of the skull. The image is obtained by interacting an electromagnetic field with hydrogen atoms.
This diagnosis allows you to evaluate the functioning of neurons and detect changes in the density of brain tissue. Having identified asymptomatic stages of focal lesions, it is possible to begin timely therapy.
MRI allows you to obtain images in three planes (transverse, longitudinal and frontal) and identify the cause of malnutrition of brain structures:
- Necrotic single lesion in the cerebral cortex, resulting from narrowing or closure of a spinal artery by a thrombus (congenital pathologies, the result of atherosclerosis or spinal hernia);
- Multiple focal lesions – pre-stroke condition (diagnosis allows timely treatment to begin and the development of irreversible processes to be prevented);
- Changes in the frontal or parietal lobe - small lesions that occur with hypertension and crises;
- Microfocal lesions - diagnosed by injection of a contrast agent, typical for older patients, or the presence of congenital anomalies.
The detected pathology using MRI allows one to assess the rate of disease progression and choose the right treatment tactics.
How to Read Brain MRI Results
Now let’s try to read the MRI report of the brain with a transcript of the images using the following example:
- Scanning technique – lists the modes in which the study was carried out;
- A series of tomograms reveal small foci of ischemia - areas of the white matter of the brain experiencing oxygen deficiency (age-related changes). Any focal changes, regardless of location, are pathology;
- The following describes the cerebral cortex - slight atrophy of the frontotemporal lobes is also an age-related change (the study was carried out in an elderly person);
- Then the system of the ventricles of the brain is described - the cavities in which cerebrospinal fluid circulates - if they are not dilated and have a normal shape, then everything is normal.
- The corpus callosum, cerebellum and brain stem are unchanged;
- Next comes a description of the pituitary gland - a gland located at the base of the brain (a slight flattening is possible normally), the area of the optic chiasm, the sinuses of the internal carotid artery - also without changes, since there is no asymmetry, their contours are clear and even;
- Then comes a description of the eyeballs and the contents of the orbits - without pathological signals, i.e. fine;
- The area of the cerebellopontine angle—the origin of the auditory or vestibulocochlear nerve responsible for hearing—is unchanged, the nerve is identified on both sides;
- The paranasal sinuses are described - there is a cyst in the right maxillary sinus - the remaining sinuses are normal, pneumatization is normal (contain air, not pus or liquid);
- Next comes a study of cerebral vessels or MR angiography - no changes in caliber, symmetry, no displacement or narrowing of the lumen - the norm. Slight narrowing is allowed;
- Then venography is performed - no changes and normal caliber - normal.
In conclusion, only pathological changes are identified - in this case, these are foci of ischemia, atrophy of the frontotemporal regions, and a maxillary sinus cyst. In general, the picture corresponds to the patient’s age – 65 years. MRI signs of vascular encephalopathy - the final diagnosis will be determined by the attending physician. Please note that normally the images show no changes, focal or diffuse (evenly distributed), cysts, tumors, neoplasms, or areas of pathological hyper or hypointensity of the signal. The anatomical formations have clear, even contours, are not displaced, and are symmetrical. The vessels are symmetrical, without signs of narrowing of the lumen, with normal course and caliber, the intraluminal signal (actually blood in the vessel) is homogeneous, which indicates the absence of blood clots in the lumen of the artery or vein.
In a similar way, images are deciphered and described in any clinic. However, the accuracy of the conclusion made depends on the qualifications of the MRI diagnostic physician.
Causes and signs of pathology
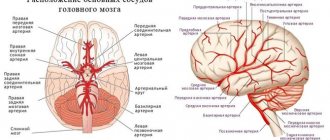
Nervous tissue is provided with intensive blood supply; a feature of perfusion in the brain is the bridges between the vessels. In case of emergency oxygen starvation, blood circulation is restored by another vessel.
Neurons are vulnerable even to a short-term lack of nutrition; cell death leads to irreversible processes in the brain - motor abilities and intelligence are impaired.
With age, blood vessels become less elastic and fragile. A common cause of damage to the cerebral cortex is concomitant diseases of the vascular system.
Reasons leading to defeat:
- Arterial hypertension;
- Vascular atherosclerosis;
- Hyperhomocysteinemia (high levels of homocysteine in the blood);
- Metabolic disorders;
- Inflammatory diseases of the meninges (leptomeningitis, pachymeningitis, arachnoiditis);
- Amloid angiopathy (amloid is deposited in the arteries);
- Multiple sclerosis;
- Damage to the cerebral cortex (trauma);
- HIV infection;
- Circulatory disorders (stroke, heart attack, dystrophic changes);
- Dyscirculatory changes (impaired blood circulation in the vessels of the skull, as well as in the spinal cord);
- Consequences of ischemia.
Brain tissue receives nutrition from the carotid and vertebrobasilar basins, interconnected in the velisian circle. In case of abnormalities or anatomically undeveloped vessels, there is no way to compensate for hypoxia by restoring blood flow through an anastomosis (connection with another vessel), which leads to focal damage to the brain of a vascular nature.
Symptoms of lesions of brain cells in the initial stage do not have a clear clinical picture, which leads to further destruction of axon bundles (white matter).
Clinical signs:
- Muscle spasms;
- Increased blood pressure;
- Dizziness;
- Mental disorders;
- Epileptic seizures;
- Migraine;
- Speech impairment;
- Decreased memory;
- Paralysis.
Causes
Damaged areas in the white matter are caused by the following diseases and conditions:
- Group of vascular diseases: atherosclerosis, amyloid angiopathy, diabetic microangiopathy, hyperhomocysteinemia.
- Inflammatory diseases: meningitis, encephalitis, multiple sclerosis, systemic lupus erythematosus, Sjogren's disease.
- Infections: Lyme disease, AIDS and HIV, multifocal leukoencephalopathy.
- Poisoning by substances and heavy metals: carbon monoxide, lead, mercury.
- Vitamin deficiency, especially B vitamins.
- Traumatic brain injuries: bruise, concussion.
- Acute and chronic radiation sickness.
- Congenital pathologies of the central nervous system.
- Acute cerebrovascular accident: ischemic and hemorrhagic stroke, cerebral infarction.
At-risk groups
Risk groups include people exposed to the following factors:
- Arterial hypertension. They are at increased risk of developing vascular lesions in the white matter.
- Poor nutrition. People who overeat, excessively consume extra carbohydrates. Their metabolism is disrupted, as a result of which fatty plaques are deposited on the inner walls of blood vessels.
- Foci of demyelination in the white matter appear in older people.
- Smoking and alcohol.
- Diabetes.
- Sedentary lifestyle.
- Genetic predisposition to vascular diseases and tumors.
- Constant hard physical labor.
- Lack of intellectual work.
- Living in conditions of air pollution.
Parieto-occipital dominance
The main characteristic of this group of disorders is parieto-occipital white matter lesions. These include X-linked adrenoleukodystrophy (ALD), Krabbe disease, early-onset peroxisomal disorders, and neonatal hypoglycemia.
Krabbe disease
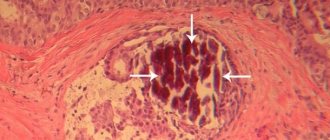
Krabbe disease is an autosomal recessive inherited disorder (lysosomal disorder) caused by deficiency of galactosylceramidase (chromosome 14q31), in which the accumulation of highly cytotoxic psychosine is thought to cause widespread demyelination. Large, multinucleated cells called "globoid cells" also appear. Depending on the age at which it appears, it is classified as an infantile, late infantile, adolescent, or adult-onset disease. Most cases are infantile and begin with the onset of fever, irritability, feeding difficulties, developmental delay, peripheral neuropathy, spasticity and optic atrophy at 3–6 months of age.
In the early stages, computed tomography (CT) reveals characteristic hyperdense areas in the thalamus and corona radiata. This is thought to reflect high density globud cells and glial proliferation.
MRI may also show T1 hyperintense and T2 hypointense MR signal around the ventricles, as well as linear structures similar to those seen in MLD (Figure 3). The dentate nucleus of the cerebellum, cerebellar white matter, and pyramidal tract of the brainstem show T2 hyperintense signal from an early stage.
Figure 3. Boy with Krabbe disease with cognitive dysfunction and motor impairment. CT scan revealed a hyperdense area (arrow) in the posterior limb of the internal capsule. On T1- and T2-weighted images, abnormal signals were seen in the posterior limb of the internal capsule (arrow), white matter at the posterior horn of the lateral ventricle, and splenium of the corpus callosum. The U-fibers were preserved (image courtesy of Professor Jiro ONO*, Faculty of Education, Wakayama University).
X-linked adrenoleodystrophy
X-linked adrenoleodystrophy (ALD) is an X-linked recessive inherited disorder (peroxisomal disorder) caused by an abnormality of the ABCD1 gene (chromosome Xq28). Impaired β-oxidation leads to the accumulation of very long-chain fatty acids in the cerebral white matter and adrenal glands, causing demyelination and adrenal failure. ALD is divided into childhood, adolescent and adult brain forms, adrenomyeloneuropathy (AMN) and Addison's disease.
Childhood brain disease develops between 5 and 8 years of age with the onset of symptoms including mental retardation, spastic gait, and visual and hearing impairment. Pathological demyelination develops from the white matter surrounding the lateral ventricles to the splenium of the corpus callosum, which gradually expands outwards.
MRI shows symmetrical T2 hyperintensities and T1 hyperintensities extending transversely from the white matter surrounding the trigone of the lateral ventricle, gradually widening and with accumulation of contrast at the edge (Fig. 4). Damage to the corticospinal tract is also evident.
Figure 4. School-age boy with X-linked adrenoleukodystrophy (ALD) presenting with movement disorders and visual impairment. White matter lesions are predominantly present in the occipital region.