Parkinson's disease mainly affects older people. The disease develops due to a lack of the neurotransmitter dopamine. It occurs in 120–180 people per 100 thousand population. The disease progresses steadily and leads to disability. Neurologists at the Yusupov Hospital use modern methods of treating Parkinson's disease, which can reduce the severity of symptoms and improve the quality of life of patients.
Initial manifestations of the disease
Between 5 and 10% of all cases of Parkinson's disease have a direct monogenic basis. Currently, more than fifteen genes for hereditary forms of primary parkinsonism have been identified.
The remaining cases are sporadic and occur under the influence of several factors. The sporadic form of the disease develops as a result of the influence of genetic and environmental factors. This determines the characteristics of cellular detoxification and xenobiotic metabolism, processing of a number of neuronal proteins, antioxidant protection, and the nature of dopamine metabolism.
An obligatory sign of the disease is hypokinesia, i.e. slowness, awkwardness of movements, impoverishment of the motor pattern, while muscle strength remains intact throughout the disease. The patient experiences some difficulties when performing the following basic everyday activities:
- tying shoelaces;
- fastening buttons
- shaving
- use of cutlery
- sticking one's hand into one's sleeve
- writing difficulties: handwriting becomes small (micrography)
- acheirokinesis: loss of friendly movement of the affected arm when walking
Doctors often encounter advanced stages of the disease in practice, because most people associate Parkinson’s disease with tremor, which is not at all necessary for Parkinson’s disease, while patients ignore other symptoms of the disease or attribute them to diseases of the joints or muscles.
Neurologists distinguish four components of akinesia:
- violation of motor initiative;
- violation of motor learning strategy;
- violation of the kinetic “melody”;
- When performing repeated tasks, there is a gradual attenuation of the amplitude of movements.
If tremor is present at the onset of the disease, then it is necessarily one-sided, like other signs of the disease; classic tremor in Parkinson’s disease is observed in a resting limb, intensifies when walking, but when performing movements of the affected limb, the tremor disappears. This type of tremor is not unique to Parkinson's disease, but its presence almost always indicates Parkinson's disease. It should be noted that Parkinson's disease never begins with a shaking head.
The following symptoms are characteristic of Parkinson's disease:
- hypokinesia;
- rest tremor;
- plastic muscle rigidity;
- postural instability.
Postural instability occurs at a more advanced stage of the disease.
Hypokinesia is detected clinically with a number of voluntary movements:
- the patient freezes in various positions, sometimes resembling a mannequin (not to be confused with true “freezes”, as complications of levodopa therapy);
- he has difficulty changing body position and initiating movement;
- there is no emotional coloring on the face (hypomimia), the patient rarely blinks;
- speech becomes monotonous, quiet, poorly modulated, gradually fading, and acquires a “tremor” character;
- hypophonia develops (decreased speech volume); bradyllia (slowness of speech), dysprosody (loss of melody in speech).
For early detection of hypokinesia, doctors at the Yusupov Hospital use the following tests:
- Fournier test. The patient is asked to perform a series of movements as quickly as possible: stand up, sit down, bend over, turn around, bend over. Slowness of movements is possible at the initial stage of hypokinesia;
- tapping test with thumb and index finger. The patient alternately taps on the table with both hands with the index and thumb at the maximum possible pace and with maximum amplitude. When hemiparkinsonism develops, one hand lags behind the pace and amplitude of the other hand, which is not yet involved in the disease;
- test of squeezing and unclenching the hand: the doctor asks the patient to clench and unclench the hand as quickly as possible (on the side of developing hypokinesia, the hand lags behind).
- Toe tap test
- Test with tapping the heel on the floor, in both cases an asymmetry of symptoms is visible.
Muscle rigidity, or plastic hypertonus, is a plastic increase in muscle tone. It increases in the initial phase of the movement and remains until the end of the movement. During a neurological examination, doctors often find the Negro phenomenon (the “gear wheel” symptom): against the background of plastic hypertonicity, a feeling of intermittency, step-by-step muscle resistance appears, and the tone increases with passive alternating movements.
Due to increased muscle tone, which predominates in the flexor muscles of the torso, the patient develops a peculiar “petitioner” pose: his head is lowered, his legs and arms are bent at the knee and elbow joints, and his feet take a parallel position to each other. By the way, forward tilt of the body, along with resting tremor and acheirokinesis, greatly facilitate the clinical diagnosis of Parkinson's disease. After raising the patient's head above the pillow, it remains in this position for some time. When performing the pendulum leg swing test, limb movements stop immediately after the test is completed.
Combined tests and questionnaires
In medicine, tests have been developed that allow one to identify several impaired mental functions at once. They consist of many tasks, each of which is responsible for memory, attention or thinking. The Mini-Cog test for Parkinson's disease has become widespread in clinical practice. At the beginning, the test taker is given 3 words that are not related to each other in meaning. The patient must then draw a clock face, place the numbers on it, and position the hands so that they show a specific time (for example, twenty minutes to four). After this, the test taker is asked to reproduce the words from the first task.
In clinical practice, another complex test is used - the Montreal Cognitive Function Assessment Questionnaire. It is used by psychiatrists to detect dementia due to Parkinson's disease. The test is considered difficult and requires 30-60 minutes to complete. It consists of several blocks and evaluates all higher brain functions of a person:
- abstract and spatial thinking;
- speed reaction;
- ability to remember and reproduce information;
- general level of intelligence;
- attention, its mobility and switchability;
- optical-spatial activity (the ability to determine the location, size, and distance of an object).
Important! The simplest and most informative method for identifying dementia in Parkinson's disease is the Mini-Cog test.
The test for Parkinson's disease consists of drawing a broken line, a three-dimensional object (cube, parallelepiped), or a clock dial with a given time. The questionnaire also contains arithmetic operations, reproduction of named words, naming numbers in reverse order, and simple logical tasks.
Non-motor manifestations of Parkinson's disease
Parkinson's disease has a whole range of non-motor manifestations that occur in all patients, regardless of the stage of the disease and age of onset:
- neuropsychiatric disorders (emotional, cognitive, behavioral, psychotic);
- sleep and wakefulness disorders;
- sensory disturbances (tingling, goosebumps) and pain;
- autonomic disorders (a very wide range of disorders among which the most maladaptive are frequent urge to urinate and orthostatic hypothesis, and the most common symptom is constipation);
- increased fatigue.
Before the onset of classic motor disorders in Parkinson's disease, non-motor manifestations may appear:
- constipation;
- impaired sense of smell;
- sleep disorders;
- pain syndromes.
In this regard, neurologists currently distinguish the preclinical, premotor stage of Parkinson's disease.
Parkinson's disease: a review of all the latest news
Alzheimer's disease and Parkinson's disease are perhaps the best known and most common diseases of the central nervous system. And their prevalence is steadily growing: after all, we are living longer, and the main risk factor in both cases is age. The fight against these diseases is going on with varying degrees of success. Nevertheless, the scales are tipping—slowly but surely—in favor of scientists.
Today I will tell you what medical news is available from the scientific fronts in the fight against Parkinson’s disease. All these “summaries” can be divided into three groups: the study of Parkinson’s disease, its early diagnosis and treatment. And to make it clear how actively this disease is being studied, I note: all this news happened over the past three (!) months.
News about the study of Parkinson's disease
1. Parkinson's symptoms are now being studied in primates.
Japanese researchers from Keio University in Tokyo have finally been able to produce large animal models of Parkinson's disease. It is usually studied in mice, but in order to develop drugs for humans, it is necessary to test its effect on animals that are more similar in physiology to Homo sapiens.
Scientists have genetically modified monkeys from the marmoset family by inserting into their genome a defective copy of the SNCA gene, which is associated with Parkinson's disease. As a result, from a very early age, the monkeys showed symptoms of the disease: in the first year of life they suffered from sleep disorders, in the second they observed deposits of Lewy bodies (pathological protein formations) in the neurons of the brain stem, and in the third they were already experiencing motor disturbances.
Moreover, when the unfortunate animals were prescribed the anti-Parkinsonian drug levodopa, their condition improved significantly.
2. The structure of alpha-synuclein has become clearer.
Biochemists from the University of Illinois, together with colleagues from the University of Pennsylvania, Vanderbilt University and Queen Mary University of London, have for the first time obtained a detailed structure of alpha-synuclein fibrils, a key protein in Parkinson's disease.
In this disease, alpha-synuclein molecules form long fibrils that disrupt brain function. This is somewhat similar to amyloid plaques in Alzheimer's disease, but the structure of synuclein fibrils remained unclear due to its complexity until recently. Now neuroscientists have become clearer about how these objects that cause the death of neurons are formed and how they can be dealt with.
News about disease diagnosis
1. The psychological characteristics of the patients were discovered.
A team of UCLA neurologists has found that a decision-making process can be used to diagnose Parkinson's disease at a very early stage.
They found that people with early Parkinson's disease have difficulty making perceptual (sensory) decision-making when sensory information is weak and they need to rely on earlier experiences.
Based on these data, neurologists plan to identify a special “label” that could form the basis of a diagnostic test.
2. Biomarkers in the blood were identified.
Scientists from the German Center for Neurodegenerative Diseases, as well as from the Hertie Institute for Clinical Brain Research and the University of Tübingen, have discovered proteins (small protein fibers, the so-called neurofilaments, to be precise), the presence of which in the blood and cerebrospinal fluid (cerebrospinal fluid) reflects the degree of degradation of nerve cells. At least, in experiments on mice with models of Parkinson's and Alzheimer's diseases, it was possible to diagnose the degree of disease progression based on the concentration of these filaments.
Such an analysis will be required not so much to diagnose the disease itself, but to monitor the effectiveness of treatment with a particular drug.
3. Possible reasons for late diagnosis were found.
Scientists from the School of Medicine at the University of Texas Health Science Center have found that a person can live, walk, and not know that Parkinson's disease is already developing in his brain for almost two decades. As a result, the first symptoms appear only when the disease is actively developing and time may be lost.
However, this has only been proven for mice and extrapolated to humans. In mice, it took 14 weeks from the onset of problems with neurons in the substantia nigra to symptoms. On the other hand, you wouldn’t cut into pieces the brain of a healthy person just to find out such news?
News about therapy
1. Singing helps with Parkinson's.
Doctors from three hospitals - Guy's, St Thomas' and St Helier's - in London carried out a systematic review of published evidence on the beneficial effects of singing on people with Parkinson's disease. The review has two main goals - to stimulate further high-quality research in this area and to draw the attention of clinicians to the therapeutic opportunities offered by such a simple leisure activity as singing.
There is a positive trend in the review, but the authors suggest conducting more thorough research into how singing improves the functioning of the speech apparatus of patients.
2. The first drug against hallucinations was created.
Parkinson's disease requires treatment not only for the underlying problem, but also for the associated effects. For example, hallucinations and illusions that often occur with this disease. And this year, the FDA registered the first ever drug to treat similar symptoms of Parkinson's disease. The drug is called Nuplazid (pimavanserin) and is available in tablets.
3. Donor neurons will be replaced with their own cells.
It is well known that Parkinson's disease usually affects the so-called substantia nigra, or substantia nigra, which contains neurons that produce dopamine.
Attempts have long been made to transplant neurons into the substantia nigra instead of dead ones. Not long ago, an amazing result was published: the transplanted nerve cells lived and supplied the substantia nigra with dopamine for a quarter of a century.
But all this is a transplant of donor neurons. Now scientists have gone further: they decided to grow new neurons for transplantation from the patient’s own cells. In a number of countries, including Russia, similar work is already underway. Skin cells are taken from the patient, then they are turned into stem cells, which in turn differentiate into dopaminergic neurons. Experiments on transplanting such neurons will take place very soon.
Alexey Paevsky
Photo istockphoto.com
3. Diagnosis of Parkinson's disease
To diagnose Parkinson's disease, your doctor will ask questions about your symptoms, existing health problems, and perform a neurological examination. A neurological examination includes specific questions and tests that will show how well your nerves are functioning. For example, the doctor will watch how you move, check muscle strength and reflexes, and vision. In some cases, special medications may be recommended. And the result of how the medicine works will help accurately diagnose the disease.
Laboratory tests and analyzes
will not help diagnose Parkinson's disease, but they will help rule out other diseases that may cause symptoms similar to Parkinson's disease. An MRI procedure is prescribed to detect signs of a stroke or brain tumor.
About our clinic Chistye Prudy metro station Medintercom page!
Treatment of pathology
Treatment strategies for Parkinson's disease depend on the stage at which the patient begins receiving the necessary therapy. For this reason, neurologists prefer to separate therapeutic approaches aimed at relieving early and late symptoms.
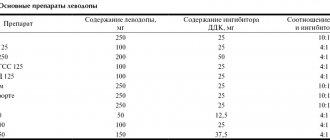
Treatment in the early stages involves the use of medications that stimulate the synthesis of dopamine in the brain. The therapeutic effect is achieved by stimulating dopamine releases and blocking reuptake. Thanks to this, it is possible to reduce the rate of neuronal death. Basic drugs can be used as part of complex treatment or as monotherapy. The combination of necessary substances is selected by a neurologist based on the clinical picture of parkinsonism and the individual characteristics of the patients.
Treatment of Parkinson's disease in the later stages remains an inevitable stage, since drug therapy can only slow down destructive processes. Progressive pathology is complemented by new symptoms that are difficult to relieve. At a certain point, the usual effectiveness of medications decreases. The patient experiences hypersensitivity of dopamine receptors and a kind of withdrawal syndrome due to the body's resistance to substances taken for a long time.
Against this background, doctors are forced to prescribe constantly increasing doses of medications to patients by reducing the intervals between doses. An alternative solution is to switch to a combination treatment regimen, which uses drugs from several groups. In some cases, surgery may be possible to implant an electrode into the patient that provides deep brain stimulation. This method allows you to stop resting tremor and restore motor activity in people suffering from Parkinson's disease.
Detailed description of the study
Parkinson's disease is a slowly developing brain disease associated with the destruction of the structures responsible for the production of dopamine. This provokes the development of various movement disorders, including:
- Rest tremor - trembling of some parts of the body in a calm state;
- Muscle stiffness;
- Slowing down movements;
- Gait disturbance;
- The emergence of pathological postures.
As a rule, the disease manifests itself after 60 years. Men get sick somewhat more often than women.
There are primary, or idiopathic, and secondary, or symptomatic, parkinsonism, which can occur due to the use of certain medications, as a result of injury, and also as a consequence of encephalitis.
Specific to parkinsonian disorders is reduced activity of the dopaminergic system. Normally, the structures of this system carry out the synthesis of dopamine, one of the main inhibitory transmitters of the central nervous system (CNS). This important neurotransmitter is formed through sequential enzymatic transformations: phenylalanine → tyrosine → L-DOPA → dopamine, which is stored in neurons of the brain and, as needed, transported to synapses - the sites of neuronal binding - for the transmission of nerve impulses.
After dopamine is released from neurons into synapses, approximately 80% of it is returned back, and the remaining small part is lost its biological properties with the help of the enzymes monoamine oxidase-B (MAO-B) and catechol-O-methyltransferase (COMT).
Insufficient formation of dopamine leads to an imbalance of other CNS neurotransmitters (glutamate, acetylcholine, etc.), which provokes specific motor disorders. The activity of the dopaminergic system of the central nervous system decreases with age in almost all people, but in some cases it reaches the stage of clinically pronounced disorders, and the person develops parkinsonism.
It is known that the central nervous system adapts well to a slight dopamine deficiency, and clinical signs of parkinsonism appear only with a loss of at least 70% of dopamine, i.e. with major changes.
In approximately 20% of cases, Parkinson's disease is familial - hereditary forms of the disease are noted. As a rule, the development of hereditary forms of parkinsonism is associated with mutations in the SNCA, LRRK2, and PRKN genes. Genetic mutations provoke the destruction of cells in the substantia nigra of the brain. These cells are responsible for the production of dopamine.
The SNCA gene encodes the α-synuclein protein, which is the main component of Lewy bodies (pathological protein formations in neurons). The gene mutation provokes the accumulation of insoluble protein formations in the cell and the subsequent death of neurons.
The LRRK2 gene encodes the protein dardarin, which is found in the cell nucleus and also in Lewy bodies. When the gene mutates, the level of dardarin increases significantly, which also provokes the death of neurons.
The PRKN gene encodes the parkin protein, which is found in the nuclei of brain cells. Parkin destroys abnormal proteins in brain cells. Due to the mutation, its functions are impaired, which leads to the accumulation of abnormal proteins and the death of neurons.
The diagnosis is made in the presence of characteristic clinical manifestations of Parkinson's disease, as well as if the pathology is diagnosed in blood relatives. Genetic testing allows you to confirm a previously made diagnosis.