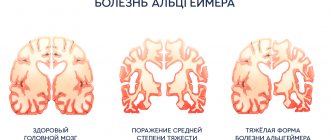
Alzheimer's disease is a pathology with neurodegenerative disorders in the brain. As the disease progresses, patients' intellectual abilities deteriorate, memory is impaired, and self-care skills are lost. Naturally, patients and their families are primarily interested in the question: is there a cure for Alzheimer's disease? However, modern science cannot yet give a positive answer. Alzheimer's disease is treated with drugs that can only slow down the pathological process, but do not eliminate it completely. New drugs are constantly being developed to treat Alzheimer's, but they cannot yet completely eliminate the disease. The Yusupov Hospital uses the most modern methods of treating Alzheimer's disease, which normalize the patient's condition and improve his quality of life.
Symptoms of Alzheimer's disease
The disease most often occurs in old age. But its development can begin from 40 to 60 years. In most cases, I diagnose it when the signs of pathology have already become obvious, which significantly complicates the treatment of the disease and worsens the prognosis. This is due to the fact that the first signs of pathology are ignored, and in the meantime the disease progresses. The sooner medications for Alzheimer's disease are started, the greater the chance of maintaining the patient's mental clarity for a long time.
The first sign of developing Alzheimer's disease is memory loss. Typically, short-term memory suffers when the patient cannot remember recent events. At the same time, the events of bygone days are remembered very well.
Another sign of the disease is periodically inappropriate behavior of the patient. This can manifest itself as unreasonable aggression, increased irritability, and inappropriate fun. Human activity decreases and interest in the world around us disappears. A person has difficulty perceiving information, and speech impairment occurs.
As the disease progresses, the severity of clinical manifestations increases. It is recommended to start taking Alzheimer's medicine at an early stage to slow down neurodegenerative processes. Drugs for the treatment of Alzheimer's help stop the development of pathologies and improve the patient's condition.
The creation of drugs for the treatment of neurodegenerative diseases is one of the most difficult problems of modern medicinal chemistry. In Fig. Table 1 provides comparative estimates of risks and costs in the development of drugs for the treatment of diseases of the central nervous system. At the same time, the social and financial significance of their creation exceeds any possible risks and development costs. So, in the USA in 2010-2011. The economic cost of Alzheimer's disease (AD) exceeded $215 billion [1]. According to the Alzheimer's Disease Therapeutics and Diagnostics: World Market 2013-2023 report, global sales of drugs for the treatment of AD could reach $8.3 billion by 2021.
Rice. 1. Comparative assessments of the risks and costs of drugs for the treatment of diseases of the central nervous system. 1 — probability of a drug entering the market for the treatment of diseases, %; 2 — time before obtaining permission to use, years; 3 — duration of the 2nd and 3rd phases of testing, years; 4 — probability of success in the 3rd phase, %; 5 - number of patients in trials; 6 — approximate cost of development (according to [1]).
According to J. Cummings et al. [2], during the period 2002-2012. 413 clinical trials were conducted on 244 drugs proposed for the treatment of AD, including 124 phase 1 trials, 206 phase 2 trials, and 83 phase 3 trials. Specifically, since 2007, when the US Food and Drug Agency (FDA) mandated clinical trial registration, 54 phase 3 trials have been conducted. However, despite the enormous efforts and financial expenditures aimed at finding effective drugs for the treatment of AD, not a single new drug has been brought to market over the past 11 years.
To date, four drugs are most actively used in clinical practice: donepezil (Aricept), galantamine (Reminyl), rivastigmine (Exelon) and memantine (Noogerone). The first three are acetylcholinesterase inhibitors.
According to modern concepts, AD is a proteinopathy that develops as a result of impaired metabolism of amyloid precursor protein (APP) and tau protein [3]. Soluble oligomers and aggregation intermediates are most toxic to nerve cells, whereas the final aggregation products are relatively inert. This is typical for both β-amyloid and tau protein [4]. Development of B.A. is a multifactorial process in which dozens of molecular entities take part, which determines a wide selection of targets for the design of potential drugs [5]. In recent years, dozens of reviews have been published analyzing various aspects of the pathogenesis and pharmacotherapy of AD and other dementias.
First-generation cholinesterase inhibitors (ChEIs), such as tacrine (approved for use since 1993), nonselectively inhibited AChE with respect to another enzyme of this group, butyrylcholinesterase (BuChE), and showed low organ specificity. Currently, they are practically not used.
One of the approaches used to improve the tolerability of drugs of the class of ChEIs involved increasing the selectivity of AChE inhibition in relation to BuChE, which was supposed to reduce the peripheral toxicity of these compounds. This principle was implemented in the development of second-generation AChE drugs, such as Aricept (approved for use since 1996) and galantamine (since 2001), which exhibit pronounced selectivity towards AChE. Another approach, successfully implemented, was implemented when creating the drug rivastigmine (since 1998). It consists of creating substances with pronounced region selectivity, providing selective inhibition of brain AChE in comparison with peripheral forms of cholinesterases. These drugs are significantly better tolerated than tacrine and show some effectiveness in the early and moderate stages of AD. In addition to the anticholinergic effect, they affect the processing of the APP protein and may have some promise in terms of slowing the development of neurodegenerative processes in AD [6]. On the other hand, ChEIs can often lead to increased levels of phosphorylated tau protein [7], potentially reducing their therapeutic appeal.
The last drug brought to market for the treatment of moderate and severe forms of AD in 2003 was the drug memantine, which is a non-competitive low-affinity blocker of the intrachannel site of the NMDA subtype of glutamate receptors. It was originally thought that its cognitive-stimulating properties were achieved by improving the signal-to-noise ratio of glutamatergic nerve impulse transmission due to optimal voltage-dependent blockade of the intrachannel site of NMDA receptors in the brain. The results of recent studies have suggested that the therapeutic effect of memantine is associated with the ability to block the toxic effect of β-amyloid peptide, which is realized with the participation of NMDA receptors in the brain [8].
In recent years, the strategy for finding drugs for the treatment of AD has changed significantly.
In order to identify the main trends and targets in the search for new drugs for the treatment of AD, we analyzed data on drugs that were in various phases of clinical trials. The data presented in this review are taken from the Thomson Reuters Intergrity database and information posted on the public website www.clinicaltrials.gov, which registers ongoing clinical trials since 2000.
At the end of October 2015, 51 drugs were in phase 1 clinical trials. Based on their mechanism of action, they were divided into several groups.
Vaccines - 9 drugs. At the same time, 5 drugs acted on β-amyloid (without specifying the form of amyloid), in particular drugs based on monoclonal antibodies SAR-228810 (Sanofi) [9], MEDI-1814 (AstraZeneca) [10], and the drug KHK- 6640 (“Kyowa Hakko Kirin”) [11] and 2 drugs based on recombinant hybrid proteins: Lu-AF-20513 (“Lundbeck”) [12] and TTP-4000 (“Trans Tech Pharma”) [11]. 4 drugs acted on tau aggregates: RG-7345 (Genetech) [13], BMS-986168 (Bristol-MyersSquibb) [11], AADvac-1 (Axon Neurosci) [14], ACI-35 (“ACImmune”) [15].
8 drugs were declared as substances that act on the formation of key pathomorphological formations characteristic of AD - amyloid plaques and neurofibrillary tangles. The drug SAN-61 (Diamedica) [11], which stimulates the proliferation of stem cells, simultaneously acted on amyloid plaques and neurofibrillary formations. The drug Exebryl (ProteoTech) also has a similar effect [16], but there is no data on its further development. The drugs ARC-29 [17], ARC-031 [18] (Archer Pharmaceuticals) and ALZT-OP1 (AZ Therapeutics) [19] prevented aggregation and reduced the level of the soluble form of amyloid, and ALZ-801 (Alzheon) ) [20] was a "prodrug" form of the anti-amyloid agent tramiprosate. The drug Ro-63−8695 (GlaxoSmithKline) [21] is characterized as reducing amyloidosis in the brain. The drug TPI-287 [22] was a stabilizer of microtubular structures.
2 drugs acted as inhibitors of APP protein proteolysis enzymes, with BI-1181181 (Boehringer Inhelheim) [23] being a β-secretase (BACE-1) inhibitor, and BMS-932481 (Bristol-Myers Squibb) [24] - γ-secretase.
The neurotrophic type of action is indicated for several drugs: FGL-2 [25], FGL-lop peptide [26] (“Enkam”) were high-molecular stimulators of fibroblast growth factors, and NsG-0202 (“NsGene”) [27] stimulated the secretion of growth factor nerves.
Trials have begun on the high molecular weight drug Copaxone, which belongs to the class of immunomodulators and was previously used to treat multiple sclerosis [28].
Work continues, although less actively, in the search for cholinesterase inhibitors. In particular, a specific inhibitor of butyrylcholinesterase (bisnorcymserine, QR Pharma) [29] and a non-selective inhibitor of butyryl and acetylcholinesterase, the drug memogain (GLN-1062, Neurodyn Life Sci) [30], which is a derivative of a well-known drug for the treatment of AD, are being tested - galantamine.
Compounds that modulate the activity of nerve cell receptors have attracted considerable attention. Substances of this type are often considered “signal modulating” drugs. Thus, two compounds that are antagonists of the 6th serotonin receptor subtype are being tested: AVN-322 (“Avineuro”) [31] and a drug with a pronounced multitarget effect PR-5063 (“Reviva Pharma”) [11], which also acts on 1st and 7th subtypes of serotonin and D3-dopamine receptors. The histamine receptor type 3 is the target of the drug SUVN-G3031 (Suven Life Sci) [11], and the GABA-A receptor is the target of the inverse agonist RG-1662 (Basmisanil, Roche) [11]. The drug CX-1632 (“Cortex”) [11] is a positive modulator of the AMPA receptor, which plays a key role in the processes of memory consolidation. The action of the drug AUS-131 (S-Equol, Ausio Pharm) [32], which is an agonist of estrogen receptors, is aimed at increasing the functional activity of brain mitochondria. The drug telmisartan [33], known as a treatment for hypertension, is undergoing phase 1 trials in patients with asthma.
Several drugs are inhibitors of enzymes involved in the pathogenesis of AD: two compounds inhibit 11-β-hydroxysteroid dehydrogenase type 1 - drugs UE-2343 (Actinogen) [11] and ASP-3662 (Astellas Pharma) [19] , the drug GSK-2647544 (GlaxoSmithKline) [19] blocks the activity of phospholipase A2. is developing a group of drugs based on histone deacetylase inhibitors; in particular, EVP-0344 [11] is being tested in phase 1 in patients with asthma. At the end of 2021, phase 1 clinical trials of the low molecular weight heteroaryl derivative BPN14770, which is a negative allosteric modulator of phosphodiesterase PDE4D, began [34].
Testing of drugs that can be classified as anti-inflammatory agents by their type of action is ongoing: the compound AAD-2004 (GNT Pharma) [35], which is an inhibitor of cytokine formation, and the substance GC-021109 (GliaCure) [19], which acts as phagocytosis inducer.
Several drugs are claimed to be antioxidants with a multitarget mechanism of action. These include the dietary supplement Lu-AF-2053 (Lundbeck) [36], the Etenercept complex (Life Extension Found) [37], including curcumin, quercetin, fish oil and a number of other ingredients, plant extract - HX- 106 [38].
For 9 drugs in phase 1 clinical trials, the mechanism of action is not specified and the structures are not disclosed.
At the end of October 2015, data were available on 59 drugs in phase 2 clinical trials. Based on their mechanism of action, they were divided into several groups.
6 drugs are vaccines acting on β-amyloid formations. In particular, , which has developed the technology for creating “affytopes” (specific antibodies to shortened fragments of antigens that do not cause side autoimmune effects), is testing the drug AD-04 [39], which acts on β-amyloid peptides. Previously, this company conducted phase 2 trials of another vaccine, AD-02 [19], which selectively acted on Aβ-40-42 peptides, but at the moment there is no data on the further development of this drug. ACI-24 (“AC Immune”) [40] is an oligospecific vaccine developed using liposomal technology. The drug BAN-2401 (“Eisai”) [41] is a new group of monoclonal antibodies that selectively neutralize and remove soluble protofibrils and β-amyloid aggregates. In September 2015, trials of the UB-311 vaccine [42, 19], which combines the N-terminal fragment of β-amyloid peptide 1-14 with a T-helper epitope, began.
After the successful results of the 3rd phase of trials of the vaccine drug solanezumab [43], a number of developments, work on which had been suspended, were returned to clinical trials. Thus, the drug crenezumab (AC Immune and Genetech) [44], which is a humanized monoclonal antibody IgG4kappa acting on both the soluble and aggregated form of β-amyloid, initially did not pass the 2nd phase of clinical trials, but then again returned to phase 1, but using higher doses. Since September 2015, this drug has been in phase 2 trials. The drug ponezumab (PN-1219, Pfizer) [45], which is a humanized monoclonal antibody IgG2kappa, has not passed phase 2 clinical trials in the treatment of patients with AD, but is currently in phase 2 trials in the treatment of patients with cerebral angiopathy.
Several small-molecule compounds can be classified into the general group of “anti-amyloidogenic” drugs. In 2015, trials for AD and mild cognitive impairment (MCI) of the drug posipen (QR Pharma) [46], which is a (+)-isomer of phenserine, which showed in preclinical studies the ability to reduce the level of β-amyloid and APP protein, were stopped. conducted phase 2 trials of the drug scyllo-inositol (ELND005) [47] in patients with B.A. In preclinical studies, it was found that it blocks the aggregation of β-amyloid peptide, reducing the concentration of its toxic forms. The main positive effect is associated with a decrease in agitation in B.A. Clinical trial results are mixed [11].
There is data on 2 drugs that act on the enzymes involved in the formation of β-amyloid peptide: drugs E-2609 (“Eisai”) [48], a β-secretase inhibitor (BACE-1), and EVP-0962 (“Eisai”) are under active development. FORUM Pharm") [19] is an orally acting γ-secretase modulator (inhibitor), which is also undergoing phase 2 clinical trials in patients with mild cognitive impairment.
The group of drugs with a neurotrophic effect includes T-817MA (Toyama FujiFilm) [49] - it stimulates neurite growth and exhibits a neuroprotective effect, reducing oxidative stress in brain tissue. The short oligopeptide davunetide (“Paladin”) [50], containing 8 amino acid residues, is the minimal active fragment of the neuroprotective protein ADPN, which is involved in the implementation of neuroprotection induced by the vasoactive peptide VIP; it is being tested in phase 2 on a number of nosologies associated with tau- pathy, including dementia of the frontotemporal and Alzheimer's type. is conducting phase ½ clinical trials of the drug neurosteam-AD [19, 51] based on mesenchymal stem cells. Gene therapy has been used to create CERE-110 [52], which delivers nerve growth factor (NGF) genes. The product has passed the 1st phase and has been transferred to the 2nd phase, but there is no data on the test results.
A significant number of drugs in phase 2 clinical trials belong to the group of “signal modulating” agents that act at the level of synaptic signal transmission. They mainly act on enzymes and receptors, as well as mechanisms regulating the level of second messengers.
Thus, the drug ABT-126 (“AbbVie”) [53], which is an agonist of α-7-nicotinic receptors, is undergoing long-term trials in combination with AChE inhibitors. The drug isproniciline (AZD-3480, Targacept) [54] is an α-4-β-2-nicotinic receptor agonist. However, data on the results of its tests have not been published.
3 drugs are antagonists of the 6th subtype of serotonin receptors: PF-05212377 (Pfizer) [55], SUNV-502 (Suven Life Sci) [19] and SB-742457 [56], which is testing it against the background donepezil treatment. The drug S-38093 (Servier) [11] is characterized as a specific antagonist of H3-histamine receptors, and ORM-12741 (Orion) [57] - of α-2C adrenergic receptors.
PXT-864 (“Pharnext”) [58] is a fixed-dose combination of baclofen and acamprosate. It has a pronounced multi-target effect, also acting as a GABA-B receptor agonist, an NMDA receptor antagonist, and a modulator of metabotropic glutamate receptors. The drug AN2/AVex-73 (Anavex Life Science) [59] blocks sodium channels, is a σ-1-opioid receptor agonist, an M1-muscarinic receptor agonist, and an acetylcholinesterase inhibitor. Its combination with donepezil is also undergoing phase 2 clinical trials. In September 2015, phase 2 trials of the drug dexpramipexole (Biogen) [60], previously proposed for the treatment of amyotrophic lateral sclerosis (ALS), were expected to be completed. The compound is a stereoisomer of the dopamine receptor agonist pramipexole [61].
In recent years, the specifically designed multitarget drug lagostigil (“Avraham”), which acts as an inhibitor of cholinesterases and monoamine oxidase, types A and B, has been actively discussed. It showed good results in phase 2 clinical trials, but failed phase 3 and is currently in phase 2 clinical trials in patients with MCI [62]. Research is underway on the specific MAO-B inhibitor rasagiline [63], proposed for the treatment of some forms of parkinsonism. is testing another MAO-B inhibitor, the drug RO-4602522 [64], in the treatment of patients who had previously undergone courses of therapy with cholinesterase inhibitors or memantine (its trial was discontinued at the end of 2015). Inhibition of phospholipase A2 is stated as the main mechanism of action of the drug rilapladib (SB-659032, GlaxoSmithKline) [65]. Its clinical trials for AD were completed in 2015, but the results are not yet available.
Glutaminyl cyclase is the main target of the drug PQ-912 [11], and phosphodiesterase 9A is the main target of the drug BI-409306 [66] from Boehringer Ingelheim. The drug bryostatin 1 (“Blanchette Rockefeller Neurosci Inst”) [67], which is an activator of protein kinase C (PKC), has been submitted for phase 2 trials in patients with moderate to severe forms of BA. Phase 2 clinical trials have begun for the treatment of patients with AD and MCI with the anti-inflammatory agent VX-745 [68], which acts as an inhibitor of p38 MAPK (mitogen-activated protein kinase p38), an enzyme involved in inflammatory processes involving glial cells.
N-type calcium channels are the target of action of the well-known anticonvulsant drug levetiracetam (AgeneBio) [69], which is being tested for mild cognitive impairment associated with the development of AD.
The drug riluzole (Rockefeller Univ) [70], used for the treatment of ALS, is in phase 2 clinical trials. The mechanism of its action is multitarget and includes a group of targets of the glutamatergic system of the central nervous system and a number of ion channels. A drug for the treatment of neutropenia and prostate cancer, sargramostim (leukine) (University of Colorado) [71], which acts as a granulocyte-macrophage-stimulating agent, is also in phase 2 clinical trials.
Phase 2 trials for asthma included 25 drugs that had previously been used for other purposes. These include two multi-target drugs, the action of which has a pronounced antioxidant component, well known from previous applications. This is the antioxidant resveratrol [72], which also acts on MAO-A, β-secretase, xanthine oxidase, NF-kappaB and a number of others. The drug underwent phase 2 clinical trials in patients with asthma, was withdrawn from phase 3, and is currently being tested in combination with other drugs in MCI. The herbal drug curcumin [73] has been repeatedly studied in clinical trials for AD, but no reliable positive results were obtained. In 2015, its trials continued (University of California, Los Angeles) at MCI.
The drug enbrel (“Neurokine”) [74], a recombinant protein that is a TNF-α agonist and has been used as an anti-inflammatory agent for the treatment of rheumatoid arthritis, is also being studied.
An analogue of vitamin B1, benfotiamine (Burke Med Res Inst) [75], is also undergoing clinical trials, used as a prodrug as a broad-spectrum neuroprotector for neuropathies, neuralgia, coronary circulatory disorders, etc.
In recent years, the oncolytic agent bexarotene, previously used to treat certain forms of lymphoma, has attracted close attention [76]. It has been shown in preclinical animal studies to cause a dramatic but reversible reduction in amyloid plaques and improvements in cognitive function. In this regard, its research has begun as a promising drug for the treatment of AD (Cleveland Clinic Foundation). Phase 2 clinical trial data for bexarotene are not yet available. Structurally similar to it is another oncolytic drug, tamibarotene (Osaka City Univ) [77], as well as the well-known drug isotretinoin (UH Univ Hospital) [78], widely used to treat inflammation of the sebaceous glands. The proposed mechanism of their action may be associated with retinoid receptors in the central nervous system [79]. Phase 2 AD trials of both drugs have recently been completed, but the results have not been disclosed.
Due to the presence of epidemiological data on a decrease in the number of patients with asthma among people taking drugs of the statin group for a long time [80], the main mechanism of action of which is aimed at reducing cholesterol (high-density lipoproteins) in the blood, several drugs of this class were tested for asthma . In the period from 2004 to 2012, the drugs pitavastatin [81] Kowa, atorvastatin (lipitor) [82] Pfizer, simvastatin (NIA) [83] were studied. However, no reliable positive results were obtained [84]. However, in 2015, phase 2 trials of the drug simvastatin in combination with L-arginine and tetrahydrobiopterin were started at the University of Massachusetts. In parallel, phase 4 clinical trials of this statin are underway in the treatment of patients with mild cognitive impairment (Charite University, Berlin).
A group of drugs acting on insulin homeostasis is being studied: recombinant human insulin in intranasal cocrystal form - humulin RU-100 (NIH) [19, 85]; long-acting insulin analog drug insulin detemir (Levemir/Levemir 300, Univ Washington) [86], peptide GLP-1 receptor agonists drugs liraglutide (Imperial College) [87] and exenatide (NIH) [88], drug MSDC -0160 [89], originally developed as a treatment for type 2 diabetes mellitus. also began the 2nd phase of clinical trials of the combined use of human albumin and immunoglobulin in mild and moderate forms of asthma in order to study the possibility of removing β-amyloid from the cerebrospinal fluid in patients.
Another 7 drugs are undergoing phase 2 clinical trials without the companies disclosing their structures and main mechanism of action: LND-101001 (“Lupin”) [11], MK-7622 (“Merck & Co”) [19], JNJ-54861911 (“Janassen Res & Dev”) [90], VI-1121 (VIVUS) [19], AVN-397 [91] and AVN-101 [92] (“Avineuro”) and herbal preparation RPh-201 [19] (Regenera Pharma).
According to the Thomson Reuters Integrity database and the website https://www.clinicaltrials.gov, 17 drugs were in phase 3 clinical trials at the end of October 2015.
Among the vaccines, the most promising drug is solanezumab (Ely Lilly) [43], which acts on soluble monomeric forms of β-amyloid. It initially did not show good results in two large phase 3 clinical trials, but was successful in a group of patients in the early stages of the disease. This gave the company the basis to return the drug to Phase 3 in pre-selected groups of patients. Trial results are expected by the end of 2021. Another drug, bapineuzumab (Johnson & Johnson) [93], which also acts on soluble forms of amyloid, did not pass phase 3 trials, which became one of the most serious disappointments in the search for anti-Alzheimer's drugs for last years. The company's total losses from the negative results of these tests are estimated at $340 million [94].
In the wake of the successful promotion of the drug, solanezumab, after successfully completing the 1st phase, received permission to immediately conduct the 3rd phase. Unlike the first two vaccines, aducanumab [95] acts on aggregated forms of β-amyloid. Testing of another vaccine based on IgG1 immunoglobulin, the drug gantenerumab [96], began recently. is testing a combination of the drug IgGIV [97], which is a liquid pasteurized form of highly purified human immunoglobulin IgG with albumin, in patients with mild to moderate forms of B.A. Immunoglobulin IgG itself as a drug called gammagard [19] has been tested, but there is no data on the further development of these studies.
The drug MK8931 [98], or verubecestat, and the oral drug AZD-3293 (LY-3314814) [11] are being tested in phase 3 AD as inhibitors of β-secretase (BACE1), a key enzyme in the formation of β-amyloid.
In recent years, great expectations have been associated with drugs based on the well-known dye and disinfectant, methylene blue (MB), after the discovery of its ability to block the formation of tau aggregates. The drug TRx-0014 [99] successfully passed the 2nd phase of trials (“TauRx”) for AD and was transferred to the 3rd phase for cognitive impairment (“Stanley Medical Res Inst”). There is also evidence of phase 3 clinical trials of the leukemic form of MS (TRx-00237) [100] in B.A. Trials in MCI are expected to begin.
One of the selective antagonists of the 6th serotonin receptor subtype, the drug Lu-AE-58054 “Lundbeck” [101], is undergoing phase 3 trials as an addition to donepezil therapy.
In 2015, it was planned to conduct the 3rd phase of clinical trials of the drug encenicline (FORUM Pharm and Mitsubishi Tanabe Pharma) [102], a specific agonist of 7-α-nicotinic receptors, in patients with AD while taking memantine, which was postponed, however , for a later period.
The drug memryte [103] - an oligopeptide leuprolide acetate - a GnRH receptor agonist (Curaxis) was tested for use in asthma in the form of biodegradable implants based on technology that provides long-term parenteral action of the substance. The results have not been published.
The drug nilvadipine [104], a well-known antihypertensive drug related to dihydropyridine voltage-gated calcium channel blockers, is in phase 3 trials at the Roskamp Institute.
The antidiabetic drug pioglitazone [105] has been submitted to phase 3 clinical trials for mild cognitive decline associated with the development of AD.
Tests have begun on the drug GV-971 (Shanghai Greenvalley Pharm) [19], which is an oligo-mannurarate, which has been demonstrated in in vitro
ability to reduce the toxicity of β-amyloid peptide.
Phase 2/3 clinical trials of the drug AC-1204 (Accera) [19], the mechanism of action of which is aimed at providing alternative energy sources for brain cells in conditions of the development of neurodegeneration, have been announced, but not started. The start of phase 3 clinical trials of the drug AVP-786 [11], a deuterated dexmethorphan and quinidine, is also expected. It is also being tested for depression and schizophrenia. The mechanism of action is associated with blockade of P-glycoproteins and inhibition of σ-1 and NMDA receptors in the brain.
In August 2015, phase 3 trials of the herbal preparation epigallactine gallate (Charite University, Berlin) [106], a component of Japanese green tea extract, were completed. The results have not yet been published. The mechanism of action of epigallactine gallate is the same as that of most herbal preparations - multi-target with pronounced antioxidant activity. Another herbal preparation SK-PC-B70M (SK Chemicals), representing a fraction enriched with the saponin glycoside from the Korean plant complex pulsatilla koreana, was tested for dementia of the Alzheimer's type. The results have also not yet been published.
In Fig. Table 2 summarizes data on the number and type of action of drugs for the treatment of asthma that are in clinical trials at the end of October 2015.
Rice. 2. Distribution of drugs by type of action at various stages of clinical trials (based on the TR database and the ClinicalTrials.gov website as of October 2015). The numbers above the columns indicate the number of drugs with this type of action.
As noted above, Aricept (donepezil), rivastigmine (Exenlon), galantimane (Reminyl) and memantine (Namenda, Noogerone, etc.) are most often used in the practice of pharmacotherapy of AD. At the same time, it is necessary to note a number of drugs that at different times were registered as treatments for AD and some other forms of dementia, but are currently used much less frequently.
In 1986, she registered the drug idebenone (idebenone, mnesis, etc.), a highly effective antioxidant and free radical scavenger, for oral use in the treatment of dementia of the Alzheimer's type [107]. Currently, it is also used to treat a number of other diseases, in particular Duchenne muscular dystrophy (since 2015).
In the mid-80s, the original drug ipidacrine was developed in the USSR, approved since 1990 for use as a stimulant of learning and memory in AD and other forms of senile dementia, as well as in the treatment of children with learning disabilities with minimal cerebral dysfunction [108] . The license for the use of amiridine in Japan under the name NIK-247 belonged to. Structurally related to tacrine, amiridine has significantly less toxicity, especially hepatotoxicity.
The drug Hupersine A, Cerebra [109], a plant alkaloid that is an acetylcholinesterase inhibitor and NMDA receptor antagonist, was developed for the treatment of AD and is used in China. It is currently undergoing phase 1 clinical trials for asthma as a dermal application.
Listed below are several dietary supplements registered for use to improve the condition of patients with asthma and other diseases: 1) ginkgo biloba extract - a phytoestrogen, registered by Ipsen in 1992 as a biological supplement that improves the cognitive functions of patients with senile and peripheral vascular disease dementia [110]; 2) the herbal preparation INM-176 (alzhima 176) based on ferrulenic acid complexes is used in a number of food supplements and was registered in 2003 as a biologically active substance for improving the condition of patients with asthma, as well as blood circulation, reducing the severity of mental disorders and analgesic effects [ 19]; 3) in 2009, the drug AC-1202 was registered as the first in its class - a food supplement for improving metabolic processes in moderate and more severe forms of B.A. It is believed to improve energy metabolism and lipid homeostasis in the brain [111].
Analysis of modern approaches to the search and creation of new effective drugs for the treatment of asthma allows us to identify the following main trends.
1. Creation of drugs that act on the main stages of the pathogenesis of the disease (the so-called “disease-modifying drugs”). They are able to slow down the development of structural and functional disorders in the central nervous system and provide a sustainable improvement in cognitive functions (in the case of AD), which persists even after withdrawal [112]. With regard to AD, the main directions of the search for such drugs are aimed at reducing the formation and stimulating the removal of amyloid peptides and neurofibrillary tangles from brain tissue. Fundamentally important importance is given to the search and validation of new molecular targets and pathways involved in the pathogenesis of the disease. As molecular targets, the enzymes that attract the most attention are the formation and degradation of β-amyloid peptide (β-, γ-, and α-secretases), as well as those involved in the tau protein phosphorylation cascade (Cdk-5). Special attention is drawn to the possibility of pharmacological correction of proteins of the ApoE system as a way to remove pathogenic β-amyloid oligomers. In recent years, several promising approaches to the pharmacological correction of AD have been proposed, in particular stabilization of mitochondrial functions (mitoprotectors), blockade of pathological protein aggregation in neurodegenerative diseases (drugs that prevent the development of proteinopathy), activation of endogenous cell protection mechanisms by stimulating autophagy and neurogenesis. Several promising groups of compounds have been proposed that implement these mechanisms in model systems.
2. Search for drugs that simultaneously act on several molecular targets that are involved in the pathogenesis of the disease (so-called “multi-target drugs”) [113]. Such approaches include the combination in one structure of the inhibitory properties of cholinesterase and monoamine oxidase, antioxidant and metal chelating properties, the ability to act as ligands for several receptors simultaneously, and the introduction of additional NO-generating fragments into the basic structure of the ligand. Examples of such multitarget agents are the drug lagostigil [114] and the domestic drug dimebon, which successfully passed the 2nd phase of clinical trials in Russia [115].
3. As is known, the search and creation of new drugs is a long (10-15 years), expensive (hundreds of millions of dollars) and risky process. Thus, in the field of AD over the past 10 years, more than 20 drugs have successfully passed the 2nd phase of clinical trials, but none have passed the 3rd phase. This is due to both the lack of knowledge about the mechanism of development of diseases (which are often a group of related pathologies with different etiologies) and the difficulty of modeling complex human neurodegenerative diseases in animals. In this regard, the development of new approaches to the use of already known drugs is very attractive from the point of view of simplifying clinical trials. This approach, called “drug repositioning” [116], appears to be extremely profitable from an investment point of view. Interestingly, studying cases of successful use of known drugs for the treatment of neurodegenerative diseases sometimes leads to the discovery of new pharmacological targets.
Despite the fact that over the past decade, not a single drug has been able to pass the 3rd phase of clinical trials, the active search for new drugs continues, and there is hope that in the coming years drugs will be created that act on the pathogenesis of AD and can significantly slow down the progression of this disease .
This work was supported by the Russian Science Foundation (project no. 14−23−00160).
Main drugs for Alzheimer's disease
To date, a cure for Alzheimer's disease that actually works and can completely cure a person has not yet been invented. All developed medications only help to slow down the course of the pathology, but are not able to eliminate it.
To treat Alzheimer's disease, drugs called cholinesterase inhibitors are used. This is an enzyme necessary for the breakdown of choline. Increasing the level of acetylcholine slows down the development of pathology and the formation of amyloid protein, which is one of the causes of the development of the disease. A representative of this drug for Alzheimer's is Exelon. It is available in the form of tablets, a solution for internal administration and a patch with the active substance applied. The latter form is very convenient, since in this case the person receives the required dose of the medicine automatically. While patients usually forget to take pills.
Aricept based on donepezil hydrochloride can be used to treat any form of dementia in Alzheimer's disease. It helps eliminate the clinical manifestations of pathology and slows down degenerative processes. Available in the form of tablets and solutions.
Glutamate NMDA blockers are also used in the treatment of dementia. The representative is the drug “Akatinol Memantine”. It slows down the atrophy of the gray matter of the brain.
Drug groups
Some medications can slow the progression of this disease. In some cases, the person will be able to return to normal life again. Psychiatrists and neurologists in most cases use the following groups of medications:
- Choliesterase inhibitors. These drugs are used for many degenerative diseases. They prevent the destruction of acetylcholine. It promotes the conduction of nerve signals. With the restoration of this signal, patients' memory is restored and attention improves.
- NMDA antagonists . Prescribed to normalize the patient's mental activity. Taking the pills normalizes concentration and attention.
- Neuroleptics - can remove symptoms of the disease such as aggression, delusions and hallucinations. The prescription of this drug must be agreed with a psychiatrist. It is important to choose the right dosage.
- Tranquilizers . Prescribed to combat anxiety, fear, panic attacks.
- Mood stabilizers are necessary for the patient to normalize mood. Prescribed to patients with mental disorders. Prescribed when the disease has changed the patient's character. Able to relieve aggression
- Antidepressants. Serve to combat depression. Prescribed by a medical specialist.
Second-line drugs for the treatment of Alzheimer's disease
The most effective drugs for Alzheimer's disease are cholinesterase inhibitors. However, treatment of the pathology should be comprehensive with the elimination of clinical manifestations.
What medications treat Alzheimer's disease:
- Glycine can be used to improve cerebral circulation and normalize the emotional background;
- To eliminate hallucinations and the appearance of obsessions, antipsychotics and tranquilizers can be used;
- Treatment of anxiety, panic attacks, and depression is carried out with the help of antidepressants.
All drugs for the treatment of Alzheimer's disease must be prescribed by the attending neurologist. Each of the drugs has its own contraindications and side effects, so using them independently can negatively affect your health.
In addition to drug treatment, the patient is prescribed other types of therapy:
- Physiotherapy;
- Aqua aerobics;
- Art therapy;
- Special classes to improve cognitive functions.
How to treat Alzheimer's disease: new drugs
New drugs and treatments for Alzheimer's disease are constantly being developed around the world. However, no one can yet say that a cure for Alzheimer's has been found.
An effective cure for Alzheimer's disease, developed in the United States, is currently in testing. The drug CAD 106 helps to increase antibodies to the amyloid protein, without increasing the concentration of T cells.
Another promising drug is MDA7. This immunostimulating agent, which increases the body's resistance to negative agents, stops the progression of degenerative processes in the brain.
Also, drugs that treat Alzheimer's disease may be substances originally invented for the treatment of other pathologies. Thus, Rosiglitazone, which was developed for the treatment of insulin-dependent diabetes mellitus, showed good results in eliminating dementia. The drug is still being tested on animals.
In order not to treat Alzheimer's disease, is it necessary to reduce the risk of developing the pathology?
Currently, medicine cannot answer for sure how to treat Alzheimer's disease in elderly and young patients. Many studies provide conflicting results. More or less reliable methods for preventing pathology are:
- Following a Mediterranean diet . The daily menu should consist of vegetables, fruits, whole grain cereals, fish, olive oil, and red wine. These foods contain many vitamins, including B and C, which are beneficial for maintaining neurological function.
- Eating certain foods . Research shows that consuming curcumin can to some extent prevent pathological processes that develop in the structures of the brain. And coconut oil can reduce the amount of amyloid plaques that form in the neurons of the brain stem. This property of coconut oil is explained by the fact that during the metabolism of its constituent substances, ketone bodies are formed, which take part in energy processes occurring in the brain. Cases have been described where, after using coconut oil for a month, the patient regained the ability to help with housework and pass simple psychological tests.
- Refusal of habits that destroy the body . Smoking, drinking alcohol, drug addiction and other bad habits greatly accelerate the death of nerve cells and the progression of the disease.
- Treatment of concomitant diseases . Diabetes, high blood pressure, and high cholesterol contribute to the development and progression of dementia. Drugs used to treat these diseases (such as statins) have not been shown to directly affect the quality of thought processes. However, observations show that during periods of exacerbation of such diseases, the deterioration of cognitive functions accelerates.
- Regular intellectual exercise . The researchers concluded that regular intellectual exercise can slow down the destruction of nerve tissue and slow down the progression of the disease. This effect is achieved by playing chess, learning foreign languages, playing musical instruments, board games, reading, and regular communication. Moreover, in 2015, Canadian researchers found that mastering psychotechniques aimed at developing mindfulness can prevent the development of the disease at the earliest stages.
If the patient has already been diagnosed with pathology, following these recommendations will not help get rid of Alzheimer's disease, but will slow down the decline in cognitive function, the development of dementia and maintain the neurological functions of the body at such a level that the person is able to care for himself for as long as possible.
How it works?
Neurodoctor affects the control centers of the brain.
The brain begins to produce dozens of neurohormones and form “corrective” nerve impulses.
Neurohormones are many times more effective than the most powerful drugs in quickly curing the disease. Nerve impulses eliminate pathological processes at the cellular level and correct the functioning of other organs and systems of the body.
LEARN MORE ABOUT THE METHOD
How to treat Alzheimer's disease in the elderly?
Modern pharmacological and therapeutic techniques do not make it possible to cure the disease completely, but they can facilitate its course and patient care.
So, today 4 types of drugs have been approved to help cope with cognitive impairment, but the question of how to treat Alzheimer's disease in the elderly is controlled by the government.
Three of them are inhibitors of cholinesterase, an enzyme that breaks down neurotransmitters responsible for neuromuscular transmission (acetylcholine). This enzyme is very important for learning, the normal functioning of memory, the ability to concentrate, the transmission of nervous excitement, the process of falling asleep and waking up. Cholinesterase inhibitors reduce the rate of destruction of acetylcholine. Due to this, its concentration in brain tissue increases, which compensates for the decrease in the rate of its production.
These drugs are recommended for use in the middle and late stages of the disease, since they have a number of side effects (vomiting, nausea, weight loss, muscle spasms, cardiac dysfunction). Some of them have been banned due to hepatotoxicity.
The use of cholinesterase inhibitors at the initial stage of the disease has virtually no effect, since it does not slow down the development of disorders.
The action of the fourth type of drug, Memantine, is based on regulating the intensity of production of glutamate, a biologically active chemical substance that transmits electrochemical impulses from nerve cells to muscle or gland cells. This excitatory neurotransmitter is important for the proper functioning of the nervous system, but its excess causes cell death. This condition is observed in Alzheimer's, Parkinson's, and multiple sclerosis diseases. Memantine stops the activation of glutamate receptors, thereby avoiding deterioration in the cognitive functions of patients. This drug is included in the list of vital and essential drugs. Just like cholinesterase inhibitors, Memantine is effective in moderate and severe stages of the disease. For patients with antisocial behavior, Memantine is prescribed in combination with antipsychotic drugs. This reduces aggression, but causes serious side effects. Long-term use of antipsychotic drugs in patients with Alzheimer's disease increases mortality, which should be taken into account when prescribing therapy.
Can Alzheimer's be cured forever?
In search of an answer to the question of whether Alzheimer's can be cured, researchers are exploring the use of verubecestat. It blocks the action of an enzyme involved in the formation of amyloid beta, the main component of amyloid plaques that form as the pathology progresses. There are positive results from testing the effect of the drug on animals and volunteers. After its use, the level of beta-amyloid in the blood and cerebrospinal fluid is significantly reduced without the development of serious side effects. The scientific community is awaiting the results of 2 large-scale experiments, which included 2000 and 1500 patients.
Pharmacological therapy is complemented by psychosocial care. Behavioral therapy is aimed at identifying problem behavior and correcting it. For example, in the early stages of the disease, the patient is taught the basics of correct behavior - they are helped to switch to an appropriate diet, give up bad habits, and change their lifestyle. In later stages, some problems (eg, urinary incontinence) are alleviated. At the same time, there are behavioral deviations with which such methods do not work, for example, wandering. Emotional assistance includes validation, supportive therapy, and sensory techniques. In the initial stages of the disease, they help patients better adapt to a new way of life. The technique of stimulating presence (playing audio recordings with the voices of relatives, viewing joint photos, videos) helps reduce the level of anxiety. Techniques aimed at improving orientation in reality make it possible to reduce cognitive deficits, learn to re-orient in time and space, and maintain the patient’s personality.
Prevention of Alzheimer's: drugs
Unfortunately, drugs have not yet been developed to prevent Alzheimer's disease, since the exact cause of this pathology cannot be reliably identified.
Prevention includes measures to improve overall health and improve brain function:
- Balanced diet;
- Moderate physical activity;
- Active lifestyle;
- Mental activity;
- No bad habits (smoking, drinking alcohol, drugs);
- No stress.
Treatment of Alzheimer's disease at the Yusupov Hospital
A special department has been created at the Yusupov Hospital for the treatment of neurological pathologies. The hospital's doctors have extensive experience treating various forms of Alzheimer's disease. Prescription of drugs is carried out by a qualified neurologist based on the individual characteristics of the patient.
Patient care is provided by specially trained staff who know the intricacies of caring for patients with Alzheimer's. Psychological support is also provided to patients and their relatives.
The work uses drugs for Alzheimer's, which are approved for use in Russia. Also, a certified research center operates on the basis of the Yusupov Hospital. Therefore, patients have the opportunity to receive the latest treatment, which is not available in other hospitals.