general information
There are 12 pairs of intercostal nerves in the human body. They originate from the roots of the thoracic spinal cord and cover the entire chest, adjacent to the peritoneum, muscles, skin and mammary glands. The individual fibers of each nerve are responsible for tissue sensitivity, motor function and regulation of the functioning of all structures. Accordingly, damage or inflammation in any area can radiate pain to a variety of parts of the body.
The sensations can imitate diseases of internal organs: myocardial infarction, angina pectoris, pancreatitis, gastritis, cholecystitis, etc. In some cases, only a doctor can accurately determine the nature of the pain after a full examination. That is why it is important to seek help promptly if chest pain occurs.
Make an appointment
Forms
There is no special classification of the disease. There are several separate forms depending on the mechanism of occurrence:
- radicular: associated with irritation of the spinal cord roots at the point of their exit from the spinal column;
- reflex: associated with overstrain of muscle fibers at the site of the nerve passage.
There is also a classification of neuralgia depending on:
- causes: primary (associated with damage or inflammation of the nerve itself) and secondary (due to other diseases);
- localization: unilateral and bilateral;
- course of the disease: acute and chronic.
Causes
The list of main causes of intercostal neuralgia includes:
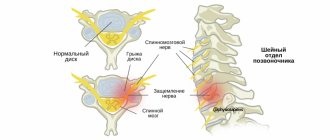
- degenerative-dystrophic diseases of the spine: osteochondrosis, arthrosis, hernias and protrusions of discs, etc.;
- uneven or excessive load on the spine and back muscles (due to carrying heavy objects, poor posture, etc.);
- spinal column deformities (primarily scoliosis);
- diseases of the nervous system, in particular multiple sclerosis;
- infectious lesions: tuberculosis, herpes zoster, influenza;
- injuries of the spine and chest, surgical interventions in this area;
- tumors in the ribs, sternum, spinal column;
- taking certain medications;
- increased load on the respiratory muscles and abdominal muscles;
- increased intra-abdominal pressure, including during pregnancy.
In addition, intercostal neuralgia can occur secondary to other diseases, for example, pleurisy, pathology of the digestive system, kidney disease, thyrotoxicosis, and immunodeficiency states. Adolescents during the period of active skeletal growth may also experience similar symptoms.
Symptoms
The main symptom of intercostal neuralgia is severe pain in the chest along the nerve. As a rule, it occurs suddenly and resembles an electric shock, gradually spreading along the ribs. The nature of the sensations can be different: shooting, pulsating, constant, burning or dull.
Deep breathing, turning the head or body, bending, pressing or simply touching the chest causes a pronounced increase in pain. In addition, characteristic signs of neuralgia are:
- persistence of pain at night;
- the ability to determine the epicenter of pain;
- redness or paleness of the skin in the affected area;
- a feeling of tingling, crawling or, conversely, numbness along the affected nerve;
- slight muscle twitching in the affected area.
As a rule, during an attack of neuralgia, a person tries to lie or sit motionless in a position in which the pain becomes slightly less.
If the cause of the pain syndrome is herpes zoster, first redness appears on the skin along the affected nerve, then numerous blisters that burst, forming crusts. After recovery, increased pigmentation remains in this area for some time.
Differences from myocardial infarction
Chest pain, especially on the left, can be a consequence not only of intercostal neuralgia, but also of more serious problems. The most dangerous is myocardial infarction. This condition requires emergency medical attention. The characteristic differences in pain are:
- occurrence against the background of physical, less often psycho-emotional stress;
- spread to the left arm, shoulder, left half of the neck and lower jaw;
- no changes when turning the body, bending, pressing on the sore area;
- decreased intensity when taking nitroglycerin and its analogues.
A heart attack is often accompanied by cold, sticky sweat, pale skin, dizziness, and fear of death.
It is important to remember that the signs of a cardiovascular accident and intercostal neuralgia are not always so radically different. An accurate diagnosis can only be made by a doctor.
Diagnostics
Intercostal neuralgia, regardless of the severity of the pain syndrome and its location, requires a full diagnosis. The following examinations will help distinguish it from other pathologies:
- questioning and medical history: identifying the nature of the sensations, the conditions of their occurrence, the duration of the attack, concomitant diseases;
- examination and palpation: the doctor evaluates the appearance of the skin, checks the reaction to movements, pressing, turning, bending, assesses the severity of reflexes;
- laboratory diagnostics: general and biochemical blood tests, general urine tests: allows to identify signs of damage to the heart muscle (tests for troponins, CPK), inflammation, renal pathology, gastrointestinal diseases, etc.; the exact set of tests depends on the location of the source of pain;
- ECG, ultrasound of the heart: allow you to identify or exclude cardiovascular pathology;
- X-ray, CT or MRI of the thoracic spine: helps to identify osteochondrosis, osteoporosis, tumors, hernias and protrusions of intervertebral discs, etc.;
- Chest x-ray: allows you to assess the condition of the lung tissue and identify signs of tumors;
- Ultrasound of the kidneys, abdominal organs (excludes relevant pathology);
- FGDS to exclude pathologies of the esophagus, stomach, duodenum;
- myelography, contrast discography, electrospondylography to assess the condition of the spine, intervertebral discs, spinal cord and its roots.
If necessary, consultations with narrow specialists and additional examinations are prescribed.
Make an appointment
Diagnostic methods
You need to see a general practitioner. After examination and exclusion of other pathologies, the therapist refers to a neurologist who determines the symptoms and treats intercostal neuralgia. The doctor examines the images, prescribes tests and medical examinations.
Instrumental diagnostic methods of examination:
- Radiography. Allows you to examine the bone structure. Makes it possible to determine the presence of non-traumatic or traumatic disorders. X-rays are taken in direct, oblique and lateral projections.
- CT scan. Examines bone and muscle structure in combination. More often used to detect pathological changes in bone structures.
- Myelography. A contrast agent is injected into the spinal canal. This is the main method for diagnosing soft tissue structures (nerve roots and spinal cord).
- Contrasting discography. During the procedure, a contrast agent is injected into the intervertebral disc.
- Magnetic resonance imaging. Allows you to obtain images of organs and tissues. Detects pathological changes in soft tissue structures: nerve tissue, muscles, ligaments, hernias and degenerative changes in intervertebral hernias.
- Electrospondylography. Using the computer diagnostic method, it is possible to assess the condition of the spinal column, identify the disease at an early stage, determine the extent of damage and monitor the course of the disease.
Treatment
Intercostal neuralgia requires complex and often long-term treatment, including medication, physiotherapy, massage, etc.
Drug therapy
In the acute phase of the disease, therapy is aimed at relieving pain and improving the patient's condition. Depending on the specific clinical situation, the following are prescribed:
- non-steroidal anti-inflammatory drugs (NSAIDs): products based on diclofenac, nimesulide, ibuprofen, meloxicam and their derivatives; used in tablet, injection and local (creams, ointments, patches) form;
- analgesics: analgin and products based on it; like NSAIDs, they relieve pain;
- muscle relaxants to eliminate muscle spasms: mydocalm, etc.;
- group vitamins: milgamma, neuromultivitis, etc.; necessary to restore normal functioning of nerve fibers;
- sedatives to reduce the psycho-emotional component of pain and improve sleep.
If necessary, the following may additionally be prescribed:
- anticonvulsants: inhibit the passage of pain impulses;
- antidepressants to relieve tension;
- antihistamines and diuretics: relieve tissue swelling, especially relevant for pinched nerve roots;
- antiviral drugs for herpes zoster;
- glucocorticosteroids for persistent pain and severe inflammation that cannot be relieved by milder means.
Physiotherapy and exercise therapy
Physiotherapeutic procedures are prescribed after the acute pain subsides. Help speed up recovery:
- UHF;
- reflexology;
- magnetic therapy;
- electrophoresis;
- laser treatment;
- paraffin applications;
- mud therapy.
These procedures help improve blood circulation and metabolism in the affected area and accelerate the regeneration of nerve tissue.
Physical therapy exercises are prescribed after complete recovery. The main goal of gymnastics is to unload the back muscles. The complex is developed individually. The first classes should be carried out under the supervision of a specialist; in the future, home exercises are allowed.
Other treatments
Since very often the cause of intercostal neuralgia is pathology of the spine and spinal cord, the following are often used as additional methods of influence:
- acupuncture;
- manual therapy;
- therapeutic massage, including the use of warming agents;
- Shiatsu massage (acupressure);
- osteopathy;
- underwater traction and other techniques.
Like all medical procedures, these techniques are used only in a clinical setting and are carried out by specialists with medical education and the appropriate certificate.
Table 1 Recommendations for the prevention of complications associated with taking NSAIDs
| Risk of gastrointestinal complications | |||
| Short | Moderate | High | |
| Low risk of cardiovascular complications | Monotherapy with NSAIDs (choosing a drug with the least ulcerogenic potential) | NSAID + proton pump inhibitor/misoprostol | If possible, alternative treatment or NSAIDs - selective COX-2 inhibitor + proton pump inhibitor / misoprostol |
| High risk of cardiovascular complications (low dose aspirin is indicated) | Naproxen + proton pump inhibitor/misoprostol | Naproxen + proton pump inhibitor/misoprostol | Avoid prescribing NSAIDs, including selective COX-2 inhibitors, use alternative treatment |
Another drug that has a sufficient gastroprotective effect is the synthetic prostaglandin E1 - misoprostol, but its use is limited by its high cost.
The protective effect of the H2-histamine receptor antagonist, famotidine, has been proven only in combination with ibuprofen. A combination drug was created, which is currently not available in Russia. However, both of its components can be purchased and taken separately. They are affordable.
It is necessary to inform the patient that even despite intense back pain, his health is not in danger. The vast majority of patients have a favorable prognosis: within 3 months, more than 90% of patients do not seek medical help again.
Less significant are complications from the urinary and central nervous systems, hepatotoxic effects of drugs:
Adverse events from the urinary system
All NSAIDs can have nephrotoxic effects. When taking drugs of this group, the following types of complications may develop: Development of acute renal failure due to spasm of renal vessels. Other mechanisms of organ damage are also possible. NSAIDs cause a moderate increase in arterial hypertension, reduce the effectiveness of antihypertensive drugs, and can cause electrolyte disturbances (hyperkalemia, hyponatremia and edema). Taking NSAIDs is associated with an increased risk of kidney cancer.
Adverse events from the cardiovascular system
All NSAIDs, both selective and non-selective, increase the risk of developing cardiovascular complications: clinical manifestations of coronary heart disease, heart failure, increased blood pressure, and the development of atrial fibrillation. Naproxen has the lowest risk of developing complications from the cardiovascular system. (Daniel H Solomon, MD, 2015). NSAIDs interact with all classes of antihypertensive drugs except calcium antagonists, reducing their effectiveness. Their use may increase blood pressure in patients (White WB. 2007). Safety issues are more relevant for patients with a high risk of cardiovascular complications (old age, long-term hypertension, constant use of antihypertensive drugs, diabetes mellitus); in patients with a low risk, they do not limit the use of drugs in this group.
Adverse events from the blood system
Neutropenia is a rare complication of taking NSAIDs and develops in less than 1% of patients; no risk factors for the development of this condition or association with taking individual drugs from this group have been established. The antiplatelet effect is associated with inhibition of COX-1, which leads to a decrease in the production of thromboxane A2. It is necessary to avoid taking NSAIDs in patients with thrombocytopenia (less than 50 x 109/l). Before surgery, drugs should be discontinued within 3-5 half-life periods. For most NSAIDs, the antiplatelet effect disappears 3 days after discontinuation. The antiplatelet effect of ibuprofen is eliminated 24 hours after discontinuation of the drug. Highly selective COX-2 inhibitors have little effect on platelet hemostasis. Concomitant use of NSAIDs and aspirin may reduce the antiplatelet effect of the latter. Interaction with warfarin leads to a significant increase in INR when taken simultaneously. More frequent monitoring of the indicator is required.
Allergic and pseudoallergic reactions
Pseudoallergic reactions associated with inhibition of COX-1 can be caused by taking aspirin and all (“crossover”) NSAIDs that inhibit COX-1: Piroxicam, Indomethacin, Ibuprofen, Naproxen, Ketoprofen, Diclofenac, Ketoralac, and less commonly, drugs with weakly expressed properties of COX inhibitors -1 — paracetamol; and even less often when using drugs that selectively inhibit COX-2, nimesulide, coxibs, oxicams; a dose-dependent effect was noted for these drugs. Allergic reactions to NSAIDs develop in the form of angioedema, urticaria or anaphylaxis. Cross-reactions to drugs with similar chemical structures are possible. If pseudo-allergic and allergic reactions to any of the NSAIDs develop, it is necessary to avoid taking all drugs in this group; as an alternative, use paracetamol in a single dose of no more than 650 mg.
Adverse effects from the respiratory system
When taking aspirin and other non-selective COX-1 blockers, it is possible to develop bronchospasm, decompensation of bronchial asthma and other obstructive bronchial lesions of inflammatory origin.
Adverse events from the hepato-biliary system
Cases of liver failure when taking NSAIDs are quite rare (3.7 per 100,000 patients taking drugs of this group). Transient slight increases in the activity of liver enzymes (less than 3 upper limits of normal) are not prognostic signs of the development of acute liver failure associated with the action of NSAIDs. Ibuprofen is the safest NSAID and has not shown severe liver damage in large studies. Along with paracetamol and aspirin, the drug is one of the best-selling over-the-counter drugs in the world. Newer NSAIDs, selective COX-2 inhibitors, oxycams and coxibs have a relatively low risk of toxicity. In rare cases, piroxicam can cause severe liver damage.
The drug Nimesulide was withdrawn from sale in a number of countries (Japan, Finland, Turkey, Israel, India, Sri Lanka, and later Ireland), and was never put on sale in the USA and Great Britain, due to a pronounced hepatotoxic effect in a series of clinical observations , however, various epidemiological studies do not confirm this information.
The European Medicines Agency (EMA) recommends only short-term use of the drug (15 days), at a dose not exceeding 200 mg/day (100 mg x 2 times a day) in adults. Taking into account all the data obtained, the Agency believes that the potential benefits of the drug, subject to restrictions, outweigh the potential risks.
The economic feasibility of monitoring liver enzyme activity in patients taking NSAIDs has not been established.
In case of an increase in activity by more than 3 times compared to the upper limit of normal, a decrease in the concentration of serum albumin, or an increase in INR, it is necessary to assume the hepatotoxic effect of NSAIDs.
Adverse skin effects
The risk of developing toxic epidermal necrolysis and Stevens-Johnson syndrome (malignant exudative erythema) when taking NSAIDs is 1 in 100,000. The highest risk is when taking piroxicam, the lowest is when taking diclofenac and ibuprofen.
Adverse effects from the nervous system
Elderly patients taking NSAIDs, especially indomethacin, may experience worsening cognitive impairment and the development of psychosis. Taking ibuprofen and naproxen is associated with the development of aseptic meningitis. In a small proportion of patients, taking NSAIDs is accompanied by the development of tinnitus. The complication is reversible after discontinuation of the drugs.
Complications
Complications of intercostal neuralgia occur quite rarely, however, in severe cases, without appropriate treatment, the patient may encounter the following problems:
- severe spasm of the respiratory muscles, limiting inhalation and exhalation;
- inability to get out of bed due to significant increase in pain;
- excessive pain syndrome that is not relieved by conventional analgesics and NSAIDs;
- heart rhythm disturbances due to muscle spasms and nerve pathology;
- decreased leg mobility.
In addition, complications can be caused by attempts to be treated outside the clinic. Abscesses and cellulitis after acupuncture, paralysis and decreased sensitivity after manual therapy are not a complete list of problems. That is why you should not treat intercostal neuralgia either independently or with the help of dubious specialists.
Low risk
No risk factors
NSAIDs differ in the severity of their ulcerogenic effects.
Indomethacin has the highest risk of gastrointestinal complications (relative risk {RR} 2.25), followed by naproxen (RR 1.83), diclofenac (RR 1.73), piroxicam (RR 1.66), ibuprofen (RR 1.43), and meloxicam (OR 1.24).
A dose-dependent effect of the drugs was noted (Richy F, Bruyere O, Ethgen O, 2004):
Low-dose ibuprofen (RR 1.6, 95% confidence interval 0.8-3.2)
High-dose ibuprofen (RR 4.2, 95% confidence interval 1.8–9.8)
Low-dose naproxen (RR 3.7, 95% confidence interval 1.7-7.7)
Naproxen at high doses (RR 6.0, 95% confidence interval 3.0-12.2)
Low-dose indomethacin (RR 3.0, 95% confidence interval 2.2-4.2)
High-dose indomethacin (RR 7.0, 95% confidence interval 4.4-11.2)
Not included in this review, ketorolac also has a pronounced gastrotoxic effect. In one study (García Rodríguez LA, Cattaruzzi C, 1998), it was shown that the risk of developing adverse events from the gastrointestinal tract with the drug is 5.5 times higher than that of other NSAIDs. Therefore, the duration of taking the drug is limited to 5 days.
In Russia and abroad, the drug is available with a prescription.
Despite the possibility of early gastrotoxicity, in most cases it does not appear within several weeks of taking the drugs. The possibility of modifying risk factors depends on the conditions of medical care for the patient.
- Patients with a history of complicated or uncomplicated gastrointestinal ulcer disease are advised to undergo testing for H. pylori before prescribing NSAIDs or aspirin. If the result is positive, appropriate treatment is carried out (even in cases where it is assumed that the previous development of ulcers was associated with taking NSAIDs).
- It is necessary to use minimal doses of drugs, the course of treatment should be as short as possible.
- In patients with an average and high risk of complications from the gastrointestinal tract, the use of selective COX-2 inhibitors or NSAIDs in combination with antisecretory drugs: proton pump inhibitors (omeprazole 20 mg/day, esomeprazole 20 mg/day up to 6 weeks), H2 blockers is indicated -histamine receptors (ranitidine 150 mg/day once at night, famotidine 40 mg x 2 times a day). Both groups of drugs reduce the severity of dyspepsia in patients. Efficacy at recommended doses is similar.
- In patients with a high risk of complications from the gastrointestinal tract, selective COX-2 inhibitors may be prescribed in combination with antisecretory drugs
- Concomitant use of aspirin with COX-2 inhibitors completely eliminates the gastrointestinal safety benefits of the latter.
- Unexplained anemia, iron deficiency, severe dyspepsia, signs of gastrointestinal bleeding indicate a possible complication of taking NSAIDs. It is necessary to consider the possibility of performing esophagogastroduodenoscopy.
Prevention
Prevention of intercostal neuralgia is mainly general measures aimed at strengthening the muscle frame and improving the health of the body. Neurologists recommend:
- lead an active lifestyle, play sports at an amateur level;
- minimize hypothermia and colds;
- watch your posture;
- avoid lifting heavy objects;
- maintain a high level of immunity;
- eat a balanced diet, if necessary, take additional vitamins, especially group B;
- treat chronic diseases in a timely manner;
- avoid stress, get proper rest and ensure yourself at least 8 hours of sleep every night.
Following these simple rules will significantly reduce the risk of developing intercostal neuralgia.
Prevention of intercostal neuralgia
The main preventive measure is gymnastics. It is necessary to perform exercises that promote muscle development, strengthening and mobility of the spine. Avoid drafts, uncomfortable positions and excessive physical activity. Everything should be in moderation.
It is important to control your posture, not lift excessive weights, eat a rational and balanced diet, take vitamins, and avoid fasting and mono-diet.
Do not forget to promptly treat diseases that can cause the development of neuralgia.
Treatment at the Energy of Health clinic
Doctors at the Energy of Health clinic will always come to the aid of patients with intercostal neuralgia. We offer each client:
- a full examination with consultations with specialists for an accurate diagnosis;
- individual selection of treatment regimen;
- services of a qualified chiropractor;
- own exercise therapy room for the most effective and safe exercises;
- modern methods of physiotherapy;
- massotherapy;
- drug blockades for severe pain syndrome.
Regular observation by a neurologist after the acute period of the disease has subsided will help prevent recurrent attacks.
Treatment of occipital neuralgia
Many patients benefit from simple measures: rest, warmth on the neck, painkillers (ibuprofen, naproxen). Massage courses are useful: they help to stretch tense neck muscles.
If this does not help, your doctor may prescribe other medications: muscle relaxants (drugs that relax tense muscles), some anticonvulsants, antidepressants. Sometimes occipital nerve blocks are required - injections of drugs that interrupt the transmission of pain nerve impulses.
In rare cases, surgical treatment may be necessary. If the pain is due to the fact that the nerve is pinched by a blood vessel, microvascular decompression is performed. Sometimes, in order to block pain impulses, a special device is used - a neurostimulator.
In general, occipital neuralgia is not dangerous; most patients can cope with it. But in order to prescribe the appropriate treatment, you need to establish the correct diagnosis. Make an appointment with our neurological center by phone.
The material was prepared by Natalya Yurievna, a neurologist at the international clinic Medica24, Candidate of Medical Sciences Lasch.
Advantages of the clinic
In the neurology department of the Energy of Health clinic, every patient receives the highest level of specialists and modern equipment for diagnosing and treating diseases. We take an integrated approach to therapy and use not only medications, but also physiotherapy, exercise therapy and massage.
Treatment is prescribed only after a thorough examination and is monitored by a specialist until the patients fully recover. Adequate prices, convenient location, private parking - we do everything for the convenience of our clients.
If intercostal neuralgia interferes with living, walking and moving, do not delay treatment. Sign up for the Health Energy clinic and get rid of pain.