Venous encephalopathy is a common condition of the cerebral vascular system, in which there is a violation of the venous outflow of blood from the brain. Moreover, this disease can be combined with arterial problems and so-called discirculatory encephalopathy (the author uses the words “so-called” due to the fact that venous encephalopathy is also inherently a discirculatory process), or it can be an independent disease.
Information for doctors. According to ICD 10, there is no diagnosis of venous encephalopathy. Because of this, to more accurately indicate the presence of a venous problem, it is more logical to use codes M53.0 (cervicocranial syndrome) and indicate that problems with the cervical spine led to this condition, leading to the diagnosis description of chronic venous outflow disorder syndrome, or indicate this syndrome within the framework of diagnosis I67.8 - discirculatory encephalopathy - in the event that this diagnosis also occurs.
At the moment, venous dysfunction is a controversial condition, not recognized by a number of authors, however, the clinical practice of the author of the site shows the importance of the presence of disturbances in the venous outflow from the cranial cavity in the formation of various symptoms.
A little about venous encephalopathy
Venous encephalopathy develops in the presence of chronic disorders of the venous outflow of blood from the brain. Due to this condition, the production of cerebrospinal fluid changes, intracranial pressure increases, and metabolic processes are disrupted. There are many reasons for this. Among them, the most common are hereditary structural features of the vein wall, cervical compression syndromes, residual dysontogenetic background (vascular hypoplasia, etc.). Less commonly, these processes arise from such reasons as the consequences of an inflammatory process in the veins and sinuses (for example, after sinus thrombosis), compression by a brain tumor, or trauma to the skull, including birth trauma.
Venous encephalopathy itself as a disease does not pose a threat to the patient’s life. However, its presence can significantly worsen the quality of life, reduce ability to work, and worsen the prognosis in the presence of other somatic diseases.
Causes
The main reason for its appearance is chronic cerebral ischemia caused by various vascular disorders:
- About 60% of cases of DEP are caused by atherosclerotic changes in the walls of cerebral vessels;
- Arterial hypertension ranks second in the list of causes. It can be observed in a number of pathologies: chronic glomerulonephritis, hypertension, polycystic kidney disease, Itsenko-Cushing's disease, pheochromocytoma, etc.
- Hypertension provokes encephalopathy due to the occurrence of vasospasm of the central nervous system, leading to depletion of blood flow;
- Pathology of the vertebral arteries can also cause the disease, as it is responsible for 30% of cerebral circulation. If the primary disease is instability of the cervical spine of a dysplastic nature, osteochondrosis, Kimerli's anomaly, developmental defects or previous spinal trauma, a symptomatic picture of circulatory disorders in the vertebrobasilar region is observed;
- DEP often occurs as a concomitant disease with diabetic microangiopathy. If, with diabetes, the patient is unable to adjust the blood glucose level to the upper limits of normal.
Also, the causes of dyscirculatory encephalopathy can be:
- Chronic or persistent hypotension;
- Arrhythmia;
- Hereditary angiopathy;
- Traumatic brain injuries;
- Systemic vasculitis.
Symptoms and diagnosis of venous encephalopathy
The symptoms of venous encephalopathy are varied, often they resemble other diseases (dyscirculatory process, problems with the cervical spine, depression, etc.). The most typical “venous” complaints are the following symptoms:
- Morning (sometimes night) headaches of a bursting nature
- Dizziness, which is non-systemic in nature, worsens when changing body position,
- Noise in the head, especially when going to bed
- Visual disturbances (a progressive decrease in visual acuity and various photopsia may be noted)
- Feeling of discomfort in the eyes in the morning
Symptoms are aggravated by working at an incline, wearing narrow collars and ties, and sleeping on a low surface. Objectively, the following signs may also be noted:
- Pastosity (swelling) of the face and eyelids in the morning (with a pale or bluish tint)
- Mild nasal congestion
Conditions after which the complaints intensify are also characteristic: bending forward with lowering the head, horizontal position of the body, taking alcohol-containing drinks, nitrates, vasodilators, warm bath or sauna, hot drinks, being in a stuffy room, daytime sleep. Or, on the contrary, they decrease: drinking caffeine-containing drinks, rinsing in cold water, walking in the fresh air, vertical body position, sleeping strictly on a high pillow.
A neurological examination is important, which, however, also does not have cardinal diagnostic signs. The neurological status reveals the following symptoms: nystagmus is expected, there is convergence insufficiency of the eyeballs, decreased corneal reflexes (rarely tested), pain in the exit points of the branches of the trigeminal nerve, decreased sensitivity in the area of innervation of the first trigeminal nerve, dissociation (difference between) knee and Achilles reflexes, impaired coordination when walking.
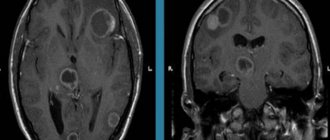
Diagnostic methods include a set of the following examinations: ophthalmological examination, which allows to identify congestion in the retina, dilated retinal veins, ultrasound examination of the veins of the neck and brain, MRI venography (if necessary, with the introduction of a contrast agent). A relative study that can help in the absence of the above methods is rheoencephalography, which allows one to evaluate microcirculation and venous outflow. The presence of diastolic index values below normal may make you think about the presence of venous disorders.
However, there are no clear diagnostic criteria. In 90% of cases, the diagnosis is made on the basis of complaints, anamnesis, and neurological examination data, focusing on the research methods carried out (if possible).
Ideally, for a reliable diagnosis, it is necessary to combine the presence of all the above-described signs of the disease along with the absence of other reliable reasons for the development of the patient’s complaints.
Material and methods
This work was carried out on the basis of the neurological department of City Clinical Hospital No. 1 named after. N.I. Pirogov. The study was approved at a meeting of the local ethics committee. All patients signed an informed consent form to participate in the observational program.
The observational program involved 60 patients with a reliable diagnosis of “chronic cerebral ischemia”, made in accordance with the diagnostic criteria proposed by V.A. Parfenov (2015) [17], and with signs of systemic venous insufficiency, as well as clinical signs of venous encephalopathy, including: morning headaches, a feeling of heaviness in the head, noise in the head, the presence of a venous network on the face.
Inclusion criteria
The program included: ages from 55 to 80 years; reliable diagnosis of chronic cerebral ischemia; signs of peripheral and central venous insufficiency; cephalgic syndrome; asthenic condition at the time of inclusion in the study in accordance with diagnostic criteria; ataxic syndrome; stable clinical, neurological or hemodynamic status of the patient for 28 days at the time of inclusion in the study.
Non-inclusion criteria
the program included: cognitive impairment (dementia) affecting the ability to participate in the program (Mini Mental Status Scale score at the time of enrollment less than 24 points); reluctance to cooperate within the program; severe disability (inability to move independently, difficulties in self-care); inability to perform any of the program procedures (for example, the presence of severe aphasia due to a previous stroke); severe depression/anxiety (score 14 or more on the HADS Hospital Anxiety and Depression Scale), requiring consultation with a psychiatrist; severe renal or liver dysfunction; severe heart failure; hypersensitivity to L-lysine aescinate or vinpocetine, or their components; taking any other drugs that can affect headache, asthenia, ataxic disorders, with the exception of those used for the treatment of the underlying disease.
All patients were randomly selected into two groups of 30 people. Patients in the main group received L-lysine escinate 10 ml per 200 ml of physiological solution intravenously, the control group received vinpocetine 2 ml per 200 ml of physiological solution intravenously. The course of treatment in both groups was 10 days.
The leading clinical syndromes in both groups were asthenic (according to diagnostic criteria), cephalgic and ataxic. The age of the patients ranged from 55 to 80 years (average age 63.21±6.34 years), the groups did not differ statistically significantly on this indicator (p=0.632) - the average age of the patients in the main group was 64.57±7.12 years, control group - 62.83±8.06 years. There were 13 men in the main group and 16 in the control group.
All patients had a wide range of vascular risk factors. Patients with grade 1–2 arterial hypertension took a standard set of antihypertensive drugs in different combinations: diuretics, angiotensin-converting enzyme inhibitors, calcium channel blockers and β-blockers. In the main group, dyslipidemia was detected in 18 patients, type 2 diabetes mellitus - in 4, in the control group - in 21 and 2 people, respectively. 11 patients in the main group and 9 in the control group had a history of varicose veins of the lower extremities. There were no heart attacks or strokes observed in patients before inclusion in the program.
The duration of the observation program was 10 days, which corresponded to the duration of the course of intravenous infusions.
The program provided for 3 visits to the doctor.
Screening visit (visit 1),
during which eligibility/exclusion criteria were assessed, including the Mini Mental State Examination (MMSE) and the Hospital Anxiety and Depression Scale (HADS).
Treatment start visit (visit 2)
- As a rule, it took place on the same day as the first visit, in some cases the next day. It included an assessment using the modified asthenia rating scale (MFI-20), a 100-mm visual analogue scale (VAS) for headache (100 mm is the most severe pain, 0 mm is no pain), the Subjective Neurological Disorder Scale (SSND; this scale consists out of ten VAS, in each of which 0 corresponds to the absence of symptoms, and 10 to the most severe symptoms; the following clinical indicators are taken into account: dizziness, unsteadiness, tinnitus, heaviness in the head, parameters of memory, attention, fatigue and quality of sleep) [12] . The Tinetti scale was also used, which includes two blocks to assess general stability and gait. The total assessment of the degree of impairment of general motor activity has the following gradation: 0–20 — significant degree, 21–33 — moderate, 34–38 — mild, 39–40 — normal. In addition, an ophthalmological examination was carried out to determine congestion in the fundus, narrowing of the arteries, dilation of the veins, blurring of the optic discs - only the presence or absence of the sign was determined. Duplex scanning of vessels (veins) was performed in a horizontal position after 10 minutes of rest. The blood flow velocity was assessed in the veins of Rosenthal, the angular veins of the eye, the bulbs of the internal jugular veins and the vertebral veins.
All examinations were carried out before the first dose of the drug was administered.
End of treatment visit (visit 3)
- was prescribed 10 days after visit 2 and included an examination similar to the examination performed at visits 1 and 2.
Statistical data processing was performed using nonparametric methods when comparing dependent and independent groups (Spearman correlation analysis, t-test for paired cases and Wilcoxon test). To assess the uniformity of distribution, the Kolmogorov-Smirnov criterion was used. For dichotomous variables, analyzes using 2 × 2 tables and McNemar's test were used. Taking into account the predominantly uneven distribution of indicators, the data were presented as the median and the 25th and 75th quartiles (Me [Q25; Q75]). In some cases, for greater representativeness, the mean and standard deviation were used. Differences between indicators were considered statistically significant if the probability of error was less than 5%.
Dizziness due to venous encephalopathy
Dizziness with venous encephalopathy has characteristic differences. It occurs after a change in body position, passes quickly enough in an upright position, and intensifies in the morning. However, this symptom can also be provoked by other factors that would also provoke it in other diseases: alcohol intake, a jump in blood pressure, etc.
Objectifying the presence of dizziness due to impaired venous outflow is difficult. Patients are checked for accuracy when performing corrdinator tests, Romberg test is performed, nystagmus is checked while standing and then in a lying position. Increased nystagmus while lying down may also indicate disturbances in venous outflow.
Dizziness with venous encephalopathy does not pose any threat to life. As a rule, treatment quickly relieves this symptom.
Treatment of venous encephalopathy
To begin with, I would like to note the groups of drugs that are best not to be used for venous encephalopathy, as they can cause a deterioration in well-being. These include antihypertensive drugs of the group of calcium channel blockers, nitroglycerin, nicotinic acid. These drugs, causing dilatation of the veins, only worsen the reasons that led to the pathological condition.
The drugs of choice for venous encephalopathy are venotonics, both for intravenous administration (L-lysine escitate, also known as horse chestnut salt, escin and amino acids), and for oral administration, these include Antistax, Troxevasin, Detralex, Phlebodia. The author of the site prefers to prescribe Detralex, although the choice of drug is the prerogative of the attending physician.
In addition, vasoactive drugs (Tanakan, Cavinton, Trental), metabolic agents (Mexidol), and specific diuretics that reduce the level of intracranial pressure (Diacarb, Mannitol) are used. Symptomatically, betahistine drugs, NSAIDs (especially for problems with the cervical spine), muscle relaxants (allow you to relieve spasm of the spinal muscles that impede venous outflow) can be used.
However, you should not bypass non-drug methods of treating the problem: exercise therapy, maintaining a correct lifestyle, limiting provoking factors (alcohol, bending work, etc.).
Venous encephalopathy, if diagnosed in a timely manner, responds quite well to treatment. Remember, your health is in your hands, and doctors can help restore it; it is only important to follow all the recommendations. Be healthy!
Treatment
Treatment of venous encephalopathy is always comprehensive and is aimed at eliminating both the underlying disease and concomitant ones. It is important to start by stopping the symptoms of the disease in order to alleviate the general condition.
Self-medication is dangerous with complications!
Attention
Despite the fact that our articles are based on trusted sources and have been tested by practicing doctors, the same symptoms can be signs of different diseases, and the disease may not proceed according to the textbook.
Pros of seeing a doctor:
- Only a specialist will prescribe suitable medications.
- Recovery will be easier and faster.
- The doctor will monitor the course of the disease and help avoid complications.
find a doctor
Do not try to treat yourself - consult a specialist.
At the first stage of the disease, treatment can be carried out at home, with a mandatory visit to a medical facility. All other stages require observation and treatment within the walls of a hospital.
Important in treatment are:
- regime ;
- physiotherapy ;
- physiotherapeutic procedures;
- breathing exercises;
- normalization of sleep;
- quitting smoking and alcohol;
- elimination of unfavorable psychotraumatic situations.
The main emphasis in treatment is on drug therapy, which includes:
- Drugs to maintain vascular - venotonics, are used in the form of tablets and infusions (intravenous administration).
- Diuretics are diuretics used to reduce intracranial pressure.
Vasoactive drugs are also used to improve blood supply to nerve tissue cells:
- myotropic antispasmodics, dilating blood vessels;
- angioprotectors that strengthen blood vessels and protect their walls from mechanical damage;
- metabolic agents that enhance energy processes in cells.
Treatment may also include, depending on risk factors:
- normalization of blood pressure;
- treatment of atherosclerosis, to reduce blood cholesterol;
- detoxification of the body using hemodialysis and hemoperfusion.
As the disease progresses, surgical treatment may be necessary. In case of thrombosis or purulent inflammation of the sinus, surgical treatment is performed.
The duration of treatment depends on the severity of the pathology. In severe cases, treatment takes up to 4 months; in mild cases, treatment takes about 1 month at home.
It should also be remembered that treatment with folk remedies for this disease is unacceptable.