Cysts of the pineal gland (epiphysis) are common, asymptomatic, and in most cases are an incidental finding. Cysts, especially large and atypical-looking ones, are difficult to distinguish from cystic tumors, so patients with suspicious changes should undergo long-term observation. On MRI or MRI, a pineal gland cyst appears as a single-chamber fluid formation with the density of cerebrospinal fluid or with a signal intensity similar to that of cerebrospinal fluid. Peripheral contrast enhancement is typical for most cysts, and rim-shaped calcifications are found in 25% of cases.
Get an MRI of the pineal gland in St. Petersburg
Symptoms of a pineal gland cyst
The vast majority of pineal gland cysts are small in size (in 80% of cases less than 1 cm) and are characterized by an asymptomatic course. Cysts that cause symptoms mainly occur in women in the second half of life. Larger cysts can cause a volumetric effect on the quadrigeminal plate, leading to compression of the superior colliculus and the occurrence of Parinaud's syndrome. When the cerebral aqueduct located between the third and fourth ventricles is compressed, obstructive hydrocephalus may develop. Rarely, if the cyst bleeds, it can quickly increase in size. This condition is called pineal cyst apoplexy.
A pineal gland cyst can cause headaches, blurred vision, and the inability to look up or down. Rare symptoms: ataxia, emotional disorders, disturbances in mental activity, dizziness, sleep disturbances, nausea, hormonal imbalance (early puberty, secondary parkinsonism).
Symptoms
Tumors of the pineal region of the brain are combined with the manifestation of symptoms such as:
- Severe headaches;
- Vomiting and nausea;
- Coordination problems;
- The occurrence of memory impairment;
- The gait changes;
- Certain visual disturbances, etc., may occur.
Most often, when there is a formation in the pineal region, its removal is prescribed. The operation can be performed with minimal trauma using endoscopic instruments. An open type process is also used (if the formation is large, elimination requires careful separation).
Brain lesions can be combined with fairly frequent manifestations of pain in the limbs, back, double vision may occur, etc.
Structure
The wall of a pineal cyst consists of three concentric layers:
- The inner layer is represented by fibrillary glial tissue, often with inclusions of hemosiderin
- The middle layer is the parenchyma of the pineal gland with or without calcifications
- The thin outer layer consists of connective (fibrous) tissue
Hormonal changes are thought to play a role in the formation of cysts, as they are most often found in young women. With age, cysts first increase in size and then “shrink.” In men, these formations remain in a stable state for a long time. Cysts usually contain proteinaceous fluid that differs from cerebrospinal fluid on CT scans; Sometimes blood is found in them. The walls of the cyst intensively accumulate contrast.
Diagnosis and treatment of brain cysts
The cost of surgery to remove a brain cyst depends on the type of disease and the diagnosis.
When examining a patient, computer or magnetic resonance imaging equipment must be used. Additionally, the heart and blood vessels of the brain are examined, blood pressure is checked, blood is donated for the presence of autoimmune and infectious diseases, coagulability and cholesterol levels. After receiving all the data, the neurosurgeon prescribes a course of treatment. If the tumor is dynamic, but is not accompanied by dangerous symptoms, medication is sufficient. The cost of medications is affordable in most cases. The main task of drugs is to eliminate the causes of the disease. For example, resorption of adhesions, restoration of blood circulation, reduction of cholesterol concentrations, normalization of blood pressure.
Important points in the treatment of cysts are considered to be: providing brain cells with glucose and oxygen, increasing their resistance to intracranial pressure, and solving problems such as weakened immunity. When detecting infectious diseases, special attention is paid to this issue. If you miss this moment, you may end up paying a high price, because the situation will definitely get worse.
What does a pineal gland cyst look like on CT and MRI?
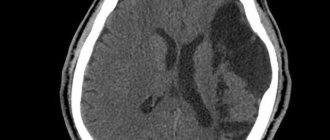
Computed tomography visualizes a fluid-dense mass with well-defined edges and peripheral calcifications found in 25% of patients. In many cases, there is also a peripheral accumulation of contrast in the cyst in the form of a thin and smooth “rim”. The cyst disrupts the course of the internal veins of the brain, displacing them upward.
Pineal cyst with a typical hyperintense signal on MRI (T2 WI) (marked with a blue arrow). Left: axial tomogram, right – sagittal
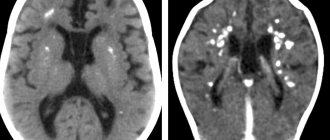
The following signs are observed on MRI:
- T1 VI
- Typical iso- or hypointense signal compared to brain parenchyma
- The signal is usually uniform
In 55–60% of cases, the signal is hyperintense compared to the cerebrospinal fluid
- High intensity signal
- High intensity signal that is often not completely suppressed
- There is no diffusion restriction
- Approximately 60% of cysts accumulate contrast
Treatment of pineal brain tumor
Treatment is prescribed based on the examinations performed. If the pineal region is affected, all laboratory tests and tumor markers must be taken, after which CT and MRI are prescribed. Having received the examination results, the doctor can clearly determine the sequence of actions. Most often, surgery is required, and removal is done as quickly as possible. Pineal brain tumors can be quite large, making the treatment process extremely difficult. Often it is simply impossible to remove such a lesion due to the possibility of causing irreparable harm to the patient.
When prescribing treatment, the doctor must focus on the general clinical picture, use the maximum diagnostic process, assess the general condition of the patient, and determine the possibility of eliminating the formation without causing harm. If traditional methods of therapy, in the opinion of the doctor, do not give the desired result, one should resort to the use of a surgical process in combination with chemotherapy, medications, radiotherapy, etc.
How to distinguish a pineal cyst from a tumor?
A pineal cyst, especially one with nodular contrast enhancement, cannot be differentiated from a cystic pineocytoma based on imaging techniques alone. Other formations may also occur in the pineal area: papillary tumor, germinoma, embryonal cancer, choriocarcinoma, teratoma, epidermoid cyst, arachnoid cyst, vein of Galen aneurysm, metastases.
Although such cases are rare, it is always best to have the results examined by an experienced neuroradiologist. Rechecking CT or MRI images will help you more accurately understand whether a tumor is suspected. Today this can be done remotely using Second Medical Opinion services, such as the National Teleradiological Network.
Common types of brain cysts:
- retrocerebellar (occurs directly in the brain, namely in places where gray matter cells die);
- arachnoid (forms between the layers of the membranes of the brain filled with cerebrospinal fluid);
- subarachnoid (most often a congenital pathology, accompanied by pulsation in the cranium and painful muscle contraction);
- pineal (appears in the pineal gland and in the area where the hemispheres connect; has a direct effect on the endocrine system);
- pineal (diagnosed in the pineal gland, leads to impaired coordination of movement, vision, and metabolic processes).
There are cysts of the choroid plexuses of the brain, the pineal gland, located between the meninges, in the subcortical ganglia, cerebellum and even the visual thalamus.
Treatment of pineal cyst
In almost all cases there is no need for treatment; in most cases, small cysts do not require follow-up studies. Depending on the size and location of the cyst, as well as symptoms, treatment may consist of stereotactic removal of the cyst, aspiration of its contents, creation of a connection with the cerebrospinal fluid spaces, and shunting. If the cyst recurs after treatment, radiation therapy is possible.
Get an MRI of the pineal gland in St. Petersburg
Life forecast
A tumor of the pineal region of the brain can be benign if it is diagnosed at an early stage, and the treatment is comprehensive and prompt, that is, there is a chance of returning the patient to normal life.
If the tumor of the pineal region of the brain is malignant, then in this case treatment should include removal, chemotherapy, radiation, etc. In the early stages, treatment gives positive results, but relapse is possible in 20-25% of cases. If the formation is large and in the last stage of development, then even after removal, relapse is possible in 30-45%, and in some cases it is impossible to perform surgery.
Publications in the media
Tumors of the pineal gland parenchyma (PGT) develop from pinealocyte precursors (cells with photosensitive and neuroendocrine functions) of varying degrees of differentiation. They are characterized by localization in the pineal region (posterior sections of the third ventricle). OPSH make up about 14–30% of all tumors of the pineal region (another large group of this localization consists of germ cell tumors (see CNS germ cell tumors).
Classification: There are three types of tumors • Pineocytoma (WHO-2) is a slow-growing tumor consisting of mature pinealocytes. Makes up approximately 45% of all OPSH. Equally often detected in men and women, the peak incidence occurs at the age of 25–30 years • Pineoblastoma (WHO-4) is a highly malignant tumor consisting of poorly differentiated cells of the pineocytic series. Makes up approximately 45% of all OPSH. In its biological properties and aggressiveness, it is very similar to a supratentorial primitive non-euroectodermal tumor (see Embryonic tumors of the central nervous system), in particular, it has a tendency to metastasize in the subarachnoid spaces. The tumor is detected mainly in children, although cases of occurrence at almost any age have been described. Develops somewhat more often in males • Tumor of the parenchyma of the pineal gland of intermediate differentiation (WHO-3) is characterized by the least predictable course. Makes up approximately 10% of all OPSHH. More often develops in adults.
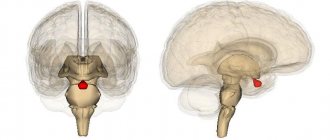
Anatomical localization : pineal region (posterior parts of the third ventricle, area of the quadrigeminal cistern).
Clinical picture : depends both on the location of the tumor and on its histological type. Symptoms of occlusive hydrocephalus and midbrain syndrome (oculomotor disorders) are characteristic. Slowly growing pineocytoma is characterized by a slow increase in the severity of symptoms and long-term relatively satisfactory health of the patient; for pineoblastoma - rapid progression of the disease and deterioration of the neurological status. Multiple neurological symptoms (including spinal) develop when the tumor metastasizes through the subarachnoid spaces.
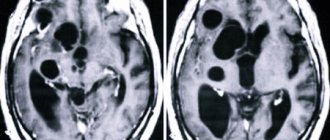
Diagnosis: Contrast-enhanced MRI is the standard examination for tumors of this location. With pineocytoma, a small, rounded formation is found in the pineal region, with clear boundaries, actively and homogeneously accumulating contrast and causing compression of the quadrigeminal plate. Pineoblastoma is characterized by all the signs of a malignant, rapidly progressing tumor (infiltrative growth pattern, heterogeneous signal with signs of necrosis and hemorrhage, large size, subarachnoid metastases).
Treatment depends on the histological diagnosis • Pineocytoma - radical removal of the tumor • Pineoblastoma - tumor resection (as radical as possible, but not to the detriment of the patient's neurological status) in combination with radiation therapy. If necessary, shunt surgery or endoscopic ventriculostomy of the third ventricle is performed. The effectiveness of chemotherapy has not been proven • In case of intermediate-grade opacitis, the treatment tactics are similar to those for pineoblastoma. Forecast. With pineocytoma, radical surgical removal of the tumor cures the patient. With subtotal/partial removal, the 5-year survival rate is 86%. With complex treatment of pineoblastoma, 1, 3 and 5-year survival rates are 88%, 78% and 58%, respectively. The prognosis for intermediate differentiation OPSH is the least predictable, but closer to that for pineoblastoma.
Abbreviations: OPSH - tumors of the parenchyma of the pineal gland . Synonym. Pineal adenoma
ICD-10 • C71 Malignant neoplasm of the brain • D33 Benign neoplasm of the brain and other parts of the central nervous system