Using magnetic resonance imaging, you can assess the condition of blood vessels, determine the size of the lumen and the tone of the walls of arteries and veins. MRI also allows you to track the processes of thrombus formation in blood vessels. To do this, the method of special sequences is used or contrast enhancement is used with a solution of gadolinium salts, which are administered to the patient intravenously.
MRI is one of the methods of modern diagnostics, based on the influence of an external magnetic field on the dipole of water located in cells. The caused resonance of hydrogen atoms (change in position) is recorded by tomograph sensors. This signal is converted into a photographic image using a special computer program. A whole series of photographs is displayed on the computer screen, and all this is due to the fact that scanning is carried out in 3 projections: frontal, sagittal and axial. Using such images, a 3-dimensional image of the area under study is obtained.
What are blood clots and why do they appear?
Thrombi are clots that form from connections between blood cells. Platelets, sticking together in chains, form lumps that are attached to the walls of blood vessels. In some situations, blood clots form due to disorders of the hematopoietic system, in others - as a result of damage to the inner wall of the vessel.
Large growths inside the vein prevent blood flow from passing through the obstructed area. As a result, congestion forms in the veins, leading to varicose veins. When a blood clot blocks the lumen, a heart attack occurs—the death of tissue that has not received oxygen through the bloodstream.
The formation of blood clots is influenced by several factors from a person’s daily life:
- Sedentary lifestyle. Lack of active mobility leads to stagnation of blood in the lower legs. Therefore, constantly sitting at a computer, as well as choosing an escalator instead of stairs, give the blood a reason to stagnate and form clots.
- Insufficient fluid intake. The quality of blood directly depends on what a person eats. With insufficient fluid intake, the blood becomes thick, which means it cannot fully perform its functions and puts a greater strain on the heart. It is easy to pump liquid blood through the system, but thick blood is much more difficult.
- Taking medications that affect the hematopoietic system. In medical practice, drugs are often used to treat certain diseases, one of the side effects of which is blood thickening. Therefore, such medications must be taken simultaneously with anticoagulants that prevent the formation of blood clots.
You can protect yourself from blood clots by regularly exposing your body to physical activity, drinking enough fluids, and including more plant-based foods rich in fiber in your diet.
Why do blood clots form in the body?
The process of blood clotting is a protective reaction that occurs in response to damage to the vessel. The clot is a biological “bandage” that dissolves over time (fibrinolysis). Thrombosis (formation of blood plugs in the lumen of a vessel) occurs in the following pathological conditions of the body:
- hypercoagulability;
- damage to endothelial cells;
- change in the nature of blood flow.
If the hemostasis system is disrupted, the blood coagulation process accelerates and the activity of fibrinolysis decreases. There is a layering of thrombotic masses, an increase in the size of the clot and occlusion of the vessel. In some cases, the formation breaks away from the inner surface of the wall and moves with the blood flow, which leads to embolism of veins and arteries. This term refers to the presence and circulation of particles that are not normally found in the said liquid medium.
Embolism is one of the causes of stenosis (narrowing) and occlusion (impaired patency) of blood vessels. Thrombosis of the veins of the lower extremities and pelvis is observed most often, which is associated with the structural features and physiology of the human body.
Factors that provoke the formation of blood clots in the body:
- injuries accompanied by a violation of the integrity of the vascular wall;
- surgical interventions;
- taking hormonal drugs, contraceptives, antihypertensive drugs;
- obesity;
- metabolic disease;
- elderly age;
- pregnancy;
- endocrine disorders;
- phlebeurysm;
- low physical activity;
- malignant neoplasms;
- infective endocarditis.
Early diagnosis of thrombosis allows you to choose an effective treatment method and prevent the development of dangerous complications (pulmonary embolism, etc.)
How do blood clots occur?
If a blood clot has formed on the wall of an artery, its appearance can be described in the following stages:
- Some process damages the artery wall.
- The body notices the violation and begins to build protection against blood loss, forming a large number of special blood cells - platelets, which, attaching to the damaged area, form a kind of patch.
- In case of coagulation disorders or changes in the hematopoietic system, platelet formation does not stop on time and continues longer than expected. This causes too much growth to form on the wall. Or platelets, which are in small quantities in the blood, floating past in the bloodstream, stick to the resulting accumulation.
The causes of damage to the walls of blood vessels can be:
- mechanical disruption of the structure due to injury;
- infectious lesion;
- high levels of glucose molecules in the blood;
- immune system dysfunction.
If there are no factors that contribute to the formation of blood clots, any injury or other damage will not lead to a large accumulation of blood cells. Under the layer of platelets, the artery wall will heal and recover, and the crust will resolve over time.
There are several stages of thrombus formation:
- disruption of the structure of the inner surface of the artery;
- activation of blood clotting factors;
- platelet adhesion at the site of injury;
- the appearance of substances that trigger a chain of reactions that form fibrin threads, which contribute to thrombus formation;
- a kind of network of fibrin threads is formed, into which blood cells enter, creating a large clot;
- Over time, the clot thickens, forming a thrombus.
When a blood clot breaks off under the influence of any factors, it begins to move through the bloodstream. Once it hits the nearest bottleneck, the blood flow will be blocked. If a similar situation happens outside a medical facility, it is impossible to save the person.
The effectiveness of MRI and the complete picture of the disease
In addition to visualizing the formation, MRI allows you to answer a number of questions:
- size and location of the blood clot;
- the presence of an embolus in the bloodstream;
- degree of patency of arteries and veins.
Another important point is that magnetic resonance imaging reveals some of the causes of pathologies. So, it will help to identify malignant formations in the surrounding tissues that put pressure on the blood vessels. If the patient has thrombophlebitis, then it is possible to analyze the characteristics of inflammation of the venous wall, such as thickening, changes in its structure, etc.
Unlike other diagnostic methods, magnetic resonance imaging provides a complete picture of the patient’s condition. The doctor sees small blood clots and simply blood clots that are located in any blood vessels, be it deep veins, the brain, internal organs or lower extremities. The three-dimensional image shows not only the problem areas, the degree of damage, but also, most importantly, the interaction with surrounding tissues.
Control examinations at intermediate stages of treatment
The examination is also important in light of the fact that when a tumor is detected that provokes the formation of a clot and disruption of blood flow, it is possible to assess the consequences of the development of the formation and predict the further course of the disease. The doctor sees foci of ischemia, as well as collaterals in the examined area. MRI is performed not only for making a primary diagnosis. Control examinations are prescribed to evaluate the effect of the chosen course of treatment and make decisions regarding further actions.
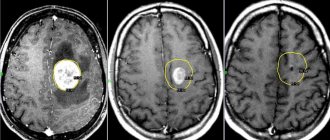
Visualization of blood clots on the tomograph screen
The image displayed on the tomograph screen differs from the image obtained with ultrasound or other research methods. The doctor receives layer-by-layer images of the area of the circulatory system of interest. Thanks to a cut-off pitch of 1 mm, even very small clots are clearly visible on the screen. The presence of an embolism is indicated by the fact that the signal becomes more intense, while in normal areas it returns evenly. Also, a visual image of a blood clot appears on the screen and has a different appearance.
Examination methods and view of blood clots on the screen
Examination of the circulatory system for problems with blood flow is carried out using two methods, which determine the type of clots:
- T1 weighted image;
- T2 weighted image.
Visually, the thrombus has a rounded shape; at the point of attachment to the vessel or with complete occlusion, it becomes denser. Its color depends on the examination method used. At T1 VI it has a neutral color, after which it becomes lighter. For the acute stage of a blood clot (the first 12 hours), T2 VI is used, in this case the clot is dark in color. But these are general characteristics, decoding is carried out by a qualified specialist, and without it it is impossible to begin a course of treatment.
Thrombosis factors
An increased risk of blood clots is caused by:
- Genetic inheritance to predisposition.
- Diseases that force you to limit physical activity, for example, bed rest.
- High degree of blood clotting.
- Arrhythmia, cardiomyopathy and other diseases that disrupt the strength and rhythm of blood flow throughout the system.
- Varicose veins.
- Liver dysfunction.
- Alcoholism.
- Smoking.
- High body mass index.
- Age-related changes in hormone levels in both men and women.
Some of these factors cannot be influenced, for example, genetic predisposition. However, you can protect yourself from the serious consequences of blood clots by maintaining an active and healthy lifestyle.
Can an MRI show blood clots?
MRI can easily be considered one of the informative methods for diagnosing pathologies associated with blood vessels.
But this method is not as accurate as CT angiography, because blood clots can only be detected by indirect signs. To improve visualization, a contrast solution is used. Contrast, which is gadolinium salts, is injected into the vessel at the lumen site. Due to the lack of normal blood flow at the site of the thrombus, the contrast agent sharply slows down its movement or demonstrates the presence of a parietal defect. But sometimes this contrast behavior can be caused not only by the presence of a clot, but also by other reasons.
MRI shows:
- The presence of a thrombus and its localization in the vessel.
- The size of the blood clot and how tightly it adheres to the vessel wall.
- The presence of emboli in the bloodstream.
- Vascular patency.
In the presence of thrombophlebitis, a tomogram will show the degree of inflammation of the walls of the venous vessels, i.e. How thick are they, are there any delaminations, structural changes, etc.
The scan will allow you to assess the condition of the soft tissues that surround the vessel and determine the influence of external factors on the blood flow (for example, pressure on the vessel from a growing tumor). Diagnosis of thrombosis using MRI will allow one to calculate the consequences of the pathological process and clearly show foci of collateral and ischemia in the area under study.
In volumetric images obtained using MRI of the extremity, even small-sized blood clots localized in the vessels of the lower extremities and deep veins, life-supporting organs and the brain are clearly visible. This instrumental method makes it possible to obtain a visual representation of the state of areas of the circulatory system and analyze the influence of surrounding tissues on them.
To determine the effectiveness of treatment associated with the normalization of hemostasis, control scans are performed periodically.
Thrombophlebitis - symptoms and treatment
Therapeutic and preventive measures for thrombophlebitis are complex and can be conservative and surgical. The main objectives are to maximize the elimination of risk factors, reduce and alleviate local symptoms in acute thrombophlebitis, prevent the spread of thrombophlebitis to the deep vein network and prevent venous thromboembolic complications.
Surgical treatment
Not long ago, the gold standard for the treatment of ascending thrombophlebitis was crossectomy (Troyanov-Trendelenburg operation), but practice results have shown that this method of surgical intervention is the most traumatic and life-threatening for patients.
When the process goes beyond the sapheno-femoral or sapheno-popliteal anastomosis, thrombectomy is performed from the main veins. Surgery can be performed using regional anesthesia or intubation endotracheal anesthesia. The preference for thrombectomy method depends on the level of location of the proximal part of the thrombus.
In case of perforator thrombosis, thrombectomy from the perforator vein is performed. In case of embolic thrombosis of the femoropopliteal segment, ligation of the superficial femoral vein (SFE) is indicated.
In case of embolic-dangerous iliocaval thrombosis, plication of the inferior vena cava is performed.
The figure shows the implantation of a vena cava filter into the inferior vena cava, the indication for which is embolic iliocaval thrombosis.
Laser treatment
According to the latest revised clinical guidelines, endovenous laser coagulation (EVLC) is a low-traumatic and safe technique for ascending thrombophlebitis. This method can be used to operate on any category of patients. As a rule, surgery is performed under local tumescent anesthesia.
Conservative treatment
Today, for existing indications, the most effective method will be anticoagulant therapy. In medical practice, it is customary to distinguish between direct-acting anticoagulants, which help reduce thrombin activity in the blood, and indirect-acting anticoagulants, which prevent the formation of prothrombin in the liver. Low molecular weight heparins belong to the group of direct-acting anticoagulants. These include medications such as Enoxaparin sodium (Anfibra, Clexane, Hemapaxan, Lovenox), Dalteparin (Fragmina) or Tinzaparin, which must be administered subcutaneously 1-2 times during the day. The use of low molecular weight heparins results in maximum effectiveness and minimal side effects. Indirect anticoagulants are Warfarin derivatives, which require special caution and a high degree of laboratory control (INR). Currently, the greatest interest is in drugs that do not require laboratory monitoring of INR and with lower risks of complications, for example, such as Xarelto (Rivaroxaban) or Pradaxa.
In addition, the patient is prescribed long-term wearing of compression hosiery and auxiliary pharmacotherapy, phlebotonic drugs (Detralex; Venarus; Phlebodia 600), etc. It is also advisable to prescribe non-steroidal anti-inflammatory drugs and local treatment.
Treatment of thrombophlebitis of superficial veins and acute thrombophlebitis
Recently, international consensus has accepted the equality between the terms “acute thrombophlebitis” and “thrombophlebitis of the superficial veins”, which determines the commonality of pathogenetic mechanisms, complications and treatment tactics.
Physiotherapeutic treatment
Intermittent pneumocompression is a physiotherapeutic method of massaging tissue using special multi-chamber cuffs with different operating pressures. This technique has excellent lymphatic drainage properties, helps reduce swelling and can be used for thrombophlebitis of the veins of the lower extremities.
Electromyostimulation using the VENOPLUS device - this patented technique consists in the fact that electromyostimulation leads to muscle contraction and activation of the muscle-venous pump. It can also be used for thrombophlebitis of the veins of the lower extremities.
Gymnastics for thrombophlebitis
This disease poses a threat to life if a blood clot breaks off, so gymnastics is contraindicated.
Leeches for thrombophlebitis
Currently, the first line of therapy is the use of low molecular weight heparins. Hirudotherapy has a much lower effect.
Ointments for thrombophlebitis
The use of ointments is possible in the complex treatment of thrombophlebitis. NSAIDs are used in the form of ointments to relieve pain. Such ointments include Fastum Gel, diclofenac, ortofen and others. It is also possible to use ointments with heparin (Lioton, hepatrombin).
Nutrition for thrombophlebitis
Nutrition does not affect the course of thrombophlebitis. It is worth adjusting the diet only if the disease occurs against the background of obesity.
Can folk remedies help?
Decoctions, tinctures and compresses have no proven effectiveness and therefore cannot be recommended for the treatment of thrombophlebitis. Thrombophlebitis is a disease that can threaten the patient’s life and therefore requires immediate and adequate treatment.
Rehabilitation
Rehabilitation usually takes place at home. Compliance with any special regime is not required. If the patient smokes, he should stop smoking if possible.