Hippocampal sclerosis is a form of epilepsy caused by pathology of the limbic system of the brain. The main generator of epileptic activity is considered to be gliosis in combination with atrophy of the cortical plate of the underlying white matter. To diagnose the disease, neurologists at the Yusupov Hospital use modern instrumental research methods, perform laboratory tests and minimally invasive diagnostic procedures.
Hippocampal sclerosis is accompanied by loss of neurons and scarring of the deepest part of the temporal lobe. Often caused by serious brain injuries. It can be left-handed or right-handed. Brain damage due to injury, neoplasm, infection, lack of oxygen, or uncontrolled spontaneous seizures results in the formation of scar tissue in the hippocampus. It begins to atrophy, neurons die and form scar tissue.
Based on structural changes, two main types of temporal lobe epilepsy are distinguished:
- with the presence of a volumetric process (tumor, congenital pathology, aneurysm of a blood vessel, hemorrhage) affecting the limbic system;
- without the presence of clearly verified volumetric changes in the medial temporal lobe.
Hippocampal sclerosis - what is it?
Hippocampal sclerosis is a form of epilepsy that is characterized by a decrease in the volume of nervous tissue and loss of neurons in the medial temporal lobe. Clinically, this pathological process is manifested by attacks of epilepsy. Sometimes this condition can be controlled with medication, but in some cases surgery may be required.
Hippocampal sclerosis often occurs in older people after a stroke. At risk are those people who suffer from high blood pressure or diabetes.
Temporal lobe epilepsy – Hippocampal sclerosis
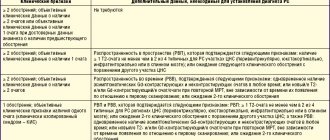
It is one of the most common types of epilepsy, accounting for about 20% of those with epilepsy and 65% of those with temporal lobe epilepsy. Eighty percent of patients with mesial temporal lobe epilepsy have hippocampal sclerosis. Febrile seizures in childhood are common and occur in 60% of cases of hippocampal sclerosis, of which 35% are complex febrile seizures. Unusually prolonged febrile seizures are characteristic of future temporal lobe epilepsy. The development of hippocampal sclerosis may have a genetic component. Hippocampal sclerosis is the most common cause of structural temporal lobe epilepsy. The cause of hippocampal sclerosis remains unknown. There are several hypothesized mechanisms for damage to hippocampal nerve cells: developmental abnormalities, an autoimmune mechanism, and damage due to overstimulation resulting from frequent or prolonged epileptic seizures. Research shows that with hippocampal sclerosis, changes in brain tissue extend beyond the hippocampus.
Symptoms of Structural Mesial Temporal Temporal Epilepsy
Ascending Epigastric Discomfort The most typical epileptic phenomenon of the structural form of mesial temporal lobe epilepsy is “ascending epigastric discomfort” combined with a feeling of fear. Patients describe this sensation as a strange, nauseating, empty, unpleasant sensation that begins in the upper abdomen and gradually moves higher and higher. This particular type of seizure is not typical of the genetic form of mesial temporal lobe epilepsy. Automatisms Automatisms are repeated, stereotyped, aimless movements, such as chewing, smacking, fingering, or movements that imitate picking up small objects with the fingers. Automatisms occur in seventy percent of those suffering from mesial structural epilepsy. Automatisms can be bilateral or limited to one side. Complex Partial Seizures This type of epileptic seizure involves the cessation of normal activity. The eyes are pointlessly directed into infinity. In this case, automatisms are typical. At the moment of a seizure, there is no reaction to the environment, as well as no awareness of what is happening. Typically, complex partial seizures last from 30 seconds to 2 minutes. They are often confused with absence seizures. Sometimes a seizure can drag on and turn into status epilepticus, i.e. continuous seizure. Other Types of Seizures Phenomena of false perception, such as: deja vu - already seen, jamais vu - never seen, taste or olfactory hallucinations, are not typical for mesial temporal lobe epilepsy. Secondary generalized tonic-clonic seizures, usually untreated, and postconvulsive brain fog are typical.
Diagnosis of Mesial Temporal Temporal Epilepsy
Brain MRI demonstrates hippocampal sclerosis. Sometimes, in addition, abnormalities in brain development can be detected. Electroencephalography (EEG) in half of the cases shows nothing on the first recording. In only a third of the subjects, a classic peak-wave epileptic focus in the temporal lobe can be detected. Long-term recording and recording after sleep deprivation increases EEG sensitivity by up to 80%. The EEG during a seizure demonstrates rhythmic 4-7 Hz slow wave activity in the temporal lobe.
Prognosis and Treatment for Structural Mesial Temporal Temporal Epilepsy
In each specific case, the prognosis is unpredictable. In some patients, the initially good results of treatment with antiepileptic drugs are lost over time, which leads to an increase in the frequency and worsening of the severity of epileptic seizures. Severe temporal lobe epilepsy can lead to memory loss, cognitive decline, and psychological disturbances. However, in most cases, seizures in hippocampal sclerosis can be well controlled for years in most patients. Any of the drugs or a combination of drugs described at the very end of this page can be used in the treatment of structural mesial epilepsy. Carbamazepine, however, is more effective than others. The choice of medications is also dictated by age, gender and comorbidities. In cases of uncontrolled structural mesial temporal lobe epilepsy, surgical treatment becomes appropriate. Surgical treatment in 60% of cases leads to complete remission; in 10% – the effect is zero; and in 20% the severity of seizures is reduced to varying degrees. Surgery involves removing a significant portion of the temporal lobe. For this reason, surgical complications are not very uncommon and amount to about 10%. The most common are speech and memory disorders and worsening severity of epilepsy.
Why choose MRI?
For pathologies localized in the brain, doctors recommend choosing magnetic resonance imaging. This is due to a number of advantages of the technique:
- Thanks to MRI, it is possible to obtain a number of images, including cross-sectional images.
- High image quality and detail.
- If necessary, a contrast agent can be used, which increases the information content of magnetic resonance imaging.
- This type of diagnosis has a small list of contraindications and does not cause any side effects.
- The procedure is completely non-invasive. Accordingly, the research process does not cause pain or discomfort.
- Magnetic resonance imaging is considered absolutely safe because it excludes exposure to radiation to the body.
- Possibility of identifying a pathological process even at an early stage of development.
The essence of the pathological process
With the development of sclerosis, unaffected organs and soft tissues are replaced by connective tissue that has a dense structure. This mechanism can be provoked by factors such as the development of the inflammatory process, age, deterioration of the immune system and addictions. In this regard, taking into account the area of development of the pathological process, tuberous or atherosclerosis, cerebral vascular sclerosis, etc. are distinguished.
Indications for the study
As mentioned above, the most informative method for diagnosing hippocampal sclerosis is magnetic resonance imaging. As a rule, a referral for research is issued by a neurologist, less often by a psychiatrist or oncologist. MRI of the hippocampus is most often part of a comprehensive diagnosis of the brain, but in some cases the doctor may prescribe a study of this particular area.
The study is prescribed for obvious signs of this pathological process.
The main symptom of hippocampal sclerosis is epileptic seizures. This condition may cause additional symptoms, for example:
- Severe memory loss.
- Periodic convulsions.
- The occurrence of panic attacks.
- Insomnia.
- Frequent headaches that do not go away even after taking painkillers.
- Dizziness may occur from time to time.
- Impaired concentration.
- Intellectual thinking suffers.
Magnetic resonance imaging can also be prescribed before surgery to clarify the location of the pathological focus. Diagnosis is also carried out in the postoperative period.
Diagnostic measures
Neurologists are involved in diagnosing this condition. It is this specialist who should be contacted if the clinical picture described above manifests itself. During the first visit, the attending physician will talk with the patient to obtain a medical history. During the dialogue, the doctor assesses the patient’s intellectual capabilities and determines behavioral traits. If emotional or intellectual abnormalities are detected, the patient is referred for examination to a psychiatrist.
Along with this, the medical specialist will undertake a number of manipulations to assess the patient’s reflexes:
- in the knee joint;
- in the carpal-radial joint;
- as well as the reflex function of the biceps muscles of the shoulders.
During the diagnosis, the patient undergoes the following studies:
- An electroencephalogram allows you to identify existing foci of pathological impulses in the brain.
- CT and MRI make it possible to take a layer-by-layer image of the brain and other structures of the skull.
- Angiography determines the presence of disturbances in the blood flow of the brain.
- ECHO is an encephalogram, which is important if the patients are newborns or young children.
Contraindications
Before diagnostics, you should make sure that you have no contraindications to MRI.
Magnetic resonance imaging is not performed in the following cases:
- The presence of a pacemaker or metal structures in the body (non-removable type).
- Women do not undergo MRI during the first trimester of pregnancy; diagnosis can only be carried out as prescribed by a doctor.
- Magnetic resonance imaging in a closed tomograph is not performed if you are afraid of closed spaces.
- It is not recommended to do an MRI if there are serious abnormalities in the functioning of the nervous system or psyche.
If there is a need to use a contrast agent, you should ensure that:
- An allergic reaction to the drug used.
- Kidney or liver failure.
- Pregnancy and lactation.
Preventive actions
In order to reduce the frequency of seizures, experts recommend regularly taking prescribed medications, as well as:
- Follow a rest and sleep schedule; you need to go to bed and wake up at the same time.
- Adhere to a diet that includes limiting the consumption of spicy, salty and fried foods, as well as liquids.
- Avoid consuming alcoholic beverages; alcohol-containing products lead to the development of many different diseases.
- Eliminate the consumption of tobacco products - tobacco and combustion products negatively affect all body systems.
- Avoid overheating or hypothermia of the body; to do this, you should avoid visiting baths and saunas, and sunbathing in the open sun.
- Eliminate consumption of tea and coffee.
Preparation rules
Here are some tips for preparing for a magnetic resonance imaging scan:
How is an MRI done?
Magnetic resonance imaging is performed in a special diagnostic room with a closed-type tomograph. Before starting the study, the specialist will tell you about some of the features of magnetic resonance imaging:
- The patient's main task is to remain still. Even the slightest body movements can lead to blurred images and a decrease in the information content of the procedure.
- If loud noises frighten you, it is better to take earplugs with you, as there is a loud noise during operation of the tomograph.
- If you feel unwell during the examination, you have the opportunity to pause the examination at any time by pressing the panic button.
Let's take a step-by-step look at how magnetic resonance imaging works:
- First, the patient must change into clothes without metal fittings - hospital clothes or his own.
- You need to take off your shoes and lie on your back on a retractable table.
- If necessary, a contrast agent is injected into the vein.
- The lower and upper limbs are secured with soft straps.
- The table automatically moves inside the tomograph.
- The duration of the diagnostic study is from 30 to 40 minutes.
At the end of the diagnosis, you need to wait for the results of the examination. If necessary, tell your doctor that you want your results digitally.
MRI with contrast
In most cases, the diagnosis of hippocampal sclerosis is carried out with an additional contrast agent. This makes it possible to get more informative and clear pictures. The contrast agent is injected into the patient’s vein immediately before the start of the diagnosis. MRI with contrast is completely safe for the body. The contrast does not accumulate in the tissues; within 24 hours the drug is completely eliminated from the body. To speed up this process, it is recommended to drink more water. Before MRI with contrast, it is necessary to consult a doctor and exclude contraindications.
Therapeutic measures
Anticonvulsants are mainly used to treat hippocampal sclerosis. In this case, only the attending physician should prescribe the intake and dosage of the drug. Self-treatment in this situation is excluded.
It is important to note that the absence of seizures indicates that the patient is recovering. The dosage of drugs in this case is reduced if there are no seizures for 2 years. Cancellation of medications is allowed only if seizures are completely absent for 5 years. In this situation, drug treatment is designed to ensure overall recovery.
Decoding the results
After all the images are received, the doctor’s task is to correctly interpret them and make a diagnosis. Using magnetic resonance imaging, you can find out the exact dimensions of a given part of the brain and identify even minimal changes in the structures of the hippocampus and neighboring areas. Detailed photographs of this area of the brain of the organ give your doctor the opportunity to determine the diagnosis and treatment tactics.
We recommend seeking medical help as soon as the first warning signs appear. Be healthy!