Article:
In early childhood, neuropsychiatric disorders such as tics are quite common.
The scientific name is tic hyperkinesis. Parents immediately notice changes in the baby’s behavior. Uncontrolled movements of certain parts of the body or certain muscles in a child cannot but become a cause for concern and questions arise:
- Where did the disease come from?
- Could it have been prevented?
- What to do?
- How to treat?
This list can go on for a long time. One thing is clear - there is certainly cause for concern. And the first thing you need to do is find out as much information as possible about this neurological disorder.
So what are nervous tics in children and what is their danger?
GENERAL CONCEPT OF TIKS
This is the most popular pathology of the children's nervous system at an early age. It is simply impossible not to visually notice the manifestation of a tic, although some parents manage to go for weeks or even months without seeing any oddities in their child’s behavior.
Tics are involuntary, stereotypically repetitive, sudden or jerky movements that are the result of spontaneous contraction of individual muscles or groups of muscles.
At the initial stage of development of the disorder, attacks occur quite rarely, and repetitive movements do not cause much concern or problems. The child can even restrain or control them. However, attempts to control the tic cause him:
- internal discomfort;
- feeling of anxiety;
- mental stress.
When control over oneself weakens, tic manifestations occur, and the baby immediately receives obvious relief.
Nervous tics in children are usually detected between the ages of two and fifteen years. In the period of 6–8 years, tic hyperkinesis most often develops, while at 14–15, in approximately half of the cases it disappears spontaneously.
Fun fact: Boys are five times more likely to have the disorder than girls. From a scientific point of view, this is explained by the more stable psyche of female representatives.
Causes of tics, diagnosis of tics and treatment of tics.
Tics are lightning-fast involuntary contractions of muscles, most often of the face and limbs (blinking, raising eyebrows, twitching the cheek, corner of the mouth, shrugging, shuddering, etc.).
In terms of frequency, tics occupy one of the leading places among neurological diseases of childhood. Tics occur in 11% of girls and 13% of boys. Under the age of 10 years, tics occur in 20% of children (i.e., every fifth child). Tics appear in children aged 2 to 18 years, but there are 2 peaks - 3 years and 7-11 years.
A distinctive feature of tics from convulsive muscle contractions in other diseases: a child can reproduce and partially control tics; tics do not occur with voluntary movements (for example, when picking up a cup and drinking from it). The severity of tics may vary depending on the time of year, day, mood, and nature of activities. Their localization also changes (for example, a child experienced involuntary blinking, which after some time was replaced by an involuntary shrug), and this does not indicate a new disease, but a relapse (repetition) of an existing disorder. Typically, tics intensify when a child watches TV or stays in one position for a long time (for example, while sitting in class or in public transport). Tics weaken and even disappear completely during gameplay or when performing an interesting task that requires full concentration (for example, reading an exciting story). As soon as the child loses interest in his activities, tics appear again with increasing force. The child can suppress tics for a short time, but this requires great self-control and subsequent release.
Psychologically, children with tics are characterized by:
attention disorders;
disturbance of perception;
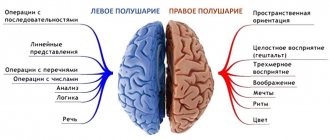
Children with severe tics show impaired spatial perception.
In children with tics, the development of motor skills and coordinated movements is difficult, the smoothness of movements is impaired, and the execution of motor acts is slowed down.
Classification of ticks:
motor tics (blinking, cheek twitching, shrugging, nasal tension, etc.)
vocal tics (coughing, snoring, grunting, sniffling)
rituals (walking in a circle)
generalized forms of tics (when one child has not one tic, but several).
In addition, there are simple tics, involving only the muscles of the eyelids or arms, or legs, and complex tics - movements simultaneously occur in different muscle groups.
Tick flow
The disease can last from several hours to many years.
The severity of tics varies from almost imperceptible to severe (leading to the inability to go outside).
The frequency of tics varies throughout the day.
Treatment effectiveness: from complete cure to ineffectiveness.
Associated behavioral disturbances may be subtle or severe.
Causes of tics
There is a widespread view among parents and teachers that “nervous” children suffer from tics. However, it is known that all children are “nervous,” especially during periods of so-called crisis (periods of active struggle for independence), for example, 3 years old and 6-7 years old, and tics appear only in some children.
Tics are often combined with hyperactive behavior and attention deficit disorder (ADHD), low mood (depression), anxiety, ritualistic and obsessive behavior (hair pulling or wrapping it around a finger, nail biting, etc.). In addition, a child with tics usually cannot tolerate transport and stuffy rooms, gets tired quickly, gets tired of sights and activities, sleeps restlessly or has trouble falling asleep.
The role of heredity
Tics appear in children with a hereditary predisposition: parents or relatives of children with tics may themselves suffer from obsessive movements or thoughts. It has been scientifically proven that tics:
are more easily provoked in males;
boys suffer from tics more severely than girls;
Children develop tics at an earlier age than their parents;
If a child has tics, it is often discovered that his male relatives also suffer from tics, and his female relatives suffer from obsessive-compulsive disorder.
Parental behavior
Despite the important role of heredity, developmental characteristics and emotional and personal traits of the child, his character and ability to withstand the influence of the outside world are formed within the family. An unfavorable ratio of verbal (speech) and nonverbal (non-speech) communications in the family contributes to the development of anomalies of behavior and character. For example, constant shouting and countless remarks lead to inhibition of the child’s free physiological activity (and this is different for each child and depends on temperament), which can be replaced by a pathological form in the form of tics and obsessions.
At the same time, children from mothers who raise children in an atmosphere of permissiveness remain infantile, which predisposes them to the development of tics.
Tic provocation: psychological stress
If a child with a hereditary predisposition and an unfavorable type of upbringing suddenly encounters a problem that is too much for him (psychotraumatic factor), tics develop. As a rule, the adults around the child do not know what triggered the appearance of tics. That is, for everyone except the child himself, the external situation seems normal. As a rule, he does not talk about his experiences. But at such moments, the child becomes more demanding of loved ones, seeks close contact with them, and requires constant attention. Nonverbal types of communication are activated: gestures and facial expressions. Laryngeal coughing becomes more frequent, which is similar to sounds such as grunting, smacking, sniffling, etc., that occur during thoughtfulness or embarrassment. Laryngeal coughing always increases with anxiety or danger. Movements in the hands arise or intensify - picking through the folds of clothing, twirling hair on a finger. These movements are involuntary and unconscious (a person may sincerely not remember what he just did), intensify with excitement and tension, clearly reflecting the emotional state. Teeth grinding may also occur during sleep, often combined with bedwetting and nightmares.
All these movements, having arisen once, can gradually disappear on their own. But if the child does not find support from others, they become fixed in the form of a pathological habit and then transform into tics.
Parents often say that, for example, after a severe sore throat, their child became nervous, capricious, did not want to play alone, and only then tics appeared. Often the appearance of tics is preceded by acute viral infections or other serious illnesses. In particular, inflammatory eye diseases are often complicated by subsequent tics in the form of blinking; Long-term ENT diseases contribute to the appearance of obsessive coughing, snoring, and grunting.
Thus, for tics to appear, the coincidence of 3 factors is necessary:
Hereditary predisposition
Incorrect upbringing (presence of intra-family conflict; increased demands and control (overprotection); increased adherence to principles, uncompromising parents; formal attitude towards the child (hypoprotection), lack of communication)
Acute stress that triggers tics
The mechanism of development of tics
If a child constantly has internal anxiety, or, as people say, “restless at heart,” stress becomes chronic. Anxiety itself is a necessary protective mechanism that allows you to prepare for it in advance of a dangerous event, speed up reflex activity, increase the speed of reaction and the acuity of the senses, and use all the body’s reserves for survival in extreme conditions. In a child who often experiences stress, the brain is constantly in a state of anxiety and anticipation of danger. The ability to voluntarily suppress (inhibit) unnecessary activity of brain cells is lost. The child's brain does not rest; Even in his sleep he is haunted by terrible images and nightmares. As a result, the body's adaptation systems to stress are gradually depleted. Irritability and aggressiveness appear, and academic performance decreases. And in children who have an initial predisposition to a deficiency in inhibition of pathological reactions in the brain, harmful psychotraumatic factors cause the development of tics.
Tics and behavioral disorders
Children with tics always experience neurotic disorders in the form of low mood, internal anxiety, and a tendency to internal “self-examination.” Characterized by irritability, fatigue, difficulty concentrating, and sleep disturbances, which requires consultation with a qualified psychiatrist.
It should be noted that in some cases, tics are the first symptom of a more severe neurological and mental illness that may develop over time. Therefore, a child with tics should be carefully examined by a neurologist and psychologist.
Diagnosis of tics
The diagnosis is established based on an examination by a neurologist. In this case, video recording at home is useful, because... the child tries to suppress or hide his tics when communicating with the doctor.
A psychological examination of the child is mandatory to identify his emotional and personal characteristics, concomitant disorders of attention, memory, control of impulsive behavior in order to diagnose variants of the course of tics; identifying provoking factors; as well as further psychological and medicinal correction.
In some cases, a neurologist prescribes a number of additional examinations (electroencephalography[2], magnetic resonance imaging[3]), based on a conversation with parents and the clinical picture of the disease, and a consultation with a psychiatrist.
Medical diagnoses
Transient tic disorder is characterized by simple or complex motor tics, short, repetitive, difficult-to-control movements, and mannerisms. The child experiences tics every day for 4 weeks but less than 1 year.
Chronic tic disorder is characterized by rapid, repeated uncontrolled movements or vocalizations (but not both) occurring almost daily for more than 1 year.
Treatment of tics
1. To correct tics, it is recommended to first eliminate provoking factors. Of course, it is necessary to observe a sleep and nutrition schedule, and adequate physical activity.
2. Family psychotherapy is effective in cases where the analysis of intrafamily relationships reveals a chronic traumatic situation. Psychotherapy is useful even with harmonious family relationships, as it allows the child and parents to change the negative attitude towards tics. In addition, parents should remember that a timely kind word, touch, or joint activity (for example, baking cookies or a walk in the park) helps the child cope with accumulated unresolved problems, eliminate anxiety and tension.
3. Psychological correction.
It can be carried out individually - to develop areas of mental activity that are delayed in development (attention, memory, self-control) and reduce internal anxiety while simultaneously working on self-esteem (using games, conversations, drawings and other psychological techniques).
4. Drug treatment for tics should begin when the possibilities of previous methods have already been exhausted. Medications are prescribed by a neurologist depending on the clinical picture and additional examination data.
The prognosis for children who developed tics at the age of 6-8 years is favorable (that is, the tics disappear without a trace).
The early onset of tics (3-6 years) is typical for their long course, up to adolescence, when the tics gradually decrease
If tics appear before age 3, they are usually a symptom of some serious illness (for example, schizophrenia, autism, brain tumor, etc.). In these cases, a thorough examination of the child is required.
VARIETIES OF NERVOUS TICS IN CHILDREN
Each child has his own individuality, and therefore nervous tics that arise for one reason or another are different.
Tic manifestations generally have two types:
- Motor (motor). They are detected by spasms of individual muscles, their groups or movement of limbs and other parts of the body.
- Voice (vocal). They can be recognized in the form of frequently repeated individual sounds, syllables, exclamations, words and even phrases.
Both groups are divided into simple and complex tics. Everything is clear here. A simple form - one short movement or sound, a complex one - several muscle groups are involved, if there are vocal disorders, progress is also observed in them.
MAIN MANIFESTATIONS
Localization of tic movements most often occurs in the facial or neck muscles. Over time, they can spread from top to bottom. The most common examples of simple childhood motor tics are:
- frowning;
- blinking;
- squinting;
- moving the wings of the nose;
- drawing in air through the nose;
- twitching of the corner of the mouth;
- turning or tilting the head;
- shrug;
- flinching;
- twitching of limbs;
- flexion or extension of fingers;
- snapping fingers.
Vocal tics are manifested by coughing, throat sounds, sniffling, spoken syllables or exclamations. This is a meaningless sound that interferes with speech and gives the impression of stuttering or stuttering. If no measures are taken to eliminate them, the situation will only get worse. Tic movements also progress and reach a new level in the form of:
- grimace;
- head tossing;
- touching various parts of the body with hands;
- contractions of the abdominal muscles or diaphragm;
- squats;
- bouncing.
All of the above nervous tics in children are not all manifestations of the disease. They can be individual and atypical. It all depends on the child’s level of development, his character and temperament, sensitivity to environmental stimuli and a number of other reasons.
What is vocalization
Vocalization is the stereotypical repetition of identical sounds that occurs in children before they learn to speak. For a child with autism, this phenomenon can continue throughout life, especially if his speech does not develop.
Vocalizations can be divided into two categories:
- Speech sounds include consonant and vowel sounds (eg baba, daba) and are often referred to as babble.
- Sudden - natural, vegetative sounds that do not resemble speech, such as crying, laughing, commotion, as well as unusual sound productions such as squeals and growls.
Higher frequency and longer persistence of atypical vocalizations have been found to be present in children with ASD and in infants at high risk for developing the syndrome, before speech emerges.
FEATURES OF THE DISEASE
Initially, the child exhibits motor tics, and if the situation worsens, then vocal tics join them. However, there are cases when hyperkinesis begins with sound tics, which significantly complicates diagnosis and delays treatment.
In severe cases, several types of spontaneous movements are observed simultaneously. Sometimes they are accompanied by vocal tics.
Nervous tics in children have their own characteristic features, which make it possible to distinguish them from other pathologies of motor functions. They can be divided into several points:
- Self-control. It should be noted that it works only in the early stages of the disease. This means that the child can control his seizures, but over time it becomes more and more difficult to do so.
- Increased symptoms due to stressful situations. The same tendency is observed at the end of the day due to overwork of the nervous system. The autumn-winter period is the peak of the disease.
- The child's consciousness is not affected in any way. This fact allows us to exclude the development of epilepsy.
- Hyperkinesis does not occur during sleep. This feature is relevant in the presence of vocal tics and confirms the absence of pathologies of the upper respiratory tract.
- A nervous eye tic in a child can at first be mistaken for developing conjunctivitis, but soon everything becomes clear.
The following pattern has been noticed: the earlier the disease appears in a child, the more severe it will be. If appropriate measures are not taken, hyperkinesis develops into a chronic form. In this case, treatment is complicated by the fact that several muscle groups may gradually be involved. Pathological movements move from the head to the lower organs and become more complex, vocal tics are added. Doctors assess them as generalized.
Tic manifestations that arise after the age of ten are almost always classified as transient. This means that they disappear spontaneously and unnoticed, just as they appeared. They are also called transient. They do not require special participation from the medical side.
Some features of the nervous system
Each lobe of the cerebral cortex (CBC) is responsible for certain functions. Neurons that send signals to skeletal muscles and provide movement are located in the precentral gyrus. The latter is located in front of the deep groove separating the frontal and parietal lobes of the CBP. On the other side of the groove is the postcentral gyrus, which is responsible for tactile sensations.
Absolutely all nerve centers of the human BSC interact with each other. Speech function, vision, mental and emotional signals - all this, due to various connections, influences motor acts and muscle tone.
There is a subcortical (extrapyramidal) system - a brain structure that does not belong to the CBP. Thanks to neural connections, they are combined into a single “composition” that performs certain tasks:
- control over muscle tone;
- control over conjugate muscle actions;
- body support;
- presence in motivational and cognitive processes.
Any voluntary movement involves simultaneous tension of some muscles and relaxation of others. Moreover, people don’t even understand what exactly needs to be reduced and relaxed. All this is done automatically due to the work of the extrapyramidal system.
REASONS FOR THE APPEARANCE
Despite countless years of research into nervous tics in children, doctors have not been able to come to a common point of view regarding the provoking factors. But among many theories, it was found that the most likely are the consequences of traumatic influences. These include:
- Fright.
- Fear.
- Divorce of parents or forced separation from one of them.
- Change of environment.
- First of September. The first days of school are extremely stressful for a child.
- The birth of a second child in the family.
Heredity also plays an important role in the occurrence of tics. Children whose parents experienced hyperkinesis in childhood are much more likely to develop it too.
An unstable situation in the family or immediate environment that a child encounters in kindergarten, school, or in the yard is, of course, the main provoking factor. Children's relationships, communication with peers and adults, can be of a very diverse nature. They often contain conflict situations, and they serve as the starting point of nervous disorders.
Organic brain damage can also cause nervous tics in children. Sometimes they are a consequence of the following events:
- severe maternal pregnancy and difficult childbirth;
- traumatic brain injury;
- a previous neuroinfectious disease.
Separately, it should be mentioned that the reasons for the development of tics may be hidden in a lack of any vitamins, minerals or trace elements. Since the child’s body is just being formed and is very unstable to external influences, hypovitaminosis can cause disturbances or malfunctions of the nervous system.
It has been noticed that the disease progresses in waves. If the child is in a calm, balanced mental state, then tic movements may decrease to minimal manifestations or not be observed at all. At the same time, any stressful situation, fear or anxiety, serves as an impetus for exacerbation of the condition and intensification of tics.
Why do they arise?
The main causes of tics are hereditary factors, autoimmune processes, disorders of dopamine metabolism in the brain, organic lesions of the brain, stress, anxiety, family problems, childhood neurosis, anxiety, headaches, fatigue, playing on a smartphone, head or brain injuries , intrauterine hypoxia, heavy workload at school, unfavorable environmental conditions. The hereditary factor is very important, but the predisposition to tics is inherited, not the tics themselves. And the first clinic appears under the influence of provoking factors. For example, constantly sitting at a computer, smartphone, laptop, tablet can provoke the development of tic movements. Or stress, joy, or a change of environment can contribute to the appearance of vocalisms.
DIAGNOSTIC PROCEDURES
Before starting any treatment, you need to have your child examined by a specialist. After the initial examination, the neurologist refers the patient to undergo electroencephalography. It makes it possible to identify the following indicators:
- local cerebral disorders;
- foci of pathological activity;
- analysis of the state of brain activity.
Repeated studies allow you to monitor the effectiveness of the therapy. A biochemical blood test is mandatory. If the doctor deems it necessary, the child may be sent for an MRI.
Identifying nervous tics in young children, establishing their causes and prescribing adequate treatment is the task of a neurologist. But the direct responsibility of parents is to ensure a comfortable stay for the child at home, in an educational institution or on the street. It is necessary to find out the factors that pose a threat to the baby’s psyche and eliminate them in any way.
TREATMENT
Very often, children who are diagnosed with tic hyperkinesis do not need special therapy. It is absolutely meaningless, and only correction of the patient’s lifestyle helps. However, if the tics become generalized, then treatment cannot be avoided. But which method the doctor chooses depends on the severity of the disease, age and physical characteristics of the child.
An integrated approach to treating tics in children is possible. It includes:
- Activities aimed at properly organizing the child’s daily routine. Protecting him from stress, anxiety and other troubles.
- Drug-free therapy. This complex includes a visit to a psychotherapist, physiotherapeutic procedures, and reflexology.
- Treatment with medications.
At the initial stages of the development of tics in young children, only routine measures are sufficient for visible positive dynamics. Rationally organized time for activities and rest, timely going to bed, proper nutrition, and exercise are the key to a positive outcome from a nervous disorder.
Family psychotherapy is of no small importance. If the situation in the family has given impetus to the development of tics, then you need to try to correct it. Under no circumstances should the child witness quarrels or scandals. It is necessary to create a calm, trusting environment so that the child feels loved and protected. You should not pull back or remind him of his nervous disorder, as this will only aggravate the situation.
Good results in the prevention and treatment of tics are provided by educational games using fine motor skills, art therapy, and relaxation. The most commonly used physiotherapeutic methods to combat this disorder are:
- biofeedback method;
- audiovisual stimulation method;
- acupuncture;
- laser therapy;
- ozokerite applications;
- massage of the cervical-collar area;
- electrosleep.
In cases where drug treatment cannot be avoided, sedatives are first prescribed. They have a general calming effect, remove nervousness and irritability. If the expected effect is not observed, the doctor prescribes tranquilizers. Their scope of action is the relief of emotional stress, anxiety and fears.
With progressive tic hyperkinesis, which is not amenable to gentle treatment, more severe drugs are used. These include antipsychotics and antidepressants. Unfortunately, these medications have a lot of side effects and are used only as a last resort, only as prescribed by a doctor and strictly following the dosage. The main indicator for use is the safety of the child, taking into account the special sensitivity of the not yet formed organism, including the nervous system.
Treatment of tics in children is usually carried out on an outpatient basis, since hospitalization can be an additional source of anxiety. For the same reason, drug therapy is avoided by injection.
Diagnosis of pathology
In order to find out what type of hyperkinesis you are dealing with, you need to undergo a comprehensive examination, which includes the following procedures:
- electrocardiogram; — Ultrasound of all main and other large blood vessels, capillaroscopy; — neurological and somatic examination; - electroencephalogram; — examination by a psychologist using various diagnostic techniques; — consultation with a rehabilitation specialist who will determine how ready the vascular system is to adapt to emotional and physical stress.
POSSIBLE CONSEQUENCES
Nervous tics in children of different ages, regardless of the cause, are signals that not everything is all right with the child, his mental state is at the limit of his capabilities, and he needs immediate help. If the irritant is removed in time, the tic manifestations go away spontaneously.
What happens if you leave everything as is? There are several possible scenarios here:
- Epilepsy. Tics may be symptoms of the early stages of this severe neurological disease.
- Severe neuroses, psycho-emotional disorders. Untreated hyperkinesis progresses in the child’s body, causing new manifestations of the tic condition. Lack of qualified help leads to the development of depression and other critical conditions.
- Tourette's syndrome. Although this mental disorder is not a consequence of parental inactivity, its clinical picture necessarily includes both motor and vocal tics.
Even if hyperkinesis disappears on its own after a week without any consequences, it is necessary to go to the doctor and undergo diagnostic procedures. This is a guarantee of the child’s health, and is done with the aim of eliminating the above diseases.
General information
According to numerous surveys, almost 25% of elementary school students have encountered a similar condition. It is curious that nervous tics are observed more often among males than among girls.
Typically, stereotypical movements do not harm children's health and disappear on their own. That's why only twenty percent of children are seen by doctors. And yet, in some situations, tics can negatively affect mental and physical well-being and manifest themselves in adolescence and young adulthood.
An important difference between this condition and seizures in nervous and mental illnesses is that the child is able to reproduce and exercise minimal control over actions. Also, tics do not appear during voluntary movements (in particular, when lifting a mug or swallowing water).
The intensity of the disorder varies depending on the activity, psychological mood, and time of day. The localization of tics may also change (for example, blinking is transformed into chaotic jerking of the shoulders). This does not indicate another disease, but a repetition of an already present one.
Tics can intensify due to children staying in the same position for a long time (watching cartoons, sitting on a bus, at a desk). Involuntary movements weaken or are eliminated during play activities, in the case of an exciting activity (the baby is reading an interesting book). If interest in the action has disappeared, then the tics appear again. Their intensity can be controlled, but then rest is needed.
Tics were first described in literature as “the habit of muscles to contract” back in the middle of the 7th century.
ADAPTATION IN SOCIETY
Children, as we know, are cruel by nature, so it will be very problematic for a child with obvious manifestations of hyperkinesis to adapt to a new team. But it’s not his fault that the nervous tic happened to him. When communicating with adults, it is very important for him to feel a tolerant attitude. And if at home they constantly focus attention on this topic and reprimand the child, believing that he is doing this on purpose, the situation only gets worse.
Parents should be completely on the side of the child, and he should feel this not only in words. This is what it should look like:
- all conversations about nervous disorders, including tics, should be prohibited, especially in the presence of a baby.
- do not focus on the problem, behave freely and naturally.
- conduct an explanatory conversation with teachers or educators of the team that the child attends, and call on them for assistance.
- choose a suitable leisure activity for your child. Single active sports, such as skiing or swimming, are encouraged.
- provide nutritious and varied nutrition.
During adolescence, a teenager’s body is unpredictable, and also undergoes hormonal changes. If at this stage nervous tics are also detected, then this can generally turn into a personal tragedy. First of all, self-esteem suffers; the child withdraws into himself, does not want to communicate with anyone, and is fixated only on his illness.
The parents’ task is to consider the threat in time and take all measures to eliminate it. Even if the tics do not go away on their own, there is every chance that properly selected therapy or medication will help get rid of them. In any case, you can and should strive to live a full life.
PREVENTION TIPS
To prevent a child’s nervous tics from developing into more serious mental disorders over time, all possible measures must be taken to prevent them. You don't need anything supernatural to do this. It will be enough not to forget that the baby sees the behavior of the parents and people around him, draws his own conclusions and evaluates the events taking place due to his level of development.
The psyche of a child at an early age is unstable and vulnerable, so any clarification of the relationship between parents in a raised voice is a stressful situation that can lead to tic manifestations. It is in the family that the child should feel support and understanding. This is his fortress, in which, if necessary, he can hide from all his fears. If there is no such relationship, then the risk of developing tics is quite high.
Children living in a calm, friendly environment are very rarely susceptible to nervous tics. To avoid having to treat the consequences of mental imbalance in a child, it is enough to create comfortable conditions for him. They are as follows:
- avoidance of anxiety and stressful situations;
- healthy, full sleep;
- high-quality and healthy food, a ban on fast food and overly sweet and fried foods;
- compliance with the daily routine, proper organization of rest;
- dosed computer use and TV viewing;
- maximum exposure to fresh air;
- classes in sports sections that match the interests and temperament of the child;
- inadmissibility of overwork.
In rare cases, raising the younger generation does not involve punishment. They are certainly necessary, but within reason. Physical impact is immediately excluded. Only moral methods of influence are acceptable. The child must clearly know what offense he is being punished for and how he should have done the right thing. At the same time, you should assure the child that punishment does not affect his love for him. Only in such a situation will he draw the right conclusions and receive minimal nervous shock.
Even if the appearance of nervous tics in a child could not be avoided, it should be remembered that this is not the worst thing that could happen to him. Modern medicine, combined with parental care and attention, can work wonders.