Trigeminal neuritis is sometimes mistakenly called trigeminal neuritis of the facial nerve, but more often another term is used - “neuralgia” - which literally means pain. This is an inflammatory process in the fifth pair of cranial nerves.
Our expert in this field:
Lashch Natalia Yurievna
Neurologist of the highest category, candidate of medical sciences, associate professor. Laureate of the Moscow City Prize in the field of medicine.
Call the doctor Reviews about the doctor
Some facts about the disease:
- On average, it occurs in 6-8 people out of every 100,000.
- Women get sick more often than men.
- In most cases, the disease is diagnosed in people over 40-50 years of age.
There are two types of trigeminal neuralgia:
- Primary occurs as an independent disease.
- Secondary – a symptom of other pathologies.
How does the trigeminal nerve work?
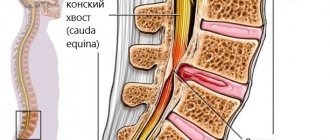
The trigeminal nerve is the fifth pair of cranial nerves (there are 12 pairs in total - they innervate the organs of the head and neck). It is paired - that is, it is on the right and left. It consists of two types of nerve fibers - sensory and motor. After exiting the skull, the trigeminal nerve divides into three branches, which seem to cover the entire face:
- Ocular - is sensitive, innervates the eyeballs, eyelids, lacrimal sacs, mucous membrane of the nose and its paranasal sinuses, lacrimal gland, forehead skin.
- Maxillary - also sensitive, innervates the skin of the cheek, temple, teeth and gums of the upper jaw, mucous membrane of the palate, nose.
- Mandibular - responsible for both sensitivity and movement, innervates the muscles of mastication, muscles of the palate, eardrum, mucous membrane of the cheek, anterior 2/3 of the tongue, skin of the temple, the front of the ear and external auditory canal, teeth and gums of the lower jaw.
Therapeutic measures in case of damage to the trigeminal nerve branch
| Event | Doctor's actions |
| Any nerve injury event | Suspected or known damage to a nerve and/or branch of a nerve requires IMMEDIATE treatment for repair and recovery. |
| Implantation | If <24-48 hours after surgery and numbness or neuropathy persists after local anesthesia has worn off, consider implant removal. N. _ B. _ On the same day, DO NOT reimplant, move the implant coronally, or replace the implant with a shorter one. |
| Endodontic treatment | If <24-48 after the onset of neuropathy, consider: - or surgical extraction of the tooth and removal of the exposed endodontic material or instrument; - or save the tooth, perform root canal filling (IDC) and long-term irrigation with saline solution. |
| Wisdom teeth surgery – injury to the inferior alveolar nerve | If <2 weeks, surgery may be indicated if radiographic evidence of tooth root fragments (incomplete extraction) or IDC damage is indicated. |
| Wisdom teeth surgery - lingual nerve injury | If >3-6 months consider cognitive behavioral therapy or surgery. |
| Anesthesia-related nerve damage (compression and ischemia of the LN or IAN) | Only therapeutic conservative treatment. |
| Nerve damage associated with orthognathic surgery | Only therapeutic conservative treatment. |
| Nerve damage associated with mandibular fracture | Only therapeutic conservative treatment. |
Many patients with sensory nerve injury present with a combination of symptoms of pain, anesthesia, hypoesthesia, hyperesthesia, and neuropathic symptoms such as pins and needles, and other paresthesias. Although these are different sensations, patients usually experience a mixture of symptoms in different parts of the neuropathic area. For example, a patient with inferior alveolar nerve injury (IANI) may experience burning pain in the chin along with lip numbness.
Rice. 3. The diagram shows the intersection of different manifestations of nerve damage. Although pain and anesthesia or hypoesthesia are diametrically different sensations, patients with nerve damage always experience combined symptoms in different parts of the neuropathic region. There are always patients who will experience a mixture of all symptoms and these are usually the hardest patients to treat.
Important! In patients with neuropathy, neurosensory testing should be performed every 2-3 weeks to assess nerve recovery, which will be reflected in a decrease in the intensity of symptoms and a decrease in the area of dermotome and mucosa involvement. Neurosensory improvement most often occurs after two to three months.
If sensitivity has not improved significantly three to four months after surgery, the prognosis is usually poor. Zuniga JR, Yates DM. Factors Determining Outcome After Trigeminal Nerve Surgery for Neuropathic Pain. J Oral Maxillofac Surg 2016 Jul;74(7):1323-9.
Nerve damage is defined as permanent if treatment is not initiated within 48 hours of injury and/or symptoms do not improve >1 month after implantation or endodontic treatment and >6 months after extraction of third molars or for other reasons.
If there is a persistent large neuropathic area (>40% of the dermatome), then severe nerve damage can be considered, and the development of pain and/or hypersensitivity are major factors that impair daily functions such as articulation, eating and drinking, shaving or applying makeup, and cleaning teeth, sleep, etc. and are often the main reasons for a patient to seek treatment.
It is the prevention of damage to the branches of the trigeminal nerve that is the main task of the clinician, since no treatment tactics guarantee complete restoration of the damaged nerve fiber and its functions.
The main recommendation for the doctor is early recognition of the injury to the sensory nerve branch, honestly informing the patient about realistic expectations for his recovery.
Treatment of trigeminal neuritis
Typically, treatment of the disease begins with medications:
- Anticonvulsants . Usually the drug carbamazepine or phenytoin, oxcarbazepine is prescribed; the doctor selects the dose individually. Over time, these medications may become less effective, in which case your doctor will increase the dosage. However, anticonvulsants have some side effects that may make it difficult to use them.
- Antispasmodics . Used together with anticonvulsants. For example, a neurologist may prescribe baclofen for you.
- Physiotherapy . Diadynamic currents, ionogalvanization with novocaine, and ultraphonophoresis with hydrocortisone help to cope with the symptoms of trigeminal neuritis.
If neuralgia manifests itself in the form of severe toothaches, painkillers are used, and ointments with anesthetics are rubbed into the gums.
If medications no longer help, the neurologist raises the question of surgical treatment of trigeminal neuritis. The following operations are possible:
- Microsurgical decompression . During the intervention, compression of nerve fibers by blood vessels is eliminated. Typically the incision is made behind the ear. The operation effectively eliminates pain, but after it a relapse may occur, complications such as hearing loss, numbness of the face, paresis and paralysis of the facial muscles.
- Transection of nerve branches . In this case, the transmission of pain impulses is disrupted.
- Radiosurgery (gamma knife). A special device generates a high dose of ionizing radiation, which damages nerve fibers. If painful attacks begin to bother you again in the future, the procedure can be repeated.
There are other surgical methods for treating this type of neuritis.
We will call you back
Message sent!
expect a call, we will contact you shortly
The trigeminal nerve provides sensation to the skin of almost the entire face and front of the head. It is mixed in structure, that is, it is responsible for both sensitivity and movement, but the motor fibers are thinner. Still, the trigeminal nerve is mostly sensitive. This determines the characteristics of the symptoms of the disease.
How to properly treat a chilled tooth nerve?
If the dental nerve is cold, you should not postpone a visit to the dentist, as the inflammatory process and pain will intensify over time, which will lead to dangerous negative consequences.
For temporary pain relief:
- Moisten a piece of sterile cotton wool with alcohol (another option is vodka) and apply it to the tooth. This will slightly suppress the inflammatory process and relieve pain. But it is important to avoid contact of the mucous membrane with the cotton wool to avoid burns.
- Add chlorhexidine (no more than 5 drops) to a glass of warm water from a kettle. The solution should be used to rinse the mouth to “pacify” inflammation.
- Use dried sage leaves in small quantities. Pour boiling water over them, let cool. After this, you can rinse your mouth with the resulting infusion.
Professional treatment
The treatment method for a cold dental nerve depends on the cause, the nature of the symptoms, the general well-being of the patient, the condition of the tooth, its pulp and oral mucosa. In case of severe complications, there is usually a need for urgent hospitalization of the patient.
If for now the symptoms are limited to acute pain, the dentist will provide emergency treatment to eliminate the inflammatory process.
If there are chips, other signs of mechanical damage to the tooth, or signs of caries, the diseased tooth is cleaned and filled.
In case of necrosis of the soft tissue of the pulp or its complete damage, surgical treatment and antibacterial therapy will be required after removal of the pulp.
What are the symptoms of trigeminal neuritis?
I am bothered by excruciating attacks of shooting, stabbing pains. They usually last for a few seconds or minutes and then suddenly go away. Most often, pain occurs in the area of innervation of the two lower branches of the trigeminal nerve: in the jaws, cheeks, teeth, gums, lips. In the area of innervation of the upper first branch of the nerve (forehead, eyes), pain occurs less frequently.
Usually only the right or left half of the face is affected. During an attack, a grimace of pain appears on the face, the person freezes, is afraid to move, and holds his breath. Sometimes the patient, on the contrary, begins to breathe heavily and frequently and rubs the sore spot.
Over time, attacks become more frequent and severe. There are certain “trigger zones” - most often they are on the lips and gums. Touching them, exposure to high or low temperature (cold or hot food) provoke painful attacks.
Often, pain due to neuritis is accompanied by vegetative symptoms, such as redness of the facial skin, lacrimation, and the release of large amounts of saliva.
Are you experiencing similar symptoms? Perhaps this is trigeminal neuritis or another disease, for example, arthrosis of the temporomandibular joint, multiple sclerosis. Only an experienced neurologist will be able to establish the correct diagnosis and prescribe effective treatment.
How to protect the dental nerve from hypothermia?
- During the cold season, use warm hats, scarves and outerwear with a high collar.
- In low temperatures and strong winds, it is advisable to cover your face with clothing.
- Do not use a thermos with hot water. Temperature changes may cause inflammation of the dental nerve and the appearance of an acute painful reaction.
Study the condition and appearance of your teeth, as well as the oral mucosa, regularly on your own. This way you can see suspicious changes in a timely manner.
Long term forecast
With treatment (and in rarer cases, without it), remission - the symptoms of trigeminal neuritis do not bother you for several months or even years. Many patients are helped by medications, but over time they begin to act weaker, and they have to resort to surgical treatments.
Frequent and severe pain attacks can reduce performance and quality of life. In young patients, the prognosis is more favorable, in older people (and it is in them that the disease occurs more often) it is more serious.
Take care of yourself, book a consultation now
Message sent!
expect a call, we will contact you shortly
The cause of trigeminal neuritis is not always found. In this case, the disease is called idiopathic . If the damage to the nerve trunks is caused by some other disease, they speak of symptomatic , or secondary , neuritis.
Most often, the disease develops as a result of compression of the nerve by improperly located vessels. In most cases, the superior cerebellar artery is to blame.
Modern medicine sees the mechanism for the development of inflammation and pain as follows. Chronic compression causes the trigeminal nerve to lose myelin , a sheath that is made of fat and is important in conducting nerve impulses. An inflammatory process develops. Subsequently, degeneration of axons - the long processes of nerve cells that make up the nerve fiber.
Symptoms of dental nerve inflammation
What are the most common symptoms if the nerve has a cold:
- possible hypersensitivity of the eyes, eyelids and forehead;
- the occurrence of constant aching pain in the jaw area;
- the appearance of shooting pain;
- constant severe pain, which worsens when teeth come into contact with cold or hot food;
- it hurts to smile.
The inflammatory process during hypothermia of the dental nerve occurs from the penetration of pathogenic microflora into the pulp, which is the cause of shooting pains when there is a large temperature difference or during physical contact (pain when chewing).
If pathogenic processes develop very quickly or the patient delays visiting the dental clinic, then inflammation can spread beyond the damaged tooth in the form of swelling, which everyone is accustomed to calling “flux.” Its medical name is periostitis. The second possible complication is periodontal inflammation. Unlike flux, it does not have an external expression in the form of noticeable swelling and is not accompanied by purulent formations.
This cold, in which the dental nerve hurts, occurs equally in men and women. Therefore, when the question arises: “What to do if your tooth gets a cold?” or “Is it possible to catch a cold on the facial nerve?”, consult a doctor immediately so as not to get even more unpleasant complications.
If you do not do this as soon as possible, the inflammatory process will develop, and this can lead to the appearance of multiple purulent foci, and subsequently to the death of first the tissue, and then the dental nerves. Over time, severe pain stops, but inflammation continues, and the longer you postpone a visit to the hospital, the more difficult the treatment will be.
Reasons for the onset of the disease
If you regularly visit the dentist and pay enough attention to dental care, then most likely you are not in danger of developing inflammation of the dental nerve. But if you neglect the condition of your teeth, such a disease is not uncommon. There are several reasons that can trigger nerve inflammation:
- neglected and not cured in time caries, especially when the remote control is damaged;
- There are chips, injuries, and fractures on the teeth;
- with a previously acquired infection due to improper treatment;
- during previous treatment, low-quality materials or medications were used;
- When installing the prosthesis, the tooth was processed incorrectly;
- Perhaps the body, at this time, was weakened by another infectious disease.
Treatment at home
What to do if your nerve has already caught a cold, but you won’t be able to visit a doctor in the near future for some reason. Is it possible to treat a tooth without the help of a dentist, and most importantly, how to treat it?
The first step is to carry out antibacterial therapy, which will prevent the development of the inflammatory process. Next, you need to deal with pain relief if professional help is not available.
The main rule that must be observed when treating any foci of inflammation is that you cannot apply warm compresses and in general do not warm the site of inflammation. The most you can do is cover your cheek with a scarf.
The following drugs can be used for pain relief: coffedon, dexalgin, oxadol, lidocaine .
ethnoscience
There are many traditional ways to treat a tooth without expensive medications. All of them belong to the so-called alternative medicine, which uses herbs, fruits or other very accessible and inexpensive remedies.
- you can try rinsing with strong alcoholic drinks, preferably regular vodka, at room temperature;
- you can apply a compress of chopped onion wrapped in a thin cloth to the ear on the opposite side of the diseased tooth;
- very good results were shown by rinsing with a lukewarm soda solution or sage infusion (15 mg of sage per 200 mg of hot water, leave for 15 minutes, strain before use);
- crush a regular analgin tablet and apply it to the painful area, this relieves acute pain well;
- Salted lard was considered an excellent remedy for toothache. Apply a small slice of lard to the sore spot;
- many traditional healers advise using a cut clove of garlic, like lard, and applying it to the affected tooth;
- make a small cotton ball, soak it in alcohol and apply it to the sore spot, trying not to touch the gum, as long-term exposure to alcohol can cause a burn;
- dilute a few drops of Chlorhexidine in a glass of warm water and rinse your mouth with this solution at least three times a day;
- Another remedy is to chew a sorrel leaf;
- pour birch buds (25 g) with alcohol (100 g), leave for 10 days. Moisten a cotton ball with this tincture and place it on the sore tooth;
- cloves have long been considered an excellent remedy for toothache, so simply moisten a cotton ball with clove oil and apply it to the gum, and if there is an open cavity in the tooth, then put the cotton wool directly into it;
- Hydrogen peroxide has long become a popular component of many folk recipes, and in this case, rinsing with a solution of peroxide and water can effectively disinfect the oral cavity, stop inflammation and, as a bonus, remove plaque from teeth.
All these folk recipes will help relieve an attack of acute pain only for a short time, but will not solve the problem itself. Only a professional doctor will help you cure inflammation.
What other causes can lead to trigeminal neuritis?
In addition to vascular compression, other causes can lead to the disease:
- Age-related changes in the body.
- Compression of the nerve branches in the bone canals of the skull in which they pass. These canals can be narrowed from birth, or as a result of certain diseases: caries, sinusitis.
- Compression by intracranial tumors.
- Injuries to the face, head.
- Multiple sclerosis. This is a chronic disease in which the myelin sheath is destroyed. Trigeminal neuritis affects 3-4% of patients with multiple sclerosis.
- Postherpetic neuralgia. Its cause is herpes zoster.
Types and causes of trigeminal neuralgia
- Primary (idiopathic) - occurs in the absence of other diseases or pathological processes due to compression of the trigeminal nerve root.
- Secondary (symptomatic) - is a consequence of other pathologies.
The factors that most often provoke the development of the disease include:
- infringement of the trigeminal nerve (temporomandibular joint injuries, congenital anomalies in the development of bone structures of the skull, tumors of the brain and facial area, pathological vasodilatation, etc.);
- viral nerve damage (herpetic infection, polio);
- odontogenic infections (“unsuccessful” filling or extraction of teeth or other surgical interventions in the face and oral cavity, reaction to anesthesia of dental canals, dental flux).
Causes of pain attacks in trigeminal neuritis. What are triggers?
Triggers are irritants, “triggers” that provoke an attack of pain. These can be a variety of mechanical or temperature effects on the skin of the face and mucous membranes.
Most often, the following factors act as triggers: shaving, eating food (especially cold or hot), any touching the face, drinking, talking, brushing teeth, wind, applying makeup, washing, smiling. When habitual daily actions always lead to excruciating pain, this significantly reduces the quality of life and interferes with work.
When you see your doctor, tell your doctor what triggers lead to attacks in your case.
How does the treatment of neuritis depend on the causes?
If the cause of trigeminal neuritis is not known, all that remains is to deal with its main manifestation – pain. The neurologist prescribes various medications, and if they stop helping, he recommends surgery.
If the cause of the disease is known, you need to try to eliminate it. For example, if a patient is diagnosed with multiple sclerosis, special therapy is prescribed that helps slow down the progression of the pathology. If the nerve is compressed by an artery or the walls of a bone canal, the compression must be removed.
Get a consultation with a doctor
Message sent!
expect a call, we will contact you shortly
Sometimes, before the correct diagnosis is finally established, a patient suffering from trigeminal neuritis has to see more than one doctor. It is extremely important to start treating the disease as early as possible. It has been proven that the longer a person suffers from trigeminal neuralgia, the more difficult it is to cope with the pathology.
Diagnosis of trigeminal neuritis: what happens during an appointment with a neurologist?
An appointment with a doctor begins with a conversation. First of all, it is important for a neurologist to get answers to three questions:
What is the nature of the pain? Is it typical for this disease ? With trigeminal neuritis, pain attacks occur suddenly, they are strong, painful and pass quickly.
Where does the pain occur ? When the trigeminal nerve is damaged, pain is localized on the face, in certain places.
What triggers lead to seizures ? Usually this is touching the face, exposure to wind, high and low temperatures.
You will be asked how long you have been experiencing symptoms, whether you suffer from any chronic diseases, and whether you are receiving any treatment. Then the neurologist will examine you and press on certain points on your face where the branches of the trigeminal nerve enter the skin. A general neurological examination will be performed to diagnose any possible medical conditions that may be causing your symptoms.
Management of patients with post-traumatic sensory neuropathy
Consultation with a patient with post-traumatic sensory neuropathy usually requires a minimum of 30–40 minutes of time.
- It is necessary to carefully and in detail collect a medical history, including: - date and origin of nerve damage; — patient’s self-assessment of neurosensory function in terms of changes in sensitivity: hyperesthesia, hypoesthesia, anesthesia; — patient self-assessment of neurogenic discomfort and regular pain: paresthesia, dysesthesia, allodynia, dysgeusia, ageusia (loss of taste); — psychological screening; — functional screening (impact on daily life).
- It is necessary to conduct a series of standardized tests of neurosensory functions, using mapping to assess the size of the neuropathic area, determine the nature of functional problems and assess the level of pain. Pain is assessed using a visual analogue scale, where 0 is no pain and 10 is the worst possible pain.
- Assess the percentage of the neuropathic area of the extraoral and intraoral dermatomes, where 100% of the extraoral dermatome - the entire extraoral area of the skin innervated by the inferior alveolar nerve on the damaged side is involved in changes, 100% of the intraoral dermotome - the entire mucosa in the area of innervation of the lingual nerve on the damaged side is affected.
- Inform the patient about the diagnosis, extent of injury, probable cause, and persistence of injury.
- Discuss possible symptomatic and etiological treatment strategies and expectations regarding such treatment. Inform the patient how his symptoms are explained by current understanding of neurobiology (eg, cold allodynia).
- The patient must be given the opportunity to communicate by telephone with the doctor.
It is important to differentiate post-traumatic neuropathy from trigeminal neuropathy associated with malignancy, multiple sclerosis, sickle cell disease, neurological disease, alcoholism, trauma, diabetes, HIV, postherpetic neuralgia, stroke, or chemotherapy.
Management options for patients with post-traumatic neuropathy will depend on understanding of the mechanisms and duration of injury, the symptoms identified, and the wishes of the patients.
Patient management strategies include:
- Comfort and observation.
- Early medical treatment (steroid hormones, vitamin B complex, and NSAIDs-nonsteroidal anti-inflammatory drugs) is aimed at minimizing the development of the inflammatory response to nerve damage and promoting its recovery. When local pain is present, there is evidence for the use of topical lidocaine 5% patch and local clonazepam injections. Botulinum toxin type A (Botox) injections for focal neuropathic pain have limited success.
- Psychiatric and psychological support in the form of cognitive behavioral therapy and based on the results of psychometric questionnaires, including the PainDETECT . It is important to reassure patients with permanent nerve damage that their condition will neither worsen nor improve, and that the condition does not predispose them to the development of any other pathology in the area. It is also very important to explain to the patient the pathological physiology of nerve fiber damage and honestly tell how difficult this condition is to treat.
- In cases of chronic pain, systemic administration of pregabalin, oxcarbazepine, venlafaxine or nortriptyline.
- Early or delayed surgical treatment, decompression or direct anastomosis.
- In cases of trigeminal neuropathic pain, alternative pain treatment strategies such as transcutaneous electrical nerve stimulation (TENS), acupuncture, low-level laser therapy, and myogymnastics may be effective.
- Speech therapy assistance.
- Observation and assessment of the dynamics of the condition according to the following results: reduction of pain, improvement of functionality and the patient’s ability to cope with iatrogenic post-traumatic neuropathy.
Typically, patients need a comprehensive approach to treating neuropathy, based on the pain, functional and psychological problems the patient is experiencing. Juodzbalys G, Wang HL, Sabalys G. Injury of the Inferior Alveolar Nerve during Implant Placement: a Literature Review. J Oral Maxillofac Res 2011 Apr 1;2(1):e1.
What diagnostic methods can a doctor prescribe for trigeminal neuritis?
The disease can be caused by various reasons, sometimes very serious (for example, cancer). Diagnosing them is not always easy. Depending on your complaints and information obtained during the examination, the neurologist may prescribe various instrumental studies and laboratory tests.
Magnetic resonance imaging of the head is most often used. This diagnostic method helps to identify pathological changes in the brain characteristic of multiple sclerosis and intracranial tumors.
The doctors of the medical center International Clinic Medica24 adhere to modern current standards - this guarantees that you will be prescribed all the tests necessary in your case, the doctor will not miss anything. At the same time, the coordinating doctor in our clinic will make sure that only truly necessary procedures are prescribed to you, so that you do not overpay for unnecessary things. All types of diagnostics are carried out using our medical center’s own equipment.
The material was prepared by Natalya Yurievna, a neurologist at the international clinic Medica24, Candidate of Medical Sciences Lasch.