Clinical picture of osteomyelitis of the tooth socket
The clinical picture of osteomyelitis of the tooth socket is characterized by complaints of acute throbbing pain both in the area of the socket and in the area of neighboring teeth. General symptoms such as weakness, hyperthermia, headache, chills, impaired performance and sleep are also observed. Swelling of the perimandibular soft tissues develops, the submandibular lymph nodes are enlarged, dense, painful on palpation.
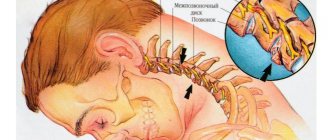
With osteomyelitis of the socket of only one molar of the lower jaw, the inflammatory process can spread to the area of the masseter or medial pterygoid muscle, which, in turn, can cause difficulty opening the mouth. When examining the oral cavity, the doctor may detect a dirty gray coating on the bottom and walls of the socket. You can also smell a specific smell. Percussion of adjacent teeth is painful.
The mucous membrane in the area of the transitional fold is hyperemic and swollen. Palpation of the alveolar process from the buccal and oral sides is sharply painful both in the area of the socket and adjacent teeth.
The acute phase of inflammation lasts about 6–8 days, sometimes 10 days. Then the inflammatory phenomena decrease, the process becomes chronic. The general condition improves, body temperature decreases. Swelling and hyperemia of the mucous membranes also decrease, and then pain on palpation of the alveolar process, swelling of facial tissues and submandibular lymphadenitis disappear. After 12–15 days, the tooth socket is filled with loose, pathological granulation tissue, sometimes bulges out of the socket, and pus can be released when pressure is applied.
On the x-ray we see fuzzy blurred contours of the compact lamina of the alveoli; osteoporosis and bone destruction in the alveolar region are pronounced. In rare cases, after 20–25 days from the beginning of the acute period, it is possible to identify small sequesters.
Causes of limited osteomyelitis of the socket
1. as a complication of alveolitis. 2. as a result of decreased immunity
Treatment of socket osteomyelitis
In the acute stage of the disease, therapy begins with revision of the hole. Under conduction or infiltration anesthesia, the tooth socket is cleaned of remnants of a blood clot, food and pathological tissue. Then the well is washed from a syringe with a weak antiseptic solution or a biologically active drug. The following drugs are used: staphylococcal and streptococcal bacteriophage, proteolytic enzymes, lysozyme. After this, a bandage with Alvogyl is applied to the wound.
To reduce inflammation and pain, dissection of the infiltrated area of the mucous membrane and periosteum is performed. An incision is made along the transitional fold 1.5–2 cm long, as well as an incision on the inside of the alveolar process. Drug therapy is prescribed: antibiotics, sulfa and antihistamines, analgesics, physical therapy (UHF, ultrasound, helium-neon laser). To increase specific immunological reactivity, phagocytosis stimulants are prescribed: pentoxyl, methyluracil, milife, lemongrass.
After relief of acute inflammation, treatment with multivitamins and stimulants of nonspecific resistance of the body is continued (methyluracil 0.5 g or pentoxyl 0.2 g 3-4 times a day, sodium nucleinate 0.2 g 3 times a day, milife 0.2 G). Concomitant ultrasound or laser therapy of the inflammation focus is necessary. Approximately 20 days from the onset of the acute inflammatory process, if the wound has not healed and sequesters are found on the radiograph, pathological granulations and small sequesters are removed with a surgical spoon, the walls and bottom of the hole are scraped out. The wound is washed with an antiseptic solution, dried and loosely packed with gauze soaked in iodoform liquid.
Dressings (treating the hole with an antiseptic solution and changing the iodoform gauze in it) are done every 2-3 days until young granulation tissue forms on the walls and bottom of the hole.
Prevention of socket osteomyelitis is the same as for alveolitis.
- Before the intervention, professional oral hygiene is necessary
- the doctor must inspect the socket and perform hemostasis by compression
- if more than two teeth are removed, apply sutures
- After tooth extraction, it is necessary to give clear recommendations to the patient
If, nevertheless, the appearance of alveolitis could not be avoided, and the patient complained of pain, it is necessary to stop the process as quickly as possible. Therefore, the patient must be informed about possible complications and motivated not to delay visiting the dentist if he experiences pain.
Post-traumatic sensory nerve damage. Terminology.
The Association for the Study of Pain has standardized a nomenclature system that defines the most commonly used neurosensory descriptive terms Classification of Chronic Pain, Second Edition: International Association for the Study of Pain Task Force on Taxonomy, ed.: H Merskey and N. Bogduk. IASP Press IASP Council in Kyoto, November 29-30-2007.
- Paresthesia is a non-painful altered sensation. May be described by patients as a pins and needles, slight burning or tingling sensation. NEW sensations - stretching, pulling sensations.
- Dysesthesia is perverted sensations. Abnormal, sometimes unpleasant sensations experienced by a person with partial damage to sensory nerve fibers when touching the skin. - Unpleasant abnormal sensation, spontaneous or provoked. Note : Dysesthesia is not pain when it hurts or paresthesia. Special cases of dysesthesia are hyperalgesia and allodynia. Dysesthesia should always be unpleasant , and paresthesia should not be unpleasant, although it is recognized that the boundary can create some difficulties when it comes to whether these sensations are pleasant or unpleasant. It should always be stated whether the sensations are spontaneous or provoked.
- Neuropathic pain (IASP) is pain caused by damage or disease of the somatosensory nervous system.
- Neuropathy (IASP) is a dysfunction or pathological change in a nerve: in one nerve - mononeuropathy; in several nerves - mononeuropathic multiplex; if diffuse and bilateral - polyneuropathy. Note : Neuritis is a special case of neuropathy and is currently a term reserved for inflammatory processes affecting the nerves. - sensitive (touch, heat, pain) - motor (movement).
- Allodynia is pain from non-noxious stimuli (pain with light touch/cold/heat). The appearance of pain in response to a stimulus that does not cause pain in healthy people. Thermal allodynia, especially cold allodynia, is a feature of the extraoral dermatome in patients with IANIs. Some patients report decreased taste and heat sensitivity. Perversion of sensitivity is characterized by an increased threshold of sensitivity and increased duration of perception, lack of precise localization of sensations of an unpleasant nature, and a tendency to irradiate. The pain continues when the stimulus is removed.
- Hyperalgesia - increased sensitivity to painful stimuli
- Anesthesia - numbness
- Hyperesthesia and Hypostesthesia are terms that are often used to describe changes in sensitivity that increase or decrease, respectively.
Rice. 5 Anatomy of the II (maxillary) and III (mandibular) branches of the trigeminal nerve. It is important to note that the branches of the superior alveolar nerve retrogradely “merge” into the infraorbital nerve, which explains the symptoms of swelling and pain in the infraorbital region when the superior dental plexus is damaged.
Post-traumatic sensory neuropathy is pain that develops after medical intervention (surgery, treatment, anesthesia), with a minimum duration of 2 months, while other causes of pain are excluded (infection, persistent malignancy, misdiagnosis, etc.), preoperative pain from others must also be excluded reasons.
It is important to add that the neuropathic area does not have to be clearly indicated by the patient, however, about 80% of patients can localize and indicate the neuropathic area.
HERE you can read more about the incidence of “phantom toothache” (atypical odontalgia) after endodontic treatment, which is classified as persistent dentoalveolar pain (PDAP type 2) and occurs in up to 3% of cases.
Trigeminal neuritis
Today, traumatic neuritis of the trigeminal nerve is considered one of the most common causes of pain syndromes in the maxillofacial area.
As a complication, it occurs during the removal of permanent molars of the lower jaw, due to damage to the lower alveolar nerve in the mandibular canal. The apices of the roots of the lower molars are in close proximity to the mandibular canal and in some cases may be located in the canal itself. Sometimes, due to chronic apical periodontitis, the bone between the root apex and the wall of the mandibular canal is resorbed. When a tooth is loosened by an elevator, the lower alveolar nerve can be injured, which will lead to partial or complete disruption of the functions of the third branch of the trigeminal nerve. The result is pain in the jaw, numbness of the lower lip and chin, decreased or absent sensitivity of the gums, decreased electrical excitability of the dental pulp on the affected side. Usually all these phenomena gradually disappear after a few weeks.
Electroodontometry
Electroodontometry is the most effective method for assessing the functional state of the trigeminal nerve when it is damaged. EDI is based on a study of the reaction of the teeth of the lower jaw to electrical stimulation. The method is performed on all teeth of the lower jaw, with preserved pulp both in the affected area and on the opposite healthy side.
S.N. scale Fedotova (1997) to assess the severity of damage to the inferior alveolar nerve based on electrical odontometry data:
- mild degree - reaction of teeth with preserved pulp on the side of nerve damage within 20-40 μA;
- moderate severity – reaction of teeth to currents from 40 to 100 µA;
- severe degree - complete loss of pain sensitivity, reaction of teeth to currents above 100 μA
The use of EDI to diagnose traumatic injuries of the inferior alveolar nerve is impossible if:
- lower jaw teeth endodontically treated
- lower jaw teeth are covered with orthopedic structures
- metal elements of splinting structures are fixed on the teeth
- missing teeth
Locations for measuring electrical excitability of facial skin
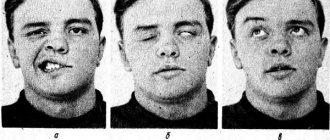
Assessment of the area of paresthesia in traumatic neuritis of the inferior alveolar nerve
The zone of paresthesia is identified - impaired sensitivity of the skin based on a tactile test, photographed, followed by an assessment of the area of the paresthesia zone: points are drawn on the border of areas of normal sensitivity of the skin, the red border of the lips and the paresthesia zone, which are then connected by a continuous line. Zones of hyper-, hypo- and anesthesia were marked with different colors.
I - vertical lines:
- midline,
- a line passing through the outer edge of the philtrum,
- a line passing through the outer edge of the wing of the nose,
- pupil line;
II - horizontal lines:
- lip line,
- a line running along the lower edge of the red border of the lips,
- the border line between the chin and lower lip,
- a line drawn along the most protruding part of the chin,
- line of the border of the chin and submental areas.
Schematic representation of the areas for measuring facial skin paresthesia.
Each of the 12 resulting squares was assigned a score depending on the nature of the sensitivity disorder:
0-sensitivity is not impaired;
1-skin hyperesthesia
2-hypoesthesia of the skin;
3-anesthesia of the skin.
Next, the sum of points was calculated and divided by 12 (quadrants).
With the results:
3.0-2.1 – severe sensitivity impairment was diagnosed;
2.0–1.1 – moderate severity;
less than 1.0 – mild severity of the pathology being studied
Trigeminal facial pain: systematics of clinical forms, principles of diagnosis and treatment
Facial pain, which includes pain on the surface of the face and/or in the mouth (orofacial pain), is one of the most common types of pain. Most often, orofacial pain manifests itself as acute dental pain, which usually regresses after dental treatment. However, in a number of cases, facial pain itself (prosopalgia) is noted, manifested by chronic or recurrent pain, often resistant to various methods of conservative treatment. A kind of primacy in severity belongs to trigeminal facial pain, especially trigeminal neuralgia and deafferentation trigeminal neuropathy, during exacerbation of which the severity of pain is many times greater than the intensity of acute toothache familiar to most people.
Taxonomy of trigeminal prosopalgia
Trigeminal prosopalgia (Greek prosopon (face) + algos (pain)) includes facial pain caused by damage to the trigeminal nerve. From the point of view of topical diagnosis, the development of any form of trigeminal prosopalgia is associated with damage to the peripheral trigeminal neuron - the peripheral trigeminal branches, the sensory trigeminal ganglion (located at the base of the skull), the sensory root of the trigeminal nerve that follows it in the direction of the brain stem, as well as those entering the brain stem sensory trigeminal fibers and sensory nuclei of the trigeminal nerve (
).
Despite the difference in the symptomatology of the clinical forms of trigeminal prosopalgia, the features of facial pain are of primary importance for their differentiation, in some cases manifested by prolonged (constant) pain, and in others in the form of paroxysms of pain. Paroxysmal forms of trigeminal pain are traditionally referred to as neuralgia, and non-paroxysmal forms - trigeminal neuropathy. However, non-paroxysmal postherpetic facial pain is also called neuralgia. These forms of facial pain—neuralgia and trigeminal neuropathy—fundamentally differ in their approaches to treatment.
Paroxysmal trigeminal prosopalgia
Paroxysmal facial pain, lasting from several seconds to several minutes, is manifested by trigeminal neuralgia (typical trigeminal neuralgia), trigeminal neuralgia due to multiple sclerosis, and symptomatic trigeminal neuralgia arising from a tumor lesion of the trigeminal nerve.
Until recently, trigeminal neuralgia, not associated with multiple sclerosis and tumor lesions of the trigeminal nerve, was called idiopathic, i.e. occurring for no apparent reason. However, as it was established as a result of serial neurosurgical interventions, the main etiological factor of typical trigeminal neuralgia is compression of the sensory root of the trigeminal nerve by an atypically located arterial or venous vessel.
Trigeminal neuralgia
Trigeminal neuralgia is the most common form of paroxysmal (paroxysmal) facial pain. It is also considered the most excruciating type of facial pain. It manifests itself as attacks of sharp, high-intensity pain in the area of innervation of the trigeminal nerve. The cessation of an attack of facial pain within a few tens of minutes after taking the anticonvulsant carbamazepine radically distinguishes trigeminal neuralgia from most other types of chronic pain. The symptoms of trigeminal neuralgia undergo significant changes as the pain syndrome increases and regresses, reaching its greatest severity at the height of the exacerbation period.
In secondary (symptomatic) forms of trigeminal neuralgia, which arise from tumor damage to the trigeminal nerve, already at the first stage of the disease symptoms may be observed that differ from the typical clinical picture.
Non-paroxysmal trigeminal prosopalgia
Non-paroxysmal trigeminal prosopalgia, manifested by prolonged facial pain, as well as sensitivity deficit (hypesthesia, anesthesia) in the facial area, includes various clinical forms of trigeminal neuropathy, including postherpetic neuralgia (). Most often, the development of trigeminal neuropathy is associated with obvious etiological factors - trigeminal herpes zoster and traumatic injury to the trigeminal nerve. In some cases, trigeminal neuropathy is one of the early manifestations of systemic diseases, in particular systemic scleroderma, systemic lupus erythematosus, sarcoidosis and Lyme disease.
Traumatic trigeminal neuropathy
It is the main form of trigeminal neuropathy, the clinical signs of which are non-paroxysmal facial pain, sensory impairment (numbness) and, very rarely, motor impairment. As a rule, the acute development of these symptoms has an obvious relationship with local pathological processes and iatrogenic effects in the maxillofacial area.
The first sign of traumatic trigeminal neuropathy is acutely developed sensory insufficiency - from mild hypoesthesia to anesthesia, limited to the innervation zone of the affected sensory branch. Subsequently, paresthesia (a feeling of “pins and needles”) and/or non-paroxysmal pain occurs in the same area of the face. Symptoms of sensory loss that accompany facial pain may persist significantly longer than facial pain. In the affected area, hyperesthesia is often detected, as well as pain on palpation of limited areas of facial skin.
Postherpetic trigeminal neuralgia
Trigeminal postherpetic neuralgia is persistent facial pain and/or burning and itching that persists from the time herpetic lesions develop or occurs several weeks after the lesions resolve (delayed postherpetic neuralgia).
Trigeminal postherpetic neuralgia most often develops in patients over 60 years of age. Its occurrence is usually facilitated by:
- late seeking medical help during the period of acute herpes zoster;
- presence of concomitant pathology;
- complicated resolution of rashes - rashes with a hemorrhagic component and secondary pyoderma;
- pronounced residual sensory deficit (“numbness” of the skin after resolution of the rash).
Deafferentation trigeminal neuropathy (prosopalgia)
Deafferentation facial pain (prosopalgia) is the most severe form of trigeminal lesion, manifested by highly intense facial pain, often resistant to conservative therapy, and severe sensory impairment. Develops as a result of significant damage (destruction) of the peripheral or central structures of the trigeminal system.
The concept of “deafferentation trigeminal prosopalgia”, as a general syndromological definition, was proposed by Yu. V. Grachev and Yu. A. Grigoryan (1995) to designate a special form of facial pain that develops as a result of deafferentation in the sensory system of the trigeminal nerve. The pathophysiological term “deafferentation” (de- + lat. afferentis bringing), literally means the separation of the receptor zones of peripheral nerves from the central sensory structures, due to a violation of the integrity or conductivity of nerve fibers.
Typical peripheral forms of deafferentation trigeminal prosopalgia are postherpetic, tumor and iatrogenically caused facial pain (caused by destruction of the ganglion and trigeminal nerve root), and central are two quite rare forms caused by syringobulbia and medulla oblongata infarction.
Diagnosis of trigeminal prosopalgia
The examination of a patient experiencing facial pain should begin with a systematic medical interview, including clarification of the clinical characteristics of the pain and analysis of anamnestic data (
).
The presence of facial pain requires a detailed study of the function of the cranial nerves, and also makes certain additions to the traditional neurological examination. Objective signs of damage to the nervous system of the face are sensory disturbances in the orofacial region - trigger zones, areas of increased and/or decreased sensitivity (Fig. 2, 3), local autonomic disorders, as well as the presence of local palpation pain.
| Rice. 2. Pattern (model) of sensory disturbances characteristic of exacerbation of paroxysmal trigeminal prosopalgia - neuralgia | Rice. 3. Pattern (model) of sensory disturbances characteristic of exacerbation of non-paroxysmal trigeminal prosopalgia - neuropathy |
When conducting palpation examination of the facial area, it is necessary to distinguish between “neuralgic” and “myofascial trigger” (English trigger).
- Neuralgic trigger points or zones (in patients with trigeminal neuralgia) are hyperexcitable areas of the skin and mucous membrane, with mechanical irritation, including light touch, causing a painful attack. At the same time, strong pressure, usually applied by the patient himself, not only does not cause pain, but in some cases leads to a decrease or disappearance of pain.
- Myofascial trigger points (essentially pain points) are located in the soft tissues of the face in the projection of the masticatory muscles. “Pressing” on them is accompanied by localized or radiating pain.
Establishing a specific form of trigeminal facial pain, which usually requires an interdisciplinary clinical examination, involves excluding a number of forms of orofacial pain not associated with damage to the trigeminal nerve, in particular temporomandibular (arthrogenic and myofascial), symptomatic (ophthalmo-, rhino- and odontogenic) and psychogenic prosopalgia.
Treatment of trigeminal prosopalgia
The complexity of treating patients with trigeminal facial pain is due to the need to determine differentiated treatment approaches due to the ineffectiveness of the use of conventional analgesics for certain forms of trigeminal prosopalgia, the frequent need to change standard treatment regimens and, in some cases, the development of “pharmacoresistant” forms of facial pain that require surgical treatment.
The ineffectiveness of traditional analgesics (for example, NSAIDs) prescribed in connection with the development of trigeminal facial pain is an indication for the use of drugs from other groups, in particular carbamazepine, gabapentin or amitriptyline, which have analgesic activity in a number of forms of prosopalgia (scheme of differentiated therapeutic approaches for paroxysmal and non-paroxysmal trigeminal prosopalgia is presented in
).
Over the past few decades, carbamazepine has remained the most effective and affordable drug in the treatment of patients with trigeminal neuralgia. At the same time, the maximum effectiveness of carbamazepine (as a “monotherapy”) appears in the initial period of the disease. The main indication for the use of carbamazepine is paroxysmal pain, covering the area of innervation of the trigeminal nerve. The daily dose of carbamazepine during an exacerbation of trigeminal neuralgia is usually 600–1200 mg (with a 3–4-time dose of the usual dosage form or 2 times of the retard form), but with uncontrolled use by a doctor it often exceeds 2000 mg/day. As neuralgia regresses, a transition is made to maintenance doses of carbamazepine and its gradual withdrawal when facial pain disappears. If there are contraindications for the prescription of carbamazepine or its forced withdrawal, gabapentin is used as an alternative remedy for the elimination of paroxysmal trigeminal pain.
Gabapentin (Gabagamma) is an anticonvulsant that has an analgesic (GABAergic-like) effect. Obviously, this explains its effectiveness in the treatment of patients with neuropathic pain, including paroxysmal and non-paroxysmal trigeminal prosopalgia. Indications for the use of gabapentin (Gabagamma) are paroxysmal facial pain in trigeminal neuralgia and trigeminal neuralgia caused by multiple sclerosis, as well as subacute and chronic non-paroxysmal pain (including deafferentation) in herpetic and traumatic trigeminal neuropathy. The daily dose of Gabagamma in patients with trigeminal prosopalgia can range from 300 to 1500 mg, with a dosage frequency of at least 3 times a day. Gabagamma is used for a long time and is gradually withdrawn. In general, the use of gabapentin (Gabagamma) is considered safer than carbamazepine and especially amitriptyline.
Amitriptyline is a tricyclic antidepressant that is a norepinephrine and serotonin reuptake inhibitor. This drug is widely used for the treatment of postherpetic neuralgia, especially accompanied by a burning sensation. The analgesic effect of amitriptyline usually develops within 1–2 weeks. To reduce the sedative and anticholinergic effects of amitriptyline, treatment begins with small doses of the drug - 10 mg 2-3 times a day (especially at night), gradually increasing the daily dose (due to evening administration) to 75-100 mg. If amitriptyline is insufficiently effective and facial pain persists, gabapentin (Gabagamma) is indicated.
Treatment of patients with damage to the trigeminal nerve also includes the use of high doses of B vitamins in the form of multicomponent preparations “Milgamma” and “Milgamma compositum”. The composition of the drug "Milgamma" (solution for intramuscular administration) includes 100 mg of thiamine and pyridoxine, 1000 mcg of cyanocobalamin and 20 mg of lidocaine. Milgamma compositum is available in the form of tablets containing 100 mg of benfotiamine and pyridoxine. The effectiveness of Milgamma in the treatment of patients with neuropathic pain is associated with inhibition (probably serotonergic) of nociceptive impulses, as well as acceleration of the regeneration of axons and the myelin sheath of peripheral nerves. The regimen for using Milgamma for trigeminal facial pain includes: prescribing Milgamma in the form of a solution for intramuscular administration - 2 ml daily, for 10 or 15 days, then Milgamma compositum - orally, 1 tablet 3 times a day, for 6 weeks.
Yu. V. Grachev , Doctor of Medical Sciences, V. I. Shmyrev, Doctor of Medical Sciences, Professor, Scientific Research Institute of Advanced Promotion of the Russian Academy of Medical Sciences, State Medical University of the Administration of the President of the Russian Federation, Moscow
Treatment of neuritis
Treatment of neuritis in traumatic injuries must be timely and wait-and-see tactics are unacceptable. For mild damage to the inferior alveolar nerve, decongestant therapy (prednisolone, veroshpirone) is sufficient. In case of moderate severity of damage, drugs that improve the conductivity of the nerve trunk (neuromedin) are added to decongestant therapy. In case of severe damage to the nerve trunk, in the absence of positive dynamics in the restoration of sensitivity within 4 months, the patient should be referred for a consultation with a neurosurgeon in order to resolve the issue of the possibility of restoring the anatomical integrity of the nerve trunk.
Various reflexotherapy methods are widely used in the complex treatment of diseases of the peripheral nervous system. In the complex treatment of diseases of the peripheral nervous system, reflexology methods such as electroacupuncture and transcutaneous electrical neurostimulation are widely used.
Prevention of neuritis
Prevention of neuritis of the inferior alveolar nerve is the correct technique for removing teeth, correct diagnosis and correct reading of the radiograph, and a gentle technique for dislocating the roots of teeth in the lower jaw with an elevator.
Symptoms
Inflammation of the trigeminal nerve on the face manifests itself quite clearly through such signs as:
- cutting pains that occur mainly at night;
- pain in the ears, eyes, chin;
- severe spasm;
- inability to lower the lower jaw without additional effort;
- upset sensitivity of nerve endings;
- feeling of numbness;
- formation of edema.
If the problem is inflammation of the trigeminal nerve, the symptoms can be of varying degrees of intensity, which depends on how advanced the disease is and what additional provoking factors there may be.
Abscess after tooth extraction
An abscess after tooth extraction is a long-term complication of a tooth extraction operation that occurs as a result of contamination of the wound surface with microorganisms. When teeth are removed, not only the tissues surrounding the tooth can be injured, but also the mucous membranes of the mouth and cheeks. A fresh wound is a favorable environment and entry point for microorganisms. Therefore, under appropriate circumstances, an abscess may form in the soft tissues or in the hole, which over time and without treatment can “spill” with the formation of phlegmon in several areas.
Causes of abscess
The cause of an abscess may be failure to comply with the rules of asepsis and antisepsis directly during the tooth extraction operation. As a result of incorrect actions by the doctor, infection occurs in the tooth socket and subsequent suppuration. Also, infection of the socket and soft tissues can occur due to the fault of the patient himself if he does not follow all the dentist’s recommendations. The patient must strictly follow the prescribed procedures, otherwise repeated surgery cannot be avoided.
Prevention and treatment of tooth abscess
Prevention of the appearance of an abscess after tooth extraction is basic regular oral hygiene and following all the recommendations of the dentist. Also, preventive measures include visiting the dentist if you experience pain within a few days after tooth extraction. Treatment of an abscess consists of opening and cleaning the abscess cavity, removing purulent formations and prescribing anti-inflammatory therapy. Sometimes the abscess opens on its own, and the pain disappears. But this does not mean that the process has been stopped, so further treatment by a dentist is necessary. Otherwise, the infection may spread to contact areas and intensify the process.
Causes
The factor that caused inflammation of the trigeminal nerve at home cannot be determined. Most often, the disease is activated against the background of:
- strong blow;
- pathological tissue displacement;
- compression of the nerve roots, which is facilitated by protrusions and swollen ligaments;
- reduced immunity.
With a diagnosis such as trigeminal nerve, treatment is most often given to patients suffering from diseases of the oral cavity, chronic infection without therapy. In addition, among the patients there are people who work under air conditioning, in difficult working conditions, where strong toxic effects are possible.