general description
Damage (neuropathy) of the femoral nerve (G57.2) is damage to the femoral nerve in the area where it exits the retroperitoneum onto the thigh behind the inguinal ligament, manifested by weakness of the anterior thigh muscles, numbness or pain along the anterior inner surface of the thigh.
The syndrome is more common in women (65%), the peak incidence is observed at the age of 40–60 years.
Causes: isolated trauma or nerve damage during surgical interventions (surgeries in the pelvic organs, on the hip), compression by retroperitoneal hematoma, tumor, abscess. Toxic effects and metabolic changes in diabetes mellitus are also possible.
Femoral nerve neuropathy
The clinical symptom complex of femoral neuropathy depends on the topic of the process. When pathology occurs at the iliopsoas level, a full range of symptoms develops, including sensory, motor and autonomic-trophic disorders throughout the area innervated by the femoral nerve. In rare cases, with a high division of the nerve, only sensory or only motor disturbances can be observed, sometimes a mosaic picture of motor and sensory disturbances.
Complete neuropathy of the femoral nerve is accompanied by only partial disruption of the iliopsoas muscles, due to the existence of their alternative innervation. Therefore, flexion and supination of the hip are practically not impaired. Paresis of the quadriceps muscle, which is responsible for straightening the leg at the knee joint, is more pronounced. Due to difficulty in extension, patients try not to bend their leg at the knee. Running and walking are difficult, especially when it is necessary to climb stairs. The gait changes. The leg is fixed in a hyperextension position. There is a lack of knee reflex.
Sensory disorders include disorders of tactile and pain perception on the anterior inner surface of the thigh and lower leg, and the medial edge of the foot. In the same zone, trophic and vegetative changes are observed, and irritating pain is possible. When lying on the stomach, symptoms of tension are detected - pain along the front surface of the thigh when trying to raise a straight leg as much as possible (Wassermann's symptom) or bend the leg at the knee joint (Mickiewicz symptom).
Neuropathy of the femoral nerve when it is affected in the area of the inguinal ligament is in general similar to the clinical picture described above. With a high origin of the saphenous nerve, predominantly movement disorders can be observed. Along with the symptoms of tension, pain is detected when pressing in the middle of the inguinal ligament.
Compression of the femoral nerve trunk in Gunter's canal is characterized by painful and tactile hypoesthesia of the skin of the medial edge of the knee joint, the anterior inner surface of the leg and the inner edge of the foot. In the same area, paresthesia and pain are observed, which increase in intensity when the lower leg is extended. The latter forces the patient to walk and stand with the leg slightly bent at the knee. The knee reflex is not impaired. Pain is detected at the point of exit of the saphenous nerve from the adductor canal, Tinel's symptom is the appearance of paresthesia along the nerve when it is tapped with a neurological hammer.
Neuropathy of the femoral nerve with isolated damage to the infrapatellar branch is manifested by paresthesia and numbness of the skin over the patella, tenderness of the point of the saphenous nerve and a positive Tinel sign.
Clinical picture
The disease develops gradually. The first complaint of patients is weakness in the leg (“doesn’t obey, as if it’s giving way”) (100%), difficulty walking (60%). Also concerning is pain in the leg, which increases with extension (90%). Less commonly noted is a decrease in sensitivity along the anterior inner surface of the thigh (40%).
An objective examination of the patient reveals pain below the inguinal fold, along the anterior inner surface of the thigh (70–90%), hypalgesia in the area of innervation of the femoral nerve; decreased knee reflex, weakness of the anterior thigh muscles, muscle atrophy.
Symptoms
The initial signs of the disease are numbness of the skin on the side of the thigh, which gradually covers an increasingly larger area. Sensations of burning, “crawling goosebumps,” tingling and coldness appear, sensitivity to touch and sometimes to changes in temperature, etc. is impaired. Almost immediately, with neuritis (neuralgia) of the lateral cutaneous nerve of the thigh, a pain syndrome occurs. Pain sensations are noticeably reduced in a lying position with bent legs and intensify with movement and in a standing position. The pain may be so severe that it interferes with movement, although muscle function is not impaired.
As the disease progresses, trophic disorders develop: the skin becomes thinner and sweating is impaired.
The disease is characterized by a wave-like pattern, when attacks are followed by periods of rest. Anatomical features of the body can lead to pain and sensory disturbances being felt in different areas of the thigh.
If the pathology develops during pregnancy, it heals spontaneously after childbirth.
Treatment of femoral nerve damage
- Symptomatic therapy (decongestants, analgesics).
- Exercise therapy, novocaine and hydrocortisone blockades.
- Surgical intervention in the inguinal ligament area.
Treatment is prescribed only after confirmation of the diagnosis by a medical specialist.
Essential drugs
There are contraindications. Specialist consultation is required.
- Voltaren (non-steroidal anti-inflammatory drug). Dosage regimen: IM at a dose of 75 mg (contents of 1 ampoule) 1 time/day.
- Ketoprofen (non-steroidal anti-inflammatory drug). Dosage regimen: IM - 100 mg 1-2 times a day; after pain relief, it is prescribed orally in a daily dose of 300 mg in 2-3 doses, a maintenance dose of 150-200 mg/day.
- Fluoxetine (antidepressant). Dosage regimen: the initial recommended oral dose is 20 mg/day. Recommended doses can be increased or decreased until a therapeutic effect is achieved. The drug can be taken regardless of meals.
- Diacarb (a diuretic from the group of carbonic anhydrase inhibitors). Dosage regimen: adults are prescribed 250-500 mg once in the morning for 3 days, on the 4th day - a break.
- Milgamma (B complex of vitamins). Dosage regimen: therapy begins with 2 ml intramuscularly 1 time per day for 5-10 days. Maintenance therapy - 2 ml IM two or three times a week.
Loss of sensation in limbs
Acute loss of sensation in individual limbs can be established in longitudinal zones corresponding to individual nerve roots, or in various areas innervated by individual nerves. The roots are usually damaged as a result of injury by osteophytes of the vertebrae due to spondylosis or herniated disc protrusion. The brachial plexus can be damaged by local trauma (during surgery or an accident involving the shoulder joint area, including birth injuries) and can then become inflamed. The lumbosacral plexus can be damaged during surgery when a retroperitoneal hematoma develops. Peripheral nerves are sensitive to injury or compression in certain classic areas, such as the elbow for the ulnar nerve, the wrist for the median nerve, the knee for the peroneal nerve, and the medial malleolus for the tibial nerve.
Nerve roots
In the upper extremities, reduction or loss of pain and tactile sensation in the first digit and radial surface of the hand raises suspicion of a lesion of the C6 root . A decrease in pain sensitivity on the fourth and fifth fingers, as well as on the ulnar surface of the forearm, indicates damage to the C8 root . If reduced pain sensitivity is detected on the second and third fingers, and sometimes on the radial surface of the fourth finger, it is necessary to think about damage to the C7 root .
In the lower extremities, acute loss of pain and tactile sensation due to damage to the L1 root appears as a longitudinal zone at the level of the groin, which distally reaches the innervation areas of the L2 and L3 , involving the anterior surface of the thigh, and proximally extending over the buttocks. Sensory deficits along the medial and lateral aspect of the tibia indicate involvement of the L4 and L5 . and S2 nerve roots in the pathological process is manifested by a decrease in sensitivity along the back of the thigh and lower leg.
Peripheral nerves
Axillary nerve. localized sensory deficits may be encountered , raising the suspicion of peripheral nerve damage.
The following injuries can lead to damage to the axillary nerve:
- shoulder dislocation;
- damage to the humerus;
- prolonged pressure, stretching, or traction on the arm during anesthesia or sleep.
Localized deficits in pain and tactile sensation over the lower part of the deltoid muscle allow the doctor to easily recognize such a lesion.
Median nerve. Reduction or loss of sensation on the palmar surface of the first three fingers and half of the fourth finger, as well as on the dorsum of the terminal phalanges of the second and third fingers and half of the fourth finger indicates damage to the median nerve.
Acute loss of sensation in the zone of innervation of the median nerve is caused mainly by the following injuries:
- hand lesions;
- lesions of the forearm;
- lesions of the wrist and hand, including puncture and bullet wounds.
Interventions requiring the insertion of needles , especially into the cubital fossa , can also result in median nerve damage that manifests as sensory deficits and pain, often with a burning, causalgic component.
Prolonged compression during anesthesia or sleep can also cause acute injury to the median nerve, manifesting as sensory and motor deficits.
Numbness and tingling along the median nerve, which awakens the patient during sleep and resolves with shaking of the arm and hand, are classic symptoms of carpal tunnel syndrome , usually resulting from repetitive circular movements of the wrist. Patients with diabetes, hypothyroidism, arthritis or acromegaly, and pregnant women are especially prone to developing carpal tunnel syndrome.
Ulnar nerve. Acute sensitivity disorder, indicating damage to the ulnar nerve, is manifested by paresthesia, followed by a decrease in tactile and pain sensitivity on the fifth and ulnar surface of the fourth finger, as well as the ulnar part of the hand to the wrist.
The most common causes leading to damage to the ulnar nerve are:
- fractures and dislocations in the shoulder joint affecting the elbow;
- lacerations;
- pressure on the nerve during anesthesia or while intoxicated.
Radial nerve. In patients with acute radial nerve lesions, sensory deficits may be found on the back of the arm if the nerve is damaged in the axilla. Damage to the radial nerve proximal to the spiral groove of the humerus results in decreased sensation on the distal extensor surface of the forearm. The superficial branch of the radial nerve gives rise to the dorsal digital nerve in the distal forearm, innervating the skin of the dorsal and radial surfaces of the hand and the dorsum of the first four fingers. The radial nerve appears to be the most commonly injured peripheral nerve.
The most common causes of radial nerve injury include:
- shoulder dislocations and fractures;
- prolonged pressure on the nerve (especially in the nerve groove);
- radial neck fractures.
Femoral nerve. Acute damage to the femoral nerve is manifested by a decrease in sensitivity on the anterior and medial surface of the thigh and in the zone of innervation of the hidden nerve (n. saphenus) on the medial surface of the lower leg.
Acute femoral nerve injury can occur as a result of the following injuries:
- fractures of the pelvic and femur bones;
- hip dislocation;
- pressure or traction during hysterectomy;
- delivery using forceps;
- hematoma pressure in the area of the iliopsoas muscle or in the groin.
Paresthesia and loss of sensation in the area of innervation of the hidden nerve can occur as a result of its damage on the medial surface of the knee during medial arthrotomy or during surgical interventions ( coronary artery bypass grafting ).
Obturator nerve. Sensory loss due to obturator nerve injury is detected in a small area of skin on the medial thigh.
The nerve can be damaged in the following situations:
- during surgical interventions on the hip and pelvic organs;
- in cases of obturator hernia;
- secondary to hematoma of the iliopsoas muscle.
Lateral femoral cutaneous nerve. The sudden onset of tingling, numbness or discomfort on the lateral and anterolateral thigh is typical of the lateral femoral cutaneous nerve (meralgia paresthetica). Hyperesthesia is replaced by hypoesthesia. The discomfort or pain may be bilateral.
This nerve can be damaged in the following cases:
- due to compression by the inguinal ligament;
- with hemorrhage in the iliopsoas muscle;
- when obese patients wear too tight clothes.
Sciatic nerve. Acute sensitivity disorders, involving the outer surface of the leg, as well as the dorsal, plantar and inner surfaces of the foot, appear with acute lesions of the sciatic nerve. The distribution of sensory deficits reflects the areas of cutaneous sensation provided by the two branches of the sciatic nerve: the peroneal and tibial nerves .
Acute sciatic nerve injury can occur when:
- fractures or dislocations of the hip;
- operations on the hip joint;
- other pathological conditions of the pelvic organs, including gunshot wounds or injections into areas close to the sciatic nerve.
Peroneal nerve. When the common peroneal nerve is damaged at the level of the head of the fibula, sensitivity is impaired on the lateral surface of the leg and the dorsum of the foot. Sometimes only the superficial branch of the peroneal nerve is damaged, which is manifested by a decrease in pain and tactile sensitivity in the more distal parts of the lateral surface of the leg. When the deep branches of the peroneal nerve are affected, a small area of skin between the first and second toes may be identified with decreased sensitivity to pain and touch.
Most peroneal nerve injuries are traumatic in nature and are usually caused by:
- pressure applied to the upper and outer surfaces of the leg;
- stretching in the hip and knee joints;
- surgical operations in the knee joint.
Tibial nerve. Acute injury to the tibial nerve leads to sensory disturbances on the lateral surface of the posterior part of the leg, innervated by its branch, the medial sural cutaneous nerve. Additional branches of the tibial nerve supply the skin of the lateral heel, the lateral aspect of the foot (sural nerve), and the sole, with the medial two-thirds of the plantar being innervated by the median plantar nerve and the lateral third by the lateral plantar nerve.
The tibial nerve is most often damaged in the popliteal fossa, at the level of the ankle joint or foot.
Damage to the tarsal tunnel, where the nerve crosses the medial malleolus, causes loss of sensation in the toes and dorsum of the foot.
Plexopathy.
Acute sensorimotor deficits indicating multiple nerve damage in a separate upper or lower extremity raise the suspicion of plexopathy .
Brachial plexus plexopathy. The acute appearance of a feeling of tingling, numbness and pain, followed after a few hours or days, as a rule, by muscle weakness and patch-type hypoesthesia in the area of the shoulder girdle and proximal muscles of the shoulder, is typical for damage to the brachial plexus (amyotrophic neuralgia). Acute brachial plexopathy may be caused by trauma in which the arm is excessively abducted, or may occur secondary to tractional movements of the arms, including injuries during childbirth. Damage to the brachial plexus can occur in epidemic form.
Brachial plexus plexopathy can develop after:
- infections;
- vaccinations;
- parenteral administration of serums;
- may occur as a complication of coronary artery bypass grafting.
In some patients, no apparent cause for plexopathy can be identified.
Plexopathy of the lumbosacral plexus is recognized by sensorimotor deficits and pain in the lower extremities. In acute lumbar plexus plexopathy , a common cause, in addition to trauma, is retroperitoneal hemorrhage.
Recommendations
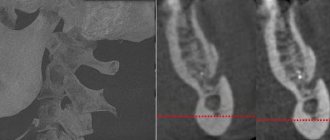
Consultation with a neurosurgeon and magnetic resonance imaging of the retroperitoneum are recommended.
| • | Leading specialists and institutions for the treatment of this disease in Russia: |
| Doctor of Medical Sciences, Head of the Department of Russian State Medical University, Professor, Academician of the Russian Academy of Medical Sciences Gusev E.I. | |
| • | Leading specialists and institutions for the treatment of this disease in the world: |
| G. AVANZINI, Italy. |
Incidence (per 100,000 people)
| Men | Women | |||||||||||||
| Age, years | 0-1 | 1-3 | 3-14 | 14-25 | 25-40 | 40-60 | 60 + | 0-1 | 1-3 | 3-14 | 14-25 | 25-40 | 40-60 | 60 + |
| Number of sick people | 0 | 0 | 0.1 | 10 | 10 | 15 | 15 | 0 | 0 | 0.1 | 10 | 10 | 15 | 15 |