Classification of jaw atrophy and bone tissue phenotypes
Depending on the position of the jaw, there are two groups that characterize the atrophic state of the upper and lower jaws:
- According to Schroeder for the top row. There are three types of upper jaws with missing teeth, resulting in thinning bone tissue:
- The jaw tubercles are very noticeable. These gaps can be filled with prosthetic implants because the physical abnormalities are not noticeable. The palate is deep, and the bend of the mucosa is quite large.
- The alveolar processes are not clearly defined. The depth of the sky is average. Prosthetics are possible, but their fixation may deteriorate after muscle tissue overstrain.
- The bone at the base of the jaw is seriously destroyed. The ridges and tubercles of the alveoli are smooth, and the palate is transformed into a flat shape. The fold of the mucous membrane becomes at the level of the palate and does not hold its shape well. As a result of pathology, prosthetic structures cannot be secured.
- According to Keller for the bottom row:
- The alveolar elements are slightly smoothed, but are visible throughout the entire jaw. At the beginning of the alveolar ridge, muscle tissue and a fold of mucous membrane are attached. Installation of the prosthesis is not difficult.
- The ridge becomes noticeable and takes on a sharper shape. The muscles are attached to the crest. In most cases, the implant causes discomfort and pain.
- It is often observed in people who have undergone early removal of lateral teeth. The alveoli around the molars and premolars become thinner. In the central part, the bone tissue does not lose volume. Creating artificial teeth is possible, but there is a possibility of the implant slipping when chewing.
- In the area of the frontal incisors, a pronounced atrophic process is observed, while the lateral dentition remains preserved. Fixation of the prosthesis cannot be done, because the likelihood of its displacement increases.
Causes
Doctors call the main cause of retinal atrophy is ischemia, during which the nutrition of the retinal tissue located between the vitreous body and the choroid of the eyeball deteriorates. Ischemia is understood as a weakening of blood supply or its complete cessation. As a result, acute or chronic oxygen starvation of tissues occurs, leading to gradual depletion of the retina, that is, atrophy.
Until now, ophthalmologists have not been able to finally formulate a list of internal and external factors under the influence of which retinal atrophy begins. In the list of provocateurs of its development
include phenomena that negatively affect the functioning of the circulatory system as a whole:
- prolonged smoking;
- carriage of cytomegalovirus;
- deficiency of vitamins, especially carotenoids and antioxidants (vitamin C, E);
- excess in the diet of saturated and solid fats, as well as foods rich in cholesterol;
- chronic intoxication of the body due to living in environmentally unsafe regions;
- systemic chronic diseases, including diabetes mellitus, hypertension and systemic lupus erythematosus;
- serious neck and head injuries.
The exact causes of the disease remain unknown in most cases. Ophthalmologists tend to call retinal atrophy a natural age-related process, because the concept of “poor” blood supply in the elderly can be applied to almost all organs. However, this does not mean that the pathology can be ignored: without supportive therapy, it can lead to complete blindness.
Implantation for jaw bone atrophy
Several techniques are used to quickly restore the dentition. For example, installation of bridges or removable dentures. However, these methods cannot restore the required load on the bone, since the gums or healthy teeth are loaded.
Implantation helps relieve pressure on the bone and prevent further thinning.
In advanced cases, when the atrophy of the jaw bone tissue is significant, restoration of the bone structure is used before implantation. Various techniques are used, for example, sinus lifting, separation of the alveolar process, and the introduction of artificial tissue. Six months after the operation, implants are inserted. As a result, bone density and volume are preserved.
Implantation with immediate loading is considered a new technique. Special materials are installed not in the alveolar process, but in the basal part of the jaw. Thanks to this, the bone is immediately loaded, and the metabolism is not disrupted. Suitable only if three or more teeth in a row are missing.
Diagnostics
The diagnosis of retinal atrophy can be made after examining the fundus. The disease is characterized by very specific signs: increased pigmentation of the macula, scattered or merging atrophic foci on the retina in the dry form of the disease, or swelling of the retina with increased vascular pattern in the wet form. The patient’s subjective complaints also help determine the diagnosis.
To confirm the diagnosis, instrumental methods are used:
- biomicroscopy of the eye, during which the doctor examines the internal structures of the organs of vision through a special slit lamp under multiple magnification;
- visometry - measurement of visual acuity using special tables: the patient looks alternately with both eyes and names the images that the doctor points to;
- angiography - radiographic examination of the blood vessels of the eyes with contrast;
- Ultrasound scanning with Dopplerography, revealing vascular obstruction;
- CT scan of the eyes, determining the boundaries of retinal ischemia and atrophy.
If vascular anomalies are detected, additional tests may be prescribed: blood tests for glucose and cholesterol, general clinical laboratory tests of blood and urine, etc. An ophthalmologist writes out referrals for examinations. In the future, doctors of other specializations may be involved: therapists, surgeons, phlebologists and cardiologists.
Types and degrees of jaw bone atrophy
Deformation of the jaw bone develops with different intensity:
- I degree. At the beginning of the disease, it is eliminated by prosthetics. The implant performs its function, the blood supply is not disrupted.
- II degree. The clinical picture is intensifying. The mucous membrane of the jaw begins to shrink. Dental prosthetics are possible, but additional treatment is required before this can be done.
- III degree. The contour of the bone tissue is smoothed both on the inside of the mouth and on the side of the chin.
When selecting a treatment method, this characteristic of the development of pathology should be taken into account. Bone tissue decreases not only in height, but also in width. The bone becomes short and thin.
Vaginal atrophy: etiological aspects and modern approaches to therapy
Postmenopause is characterized by an estrogen deficiency state in women, caused by age-related decline and then cessation of ovarian function [1]. As is known, any epithelial tissue reacts to changes in the hormonal environment surrounding them in a similar way, but none of them can compare with the epithelium of the vaginal vault and cervix in the speed and clarity of the reaction to hormones, primarily to sex steroids [2]. Thus, the urogenital tract is particularly sensitive to decreased estrogen levels and approximately half of all postmenopausal women experience symptoms associated with urogenital atrophy (UGA), affecting sexual function and quality of life [3]. The clinical picture of urogenital disorders in the menopause includes symptoms associated with vaginal atrophy (vaginal atrophy (VA)) and urination disorders (cystourethral atrophy). Unlike vasomotor symptoms, which usually resolve over time, symptoms of vaginal atrophy typically begin in premenopause and progress postmenopause, leading to functional and anatomical changes [4]. 15% of premenopausal women and 40–57% of postmenopausal women experience symptoms of VA [5], such as vaginal dryness 27–55%, burning and itching 18%, dyspareunia 33–41%, as well as increased susceptibility to infectious diseases of the organs pelvis 6–8% [4], which significantly worsens health and negatively affects the general and sexual quality of life [6]. 41% of women aged 50–79 years have at least one of the symptoms of VA [10].
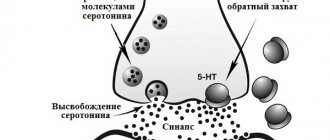
The walls of the vagina consist of three layers: the inner layer, which is lined with stratified squamous epithelium; middle muscular and outer connective tissue layers (or fibrous layer). Atrophic processes involving the connective tissue and muscle structures of the vagina, as well as the muscles of the pelvic floor, urethra, and bladder, are especially pronounced in the vaginal mucosa. It is known that in women, the vaginal mucosa consists of four main layers of epithelial cells: the basal layer; parabasal layer (or mitotically active); intermediate glycogen-containing layer; superficial (flaking) [11]. Estrogen receptors are located mainly in the basal and parabasal layers of the vagina and are practically absent in the intermediate and superficial layers [10]. Estrogen deficiency blocks the mitotic activity of the basal and parabasal layers of the epithelium of the vaginal wall, and, consequently, the proliferation of the vaginal epithelium [12]. The consequence of the cessation of proliferative processes in the vaginal epithelium is the disappearance of glycogen, a nutrient medium for lactobacilli, thus its main component, lactobacilli, is completely eliminated from the vaginal biotope [3, 12].
It is known that peroxide-producing lactobacilli, which predominate in vaginal microbiocinosis in women of reproductive age, play a key role in preventing the occurrence of diseases of the urogenital tract [10, 11]. Due to the breakdown of glycogen, which is formed in the vaginal epithelium, provided there is a sufficient amount of estrogens, lactic acid is formed, providing an acidic vaginal environment (within pH fluctuations from 3.8 to 4.4). Such a protective mechanism leads to suppression of the growth of pathogenic and opportunistic bacteria. During the postmenopausal period, the vaginal mucosa loses these protective properties, becomes thinner, and is easily injured, followed by infection not only by pathogenic, but also by opportunistic microorganisms.
Estrogens are the main regulators of physiological processes in the vagina. Estrogen receptors α are present in the vagina in premenopausal and postmenopausal women, while estrogen receptors β are completely absent or have low expression in the vaginal wall of postmenopausal women. The highest density of estrogen receptors is observed in the vagina and decreases in the direction from the internal genital organs to the skin. The density of androgen receptors, on the contrary, is low in the vagina and higher in the area of the external genitalia. Progesterone receptors are found only in the vagina and the epithelium of the vulvovaginal junction [10]. Since the cells of the vaginal stroma contain estrogen receptors, collagen, which is part of the connective tissue of the vaginal wall, is an estrogen-sensitive structure, the content of which decreases as estrogen deficiency progresses. Since estrogen receptors are located not only in the epithelium and stroma of the vaginal wall, but also in the vascular endothelium, in postmenopause there is a decrease in blood circulation in the vagina to the level of varying degrees of ischemia. In addition, estrogens are vasoactive hormones that increase blood flow by stimulating the release of endothelial mediators such as nitric oxide, prostaglandins, and endothelial hyperpolarizing factor. Such a progressive decrease in blood flow in the vaginal mucosa leads to hyalinization of collagen and fragmentation of elastic fibers, increasing the amount of connective tissue [12].
Estrogen receptors have also been found on autonomic and sensory neurons in the vagina and vulva. A study by TL Griebling, Z. Liao, PG Smith revealed a decrease in the density of sensory nociceptive neurons in the vagina during estrogen treatment. This feature may be useful in addressing the discomfort associated with VA, namely in relieving symptoms such as burning, itching and dyspareunia that many postmenopausal women experience [5, 10].
Atrophy of the vulvar and vaginal mucosa is characterized by thinning of the epithelium, decreased vaginal folding, pallor, the presence of petechial hemorrhages, and signs of inflammation. Also, due to involutive changes, there is a loss of tissue elasticity, subcutaneous fat, loss of pubic hair, and a decrease in the secretory activity of the Bartholin glands [3, 13, 14]. Typically, doctors diagnose vulvar and vaginal atrophy based on a combination of clinical symptoms and visual examination. Researchers are increasingly insisting on more objective and reproducible diagnostic methods, without excluding subjective patient complaints [13]. Historically, to diagnose VA, two main objective methods of diagnosing and assessing the effectiveness of treatment are required: vaginal pH, as well as calculation of the vaginal maturation index (VII, the predominance of cells of the basal and parabasal layers) [12, 13]. Interestingly, the degree of atrophic changes, as measured by the maturation index, does not always correlate with symptoms [15]. In a study of 135 menopausal female volunteers who completed a symptom assessment followed by a rating of “vaginal health” (assessing vaginal color, discharge, epithelial integrity and thickness, pH) and a maturation index measurement, researchers found a weak correlation between physical symptoms and maturation index.
Hormonal changes that occur throughout the life cycle affect the vaginal flora from birth to postmenopause. A decrease in estrogen during perimenopause and postmenopause leads to a decrease in the number of lactobacilli and a change in flora in general. According to SL Hillier, RJ Lau, a detailed analysis of the vaginal microflora of 73 postmenopausal women who did not take hormonal therapy did not reveal lactobacilli in 49% of cases. And among those in whom they were detected, the concentration of the latter was 10–100 times less than in premenopausal women [15]. In postmenopause, the most common microorganisms were anaerobic gram-negative rods and gram-positive cocci.
Despite the above, some women experience wasting symptoms soon after menopause, while others do not experience them until later in life. Among the factors that may increase the risk of developing urogenital atrophy, smoking is one of the most studied. Smoking has a direct effect on the squamous epithelium of the vagina, reducing the bioavailability of estrogen and reducing blood perfusion. Other hormonal factors that tend to be important are the levels of various androgens such as testosterone and androstenedione. It has been suggested that after menopause, women with higher levels of androgens, which support sexual activity, have fewer changes associated with atrophy [12]. In addition, VA is observed more often in women who have never given birth vaginally [16].
Considering the pathogenesis of the disease, estrogen therapy is the gold standard of treatment. All clinical guidelines for the treatment of UGA agree that the most common and effective treatment method is systemic or local hormonal therapy with estrogen in various forms, as it quickly improves the maturation index and thickness of the vaginal mucosa, reduces vaginal pH and eliminates the symptoms of VA [ 3, 11–13]. To treat UGA combined with symptoms of menopause, systemic hormonal therapy is used. In other cases, local treatment is preferred, which avoids most systemic side effects [12, 13]. Studies have shown that systemic hormone replacement therapy eliminates symptoms of VA in 75% of cases, while local therapy eliminates symptoms in 80–90%.
Estrogen-containing preparations for local use, presented in the form of cream, tablets, pessaries/suppositories, vaginal ring, may contain estriol, conjugated equiestrogens, estradiol or estrone. Of the three natural estrogens in the human body, estriol has the shortest half-life and the least biological activity. In Russia, there is many years of experience in the local use of estriol-containing drugs that have a pronounced colpotropic effect. Given the weak proliferative effect on the endometrium when using estriol, additional administration of progestogen is not required. Numerous studies have shown that daily use of estriol at a dose of 0.5 mg has a noticeable proliferative effect on the vaginal epithelium. Local use of estriol-containing drugs is a safe and effective approach to the prevention and treatment of VA, which has no restrictions on age and duration of treatment. Currently, in European countries there is a trend towards local use of low doses of estrogens estriol and estradiol.
In 2006, a Cochrane systematic review analyzed 19 clinical trials involving 4,162 postmenopausal women, randomized to vaginal estrogen products, and evaluating the efficacy, safety, and acceptability of therapy as an endpoint. Fourteen studies compared the safety of different drugs, seven focused on side effects and four on treatment safety and effects on the endometrium. Seven studies included placebo groups, and all showed improvement in patients taking hormonal therapy (Table).
The results of the analysis show that vaginal estradiol tablets are more effective than the vaginal ring and that both treatments are superior to placebo in relieving dyspareunia, vaginal dryness and itching. Conjugated equine estrogens (CEE) vaginal cream is superior to moisturizing creams in relieving dryness and increasing elasticity and blood flow to the vagina. However, no differences were found between the three therapies analyzed (CLE cream, estradiol tablets, and estradiol-releasing ring) with respect to parabasal cell count, karyopyknotic index, maturation index, and vaginal health index. In addition, there are also reports of no significant differences in endometrial thickness, hyperplasia, and side effects between the vaginal ring, cream, or tablet. However, a slight risk of vaginal bleeding was described in all studies that used different methods of topical estrogen therapy, as well as a possible increased risk of candidiasis [16].
A meta-analysis by Cardozo et al showed that vaginal estrogen administration is an effective treatment for VA. The combination of local and systemic therapy allows you to achieve results in a shorter time. In addition, low doses of topical estrogens: estradiol or estriol are as effective as systemically administered ones. A transdermal patch with a daily dose of 14 μg of estradiol has been shown to have similar effects on vaginal pH and maturation index as a vaginal ring with 7.5 μg of estradiol [17].
The beneficial therapeutic effect of topical hormonal therapy has also been noted in situations beyond the treatment of VA, such as reducing the risk of recurrent urinary tract infections and the development of overactive bladder. Based on the above, the estradiol-releasing ring has been approved as a treatment for dysuria and urge urinary incontinence. While systemic hormonal therapy, on the contrary, increases the incidence of stress urinary incontinence and kidney stones [10].
Thus, local therapy has a number of advantages compared to systemic administration of drugs. It avoids primary metabolism in the liver, has minimal effects on the endometrium, has a low hormonal load, minimal side effects, does not require the addition of progestogens, and has a mainly local effect.
From a practical point of view, and due to the similar effectiveness and safety of all topical estrogen preparations, the patient should be able to choose the drug that she considers most suitable for her. She should be informed that the effect is achieved after one to three months of treatment. Additional administration of progestogens is not necessary when using local forms of estrogens [18]. A 2009 review of topical hormone therapy stated that no studies observed endometrial proliferation after 6 to 24 months of estrogen use, so the literature thus provides reassurance regarding the safety of low-dose vaginal preparations with estrogen and non-estrogens. supports the concomitant use of systemic progestogens to protect the endometrium [13].
In addition to the above treatment methods for VA, today there are such as therapy using dehydroepiandrosterone, selective tissue estrogen complexes, selective estrogen receptor modulators and non-hormonal treatment methods, as well as combination drugs containing ultra-low-dose estriol and lactobacilli.
In the work of U. Jaisamrarn et al. evaluated for the first time the efficacy and tolerability of ultra-low dose estriol (0.03 mg) in combination with viable Lactobacillus acidophilus in the short and long term for the treatment of symptoms of VA. It was found that the combination of estriol and lactobacilli for 12 weeks was sufficient to achieve statistically and clinically significant results, including improvement in objective parameters (VIS, pH, proportion of lactobacilli in the vaginal microflora), as well as the quality of life of women [19].
A large number of publications are devoted to the use of intravaginal dehydroepiandrosterone (DHEA) gel for the treatment of VA [8]. DHEA is a sex hormone precursor that is produced by the adrenal glands and ovaries in addition to testosterone and estrogens. Subsequently, it undergoes biotransformation in peripheral tissues: in the brain, bones, mammary glands and ovaries. To date, specific receptors for DHEA have not been found, and therefore it is assumed that its action occurs through conversion to androgens and/or estrogens and interaction with their receptors, respectively. To date, most of the evidence for the beneficial effects of vaginally administered DHEA reported in five publications comes from a single randomized trial conducted by Labrie and colleagues. DHEA was used vaginally by 218 postmenopausal women for 12 weeks. Women were assigned to a placebo group taking 0.25% (3.25 mg), 0.5% (6.5 mg) or 1.0% (13 mg) vaginal cream daily. In patients receiving DHEA therapy, vaginal atrophy disappeared, while minimal changes in serum steroid hormone levels were observed, which remained within the normal range characteristic of postmenopause. Also in this study, there were positive effects on four aspects of sexual function: desire/interest, arousal, orgasm, and dyspareunia. DHEA 0.5% (6.5 mg) cream was found to be optimal for the treatment of vaginal atrophy and did not significantly affect serum estrogen levels [20].
Among the selective estrogen receptor modulators (SERMs), ospemifene is the most advanced drug available. A 12-week, three-phase randomized trial involving 826 postmenopausal women examined the effectiveness of this drug at a dose of 30 mg, 60 mg compared with placebo. At weeks 4 and 12, ospemifene at the previously reported doses showed statistically significant increases in superficial cell counts, decreases in parabasal cells, and decreases in vaginal pH compared with placebo. Vaginal dryness was significantly reduced in both the 30 mg and 60 mg groups compared to placebo at week 12, while dyspareunia was reduced only in the 60 mg group. The study found that the side effect of hot flashes occurred in 9.6%, 8.3% and 3.4% of participants in the ospemifene 30 mg, 60 mg and placebo groups, respectively. Endometrial thickness from baseline to week 12 changed on average by 0.42 mm, 0.72 mm and 0.02 mm in participants in the above groups, respectively [21].
The combination of conjugated estrogens and the selective estrogen receptor modulator bazedoxifene, known as tissue selective estrogen complex (TSEC), was studied in a phase 3 study where 601 women were randomized to receive daily therapy: 20 mg bazedoxifene plus conjugated estrogens. .45 mg (BZA/CE), or bazedoxifene 20 mg plus 0.625 mg conjugated estrogens, or bazedoxifene 20 mg and placebo. The study found an increase in the proportion of superficial cells and a decrease in the proportion of parabasal cells from baseline to week 12, to a greater extent in the BZA/CE group compared with placebo and BZA alone. Vaginal pH did not change significantly from baseline to the end of the study in the BZA or placebo group, but decreased significantly in both BZA/CE groups. However, the decrease in vaginal pH was significantly lower in the BZA/CE 20 mg/0.625 mg group than in the placebo group. Most bothersome symptoms were significantly reduced by week 12 compared with placebo in the BZA/CE 20 mg/0.625 mg group, but not in the BZA/CE 20 mg/0.45 mg group. There were no significant differences in side effects or study discontinuations between groups. However, a higher incidence of vaginitis was noted in the treatment groups (BZA/CE) compared with placebo [22]. Thus, TSEC, namely bazedoxifene in combination with conjugated estrogens, represents an alternative to progestin therapy to protect the endometrium from estrogen stimulation while maintaining the beneficial effects of estrogen on menopause-related symptoms.
Despite the listed methods of treating VA, one should not forget about preventing the disease. Maintaining regular sexual activity is recommended in general for all women and in particular for menopausal women. This is because sexual intercourse improves blood circulation in the vagina, and seminal fluid also contains sex steroids, prostaglandins and essential fatty acids, which help maintain vaginal tissue [12].
Although the official prevalence of vaginal atrophy varies depending on the size and individual characteristics of the population studied, an increasing number of women are affected by this condition as the population ages. One study conducted by foreign colleagues showed that more than 60% of women experience symptoms of VA 4 years after postmenopause. However, only 4% of women aged 55–65 years associate the above complaints with vaginal atrophy, 37% know that these symptoms are reversible, and 75% of women believe that symptoms of VA negatively affect their lives. Given the sensitive nature of these symptoms, patients are hesitant to seek medical help and consequently suffer from progressive symptoms [10, 23]. Only 25% of women with symptoms of vaginal atrophy seek medical help. VA is a chronic and progressive condition [10]. A significant number of women with symptoms of VA do not even realize that effective treatment is possible. Timely informing patients about the causes of the above symptoms and the possibilities for eliminating them can quickly improve the condition of women and restore their interest in life and its quality. Thus, the problem of maintaining health and preventing diseases caused by aging has acquired particular importance in recent years. Due to its relevance, new drugs for the treatment of VA are currently being developed and introduced, which will allow an individualized approach to patient treatment.
Literature
- Vikhlyaeva E. M. Guide to gynecological endocrinology. M.: Medical Information Agency, 1997. pp. 227–360.
- Urogenital disorders in menopause (clinical presentation, diagnosis, hormone replacement therapy). dis. Dr. med. Sci. M., 1998.
- Santiago Palacios. Managing urogenital atrophy // Maturitas. 2009; 63:315–318.
- Sinha A., Ewies AAA Non-hormonal topical treatment of vulvovaginal atrophy: an up-to-date overview // Climacteric. 2013; 16: 305–312.
- Griebling TL, Liao Z., Smith PG Systemic and topical hormone therapies reduce vaginal innervation density in postmenopausal women // Menopause. 2012; 19: 630–635.
- Frank SM, Ziegler C., Kokot-Kierepa M., Maamari R., Nappi RE Vaginal Health: Insights, Views & Attitudes (VIVA) survey - Canadian cohort // Menopause Int. 2012.
- Rosano GMC, Vitale C., Silvestri A., Fini M. Metabolic and vascular effect of progestins in postmenopause // Maturitas. 2003; 46: 17–29.
- Hextall E. Esrogens in the funtion urethral tract // Maturitas. 2000; 36:83–92.
- Manukhin I. B., Tumilovich L. G., Gevorkyan M. A. Clinical lectures on gynecological endocrinology. M., 2003.
- Management of symptomatic vulvovaginal atrophy: 2013 position statement of The North American Menopause Society // The North American Menopause Society. 2013; 20(9):888–902.
- James H. Pickar. Emerging therapies for postmenopausal vaginal atrophy // Maturitas. 2013; 75:3–6.
- Camil Castelo-Branco, Maria Jes´us Cancelo, Jose Villero, Francisco Nohales, Maria Dolores Juli´a. Management of post-menopausal vaginal atrophy and atrophic vaginitis // Maturitas. 2005; 52:46–52.
- Sturdee DW, Panay N. Recommendations for the management of postmenopausal vaginal atrophy // Climacteric. 2010; 13:509–522.
- Basaran M., Kosif R., Bayar U., Civelek B. Characteristics of external genitalia in pre-and postmenopausal women // Climacteric. 2008; 11: 416–421.
- Paul Nyirjesy. Postmenopausal Vaginitis. Current Infectious Disease Reports. 2007; 9:480–484.
- Suckling J., Lethaby A., Kennedy R. Local oestrogen for vaginal atrophy in postmenopausal women // Cochrane Database Syst Rev. 2006.
- Gupta P., Ozel B., Stanczyk FZ, Felix JC, Mishell Jr. DR The effect of transdermal and vaginal estrogen therapy on markers of postmenopausal estrogen status // Menopause. 2008; 15(1)): 94–97.
- Pitkin J., Rees M. British Menopause Society Council. Urogenital atrophy // Menopause Int. 2008; 136–137.
- Jaisamrarn U., Triratanachat S., Chaikittisilpa S., Grob P., Prasauskas V., Taechakraichana N.. Ultra-low-dose estriol and lactobacilli in the local treatment of postmenopausal vaginal atrophy // Climacteric. 2013; 16: 347–355.
- Labrie F., Archer D.F., Bouchard C. et al. Intravaginal dehydroepiandrosterone (prasterone), a highly efficient treatment of dyspareunia // Climacteric. 2011; 14: 282–288.
- Bachmann GA, Komi JO The Ospemifene Study Group. Ospemifene effectively treats vulvovaginal atrophy in postmenopausal women: results from a pivotal phase 3 study // Menopause. 2010; 17(3):480–486.
- Kagan R., Williams RS, Pan K., Mirkin S., Pickar JH A randomized, placebo-and active-controlled trial of bazedoxifene/conjugated estrogens for treatment of moderate to severe vulvar/vaginal atrophy in postmenopausal women // Menopause . 2010; 17(2):281–289.
- Kingsberg SA, Krychman ML Resistance and barriers to local estrogen therapy in women with atrophic vaginitis // J Sex Med. 2013; 1567–1574.
A. V. Glazunova S. V. Yureneva1, Doctor of Medical Sciences, Professor
FSBI NTs AGiP im. V. I. Kulakova Ministry of Health of the Russian Federation, Moscow
1 Contact information
Abstract. According to forecasts to 2030 there will be 1.2 bln women in postmenopause. The state of estrogen deficiency in climacterical period cause vaginal atrophy with 15–57% of women. The latest data on the problem of pathogenesis, clinical manifestations and therapy of this state are provided in review.
Jaw bone atrophy with age
One of the factors influencing the defect is age-related changes. As a rule, in patients over 60 years of age, atrophy is a common process. This is explained by the fact that the lack of minerals and cell nutrition affects metabolism and teeth fall out. The blood supply to bone tissue is disrupted and the required amount of oxygen is not supplied. This causes a change in pressure on the bone.
Symptoms of atrophy
The patient is concerned about decreased visual acuity, which is not amenable to optical correction.
In this case, visual disturbances can manifest themselves in the form of separate “spots” before the eyes or a sensation of narrowing of the fields up to “tubular vision”. Color vision disturbances are also possible.
The dynamics of symptoms may vary. Sometimes atrophy progresses steadily without treatment, even to the point of blindness. Also, the atrophic process can be suspended. In this case, the decrease in vision can be significant, but complete blindness does not develop.
Jaw bone atrophy after tooth extraction
The most common cause of the disease is the loss of a tooth or dentition. A few months after extraction, if prosthetics are untimely, the process of reducing the jawbone begins due to pressure on the alveolar process. Within a year, the deformation can reach its maximum.
The consequences of bone tissue deficiency are expressed in the deterioration of speech, changes in the proportions of the face and its shape, and the appearance of severe wrinkles in the mouth area. At an advanced stage, patients experience displacement of the dentition, loss of opposite and/or adjacent teeth. Because of this, the likelihood of implantation failure increases.
Treatment methods
After confirming the diagnosis, retinal atrophy is treated according to an individual regimen. It depends on the identified characteristics of the disease, existing chronic ailments and the general condition of the body. In mild cases, when the intensity of the ischemic process is minimal and irreversible changes have not occurred, maintenance therapy is prescribed. It consists of medications for oral administration:
- vitamin complexes enriched with antioxidants and retinol;
- medicines to strengthen the walls of blood vessels;
- agents that reduce ischemic processes and restore blood circulation in the head area.
Conservative treatment is complemented by a diet aimed at restoring blood fluidity, reducing the risk of thrombosis, and strengthening vascular walls. Patients are advised to enrich their diet with foods rich in substances beneficial to the eyes:
- beta-carotenes
- yellow and orange vegetables and fruits (carrots, pumpkin, yellow tomatoes, citrus fruits, apricots and peaches, persimmons); - lutein
- all types of cabbage, chicken and quail eggs, avocado and almost all citrus fruits; - niacin
- chicken and turkey fillet, any liver, tuna and salmon, lean pork and beef, peanuts and brown rice; - omega-3 acids
- all fatty fish; - vitamins C and E
- almonds, bell peppers and currants, citrus fruits and herbs.
To maintain vascular tone, it is important to include more cereals and grains in the menu. They should make up at least 1/3 of the diet. It is better to replace solid animal fats, including butter and heavy cream, with vegetable oils - olive, sesame, sunflower.
Important! A well-designed and carefully followed diet can stop atrophic processes in the retina and partially restore its functions.
Wet retinal atrophy has a more aggressive form and therefore requires radical treatment. In addition to the previously mentioned supportive drugs, invasive methods are used to eliminate it:
- intraocular injections of drugs
that help restore microcirculation, remove excess fluid from areas adjacent to the retina, eliminating retinal swelling; - injection sclerosis of vessels
formed in the area of atrophy using the drug Visudyne and laser stimulation; - laser coagulation of the retina
, aimed at preventing its detachment, eliminating scar tissue and destroying abnormal vessels.
If the disease becomes aggressive, a full-fledged surgical operation is performed aimed at restoring metabolic processes in the retina and normalizing blood supply. For this purpose they do:
- vitrectomy - the vitreous body is removed and replaced with a gel-like polymer, which tightly presses the retina to the vascular substrate and prevents its detachment;
- vasoreconstruction - restoration of blood supply using microsurgical restoration of the patency of the ocular vessels;
- revascularization - surgical removal of newly formed vessels.
After the intervention, long-term rehabilitation and lifelong use of drugs aimed at inhibiting the process of angiogenesis, that is, uncontrolled proliferation of blood vessels, are required.
3. Symptoms, diagnosis
The following groups of symptoms are considered to be the axial, main ones in the clinic of multiple system atrophy. The ability to coordinate complex movements is gradually lost and, as in Parkinson's disease, involuntary movements (tremors) appear against the background of increased muscle tone. Gait is disrupted and motor skills become increasingly erratic (ataxia). In addition, they suffer from the so-called autonomic functions controlled by the peripheral nervous system: certain problems arise and are aggravated with urination and defecation, water and temperature balance of the skin, breathing (especially during sleep), blood pressure (which, when taking a vertical position, can manifest itself as dizziness and short-term loss of consciousness with fall); Speech and sexual functions are disrupted and degraded, fixation of gaze becomes difficult and visual acuity decreases; the productivity of the lacrimal, salivary and sweat glands decreases. Dementia is progressing. In most cases, after a few years the patient has to be disabled. The process is fatal; in the terminal stage, patients, as a rule, are in a purely vegetative status.
Taking into account the polymorphism of possible symptoms, multiple system atrophy must be differentiated, first of all, from “pure” Parkinson’s disease and other types of neurodegeneration. In addition to a standard neurological examination and medical history, tomographic imaging methods (CT, MRI) may be prescribed for diagnostic purposes (searching for and localizing areas of degeneration). More specific, “targeted” diagnostic methods for multiple system atrophy, whether hardware or laboratory analytical methods, have not been developed to date.
About our clinic Chistye Prudy metro station Medintercom page!
2. Reasons
We happen to live in an era when the rapid development of medical science is steadily reducing the number of both incurable diseases and diseases that are incomprehensible and etiologically unclear. Multiple system atrophy refers to both.
Despite research efforts - which are significantly hampered by the rarity of the disease and the variety of possible clinical presentations - the etiopathogenetic factors and mechanisms of multisystem neural atrophy are not yet known. In addition, it is not possible to identify statistical significance for any conditions or individual characteristics that could be called risk factors and, accordingly, preventive targets. Until recently, the results of attempts to decipher multiple system atrophy at the chromosomal level are hypothetical and speculative. The predominance of men among the sick has been reliably confirmed (according to various estimates, 1.5-2 times), but this trend has not yet received a satisfactory explanation.
Visit our Neurology page