Transcranial magnetic stimulation (TMS) is a research method in the field of neurology that makes it possible to induce depolarization or hyperpolarization in brain neurons. This technique is widely used in the Yusupov Hospital and makes it possible to study the excitability of cortical neurons, the interaction of different parts of the brain with each other, and the localization of functions in the cerebral cortex.
Transcranial magnetic stimulation of the brain: reviews
Transcranial magnetic stimulation of the brain in Moscow is a relatively new and very promising direction in medicine. Using this method, it is possible to map different cortical representations, which in itself is extremely important for understanding the functional organization of the human brain, as well as the mechanisms of its control.
Transcranial magnetic stimulation of the brain makes it possible to accurately determine the boundaries of the location of various brain functions, for example, the cortical representation of visual analyzers, speech centers, and memory.
Reviews of transcranial magnetic stimulation among doctors in Moscow and other Russian cities are positive, since the procedure allows the development of new approaches to the rehabilitation of patients with neurological diseases.
The procedure is very accurate, informative, effective and painless. The technique allows many people to get rid of serious diseases.
Indications for the use of transcranial and/or peripheral magnetic stimulation:
- Headache caused by neuralgia of the greater occipital nerve of the occipital nerve.
- Myofascial pain syndrome of the sternocleidomastoid muscle.
- Pain that occurs between the spinous processes of the cervical and thoracic vertebrae.
- Pain in the suprascapular region.
- Pain in the shoulder blade.
- Elbow pain.
- Carpal tunnel syndrome.
- Chest pain caused by the musculoskeletal system.
- Thoracolumbar syndrome.
- Pain in the lower back.
- Coxarthrosis of the hip joint.
- Pain in the gluteal region.
- Knee pain.
- Pain in the Achilles tendon.
- Foot pain.
- Multiple sclerosis and other demyelinating diseases.
- Cerebral atherosclerosis, diffuse vascular lesions of the brain.
- Consequences of injuries and injuries to the brain and spinal cord.
- Radiculopathy, myelopathy, damage to the cranial nerves (facial nerve neuritis).
- Parkinson's disease and secondary parkinsonism.
- Various dementias (Alzheimer's disease).
Cyclic transcranial magnetic stimulation of the brain
The technique is indicated for children with pathologies such as autism, encephalopathy with delayed speech development, and attention deficit hyperactivity disorder. The complex of transcranial magnetic stimulation and drug therapy helps improve speech, it becomes clearer, vocabulary increases, and children’s cognitive interest increases. Patients leave positive reviews about the effectiveness of the procedure.
At the Yusupov Hospital, neurologists use transcranial magnetic stimulation to treat complex diseases in adult patients aged 18+.
TMS has proven effective in treating depression, schizophrenia, and post-traumatic stress disorder.
Carrying out the TCM procedure
The transcranial magnetic stimulation procedure is performed under the supervision of a neurologist who has the appropriate knowledge, experience and necessary training. The TMS procedure can be performed on an outpatient basis.
For the greatest effectiveness of transcranial magnetic stimulation, a course of procedures (from 15 to 20) is necessary. Based on the opinion of a specialist, both a preventive and a therapeutic course can be prescribed. For each patient, a separate treatment protocol is approved by the specialist responsible for the procedure. The course of treatment is repeated after 30-90 days if necessary.
Preparation
Before the procedure of transcranial magnetic stimulation (TMS), it is mandatory to undergo all necessary checks for the presence of contraindications. As a rule, an EEG and an examination by a neurologist are sufficient. It is recommended that a few days before the procedure, you stop drinking alcohol, taking strong medical and narcotic drugs, as well as reduce physical activity and not change the treatment regimen, if any.
At the preparation stage, the neurologist individually determines how powerful, deep and long-lasting the penetration of the magnetic field should be. When everything is ready, the doctor will start the transmagnetic device.
Progress of the procedure
The patient is in a sitting position. An electromagnetic coil (coil) is applied to a certain area of the body (head, neck, lower back, legs or arms), which generates electromagnetic pulses for a certain period of time. The usual duration of the procedure is about 30 – 40 minutes. The sensations during the procedure are similar to “current slipping”; they should in no case be painful. The required level of pulse radiation is determined by the specialist performing the procedure.
Complications
The TCMS procedure has no consequences. The procedure is painless, there are no risks of deterioration in health. Usually all patients tolerate the procedure well.
The technique is used to treat patients with various diseases and lesions of the nervous system.
Highly qualified specialists provide examination of the patient, formation of an individual treatment protocol and rehabilitation course using this innovative method.
You can make an appointment for transcranial therapeutic magnetic stimulation by calling the All Medicine Clinic 240-03-03 or on our website.
Rhythmic transcranial magnetic stimulation
Rhythmic transcranial magnetic stimulation is a proven effective method for treating a number of diseases of the nervous system, successfully used in the Yusupov Hospital.
The technique is used in the treatment of the following pathologies:
- post-stroke pain syndrome;
- Parkinson's disease stage 3;
- trigeminal neuralgia;
- migraine;
- neuropathic pain;
- multiple sclerosis;
- spinal injury;
- tinnitus and others.
The clinical effect is observed after 10 therapy sessions, for depression - after 20. Experienced neurologists at the Yusupov Hospital, in combination with transcranial magnetic stimulation, depending on the individual characteristics of the patient’s body, can also prescribe medication and physical therapy.
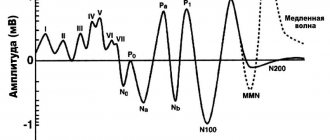
Transcranial magnetic stimulation (TMS) is a method based on stimulating brain neurons with an alternating magnetic field and recording responses to stimulation using electromyography [1]. Its essence lies in the occurrence of depolarization of the membranes of nerve cells under the influence of a strong magnetic field.
Rhythmic TMS (rTMS) is a type of stimulation that generates a series of pulses, the frequency of which varies from 1 to 100 Hz. There are two main rTMS modes: low-frequency (<1 Hz) and high-frequency (>5 Hz). Low-frequency magnetic stimulation causes a decrease in the excitability of neurons in the cerebral cortex, which leads to an inhibitory aftereffect, and high-frequency magnetic stimulation causes its increase, which has a stimulating effect [2, 3]. There are also “pattern” stimulation modes (intermittent theta burst stimulation - iTBS, continuous theta burst stimulation - cTBS), in which stimuli are presented in the form of specific clusters. The duration of the rTMS aftereffect is proportional to the duration of stimulation, the total number of stimuli and the frequency of sessions [4]. The physiological (therapeutic) effect of rTMS and long-term (up to 3 months) aftereffect are traditionally associated with changes in synaptic plasticity due to the phenomena of long-term potentiation and depression (LTP and LTD) [5].
The purpose of this work is to highlight the main possibilities of non-invasive brain stimulation using rTMS from the perspective of evidence-based medicine. When writing the review, we used data found in the PubMed database for the period from January 1994 to September 2014 (meta-analyses, protocols of large randomized, blind, placebo-controlled trials and European guidelines 2012-2014 on the safety and effectiveness of rTMS in neurology [ 6, 7]), as well as our own experience of using rTMS.
Neurorehabilitation after cerebrovascular accidents (CVA)
In theory, the use of non-invasive brain stimulation in post-stroke rehabilitation is associated with its ability to change the excitability and functional interaction of individual cortical regions. As is known, after NMC the interaction of the M1, PMC, SMA zones (primary motor, premotor, supplementary motor cortex) of both hemispheres changes significantly. By changing the excitability of these regions, it is possible to modulate the neuroplastic processes that occur after NMC.
The literature discusses the effect of non-invasive brain stimulation on the four main disabling symptoms of the patient after CMC: motor deficits, aphasia, spatial neglect and post-stroke spasticity.
1.1.
Motor deficit.
PubMed found 174 publications studying the effect of rTMS on motor functions after stroke in about 500 patients [8–10]. One of the first studies [11] showing the therapeutic effectiveness of low-frequency rTMS in the healthy hemisphere in this category of patients was carried out in 2005. Later, a large number of studies appeared [12-14] confirming this effect.
Some studies [15–17] have shown the effectiveness of high-frequency stimulation of the affected hemisphere in restoring motor functions in the acute and subacute stages of stroke. Additional studies have found that rTMS has the best effect when the ischemic focus is localized in subcortical formations compared to cortical lesions [18, 19]. The study [20] proved the effectiveness of bilateral stimulation (1 Hz - unaffected hemisphere; 10 Hz - affected) in patients with consequences of SCI. The Neuroscience Research Center is also currently conducting a blinded, placebo-controlled study of the effectiveness of rTMS, which shows that high-frequency stimulation of the affected hemisphere is superior for reducing spasticity; low-frequency stimulation significantly improves motor functions according to the Fugl-Meyer scale, and stimulation of both hemispheres leads to an increase in daily life activity according to the Barthel index [21, 22].
It has been shown [23, 24] that high-frequency rTMS of the motor representations of the pharynx and esophagus has a positive effect on swallowing function in post-stroke patients.
The situation with the pattern modes iTBS and cTBS remains uncertain. Some studies [25–27] established a positive effect of iTBS in the affected hemisphere. In contrast, in a controlled trial of 41 stroke patients [28], both regimens were ineffective.
Three meta-analyses have been published on this topic. One of them, which included 34 publications (392 patients), showed a significant reduction in the degree of arm paresis in response to rTMS [8]. At the same time, low-frequency stimulation of the healthy hemisphere was more effective than high-frequency stimulation. The best effect was achieved in patients with subcortical localization of stroke. In addition, the safety and effectiveness of iTBS in the affected hemisphere has been demonstrated. However, a 2013 meta-analysis [9], including 19 studies (588 patients), showed that these rTMS protocols were ineffective. A recent meta-analysis from 2014 [10], including 8 studies (273 patients), again showed that rTMS (both high- and low-frequency) significantly improved hand function and facilitated finger movements.
The totality of published data made it possible to assign evidence class B to the use of low-frequency stimulation of the M1 zone of the unaffected hemisphere in patients during the recovery period of a stroke (after 6 months); level C - high-frequency stimulation of the M1 zone of the affected hemisphere in patients in the acute and subacute stages of stroke and low-frequency stimulation of the unaffected hemisphere in the acute and subacute stages.
1.2.
Aphasia.
PubMed contains 75 case reports and several placebo-controlled studies. Most of them used low-frequency stimulation of the homologue of Broca's area in the right hemisphere.
A number of studies [29-31] have shown the effectiveness of TMS for various forms of aphasia, but others [32, 33] have not found significant differences between real stimulation of the right hemisphere and its imitation.
There are works [34] devoted to the use of exciting modes of stimulation of the affected hemisphere. Later, data were obtained [35, 36] that stimulation of the inferior frontal gyri of both hemispheres (low-frequency - right and high-frequency - left) also significantly improves speech functions. However, at present, there is still not enough evidence to make an unambiguous judgment about the effectiveness and place of rTMS in the rehabilitation of post-stroke speech disorders.
1.3.
Neglect syndrome.
Unilateral spatial neglect (neglect syndrome) occurs in 30% of stroke patients and significantly limits their rehabilitation. In open studies [37–40], low-frequency stimulation of the left parietal cortex showed a positive effect. The only placebo-controlled study [41] showed greater effectiveness of high-frequency stimulation of the right parietal cortex compared with low-frequency and sham stimulation in the acute period of stroke. In addition, a number of non-randomized clinical studies [42-44] have shown the effectiveness of cTBS of the left posterior parietal region in the treatment of neglect syndrome. The described studies allowed us to assign evidence class C to the cTBS stimulation protocol affecting the left posterior parietal region.
1.4.
TMS for the treatment of post-stroke spasticity.
In 2013, the only randomized, double-blind, placebo-controlled study was conducted [45], which showed the effectiveness of low-frequency stimulation of the M1 area of the unaffected hemisphere: in 90% of patients after completion of the course of stimulation and 55.5% during the subsequent 4-week observation period there was a decrease in spasticity >1 point on the modified Ashworth scale (MAS).
A study is currently being conducted at the Scientific Center of Neurology of the Russian Academy of Sciences [46], which shows a significant reduction in post-stroke spasticity with high-frequency stimulation of the affected hemisphere (frequency 10 Hz, 200 stimuli/session, 10 sessions).
There has not yet been a sufficient number of publications on the effectiveness of high-frequency stimulation to reduce cerebral spasticity, which necessitates additional studies to evaluate the effectiveness of various rTMS protocols in stroke patients.
Parkinson's disease (PD)
PudMed found 159 publications on the use of rTMS in PD, of which 15 were placebo-controlled studies, including 454 patients with PD. The main problem in their analysis is the extreme heterogeneity of patients with PD, even within the same study [6].
A meta-analysis of 10 publications (275 patients) [47] showed that high-frequency stimulation of the M1 and PMC areas is an effective method for improving motor functions in PD compared with low-frequency stimulation. In contrast, low-frequency stimulation impairs motor performance in PD, causing increased task completion time [48, 49] and increased rigidity [50]. Based on these data, the use of low-frequency stimulation of motor areas in PD is not recommended.
A significant improvement in movements was shown after subthreshold stimulation of M1 with a frequency of 5 Hz [51]. This effect was confirmed in 25 independent studies. The effect was achieved by stimulating both one hemisphere [50, 52-56] and both [57-59]. At the same time, there are negative results [60–63], which do not allow us to draw a conclusion about the unambiguous effectiveness of high-frequency unilateral stimulation in PD.
However, in these studies, the effectiveness of using standard 8-shaped coils for stimulation was assessed. The use of other types of coils (round or H-coil) allows for a less local, but more profound effect. The use of a round coil significantly increased walking speed during bilateral high-frequency stimulation of the M1 area [64]. It was shown [65] that there was a significant improvement in motor functions according to the UPDRS-III scale in 27 patients with PD who underwent high-frequency (10 Hz) rTMS on both sides using an H-coil on the M1 and dorsolateral prefrontal cortex (DLPFC).
Thus, the possible antiparkinsonian effect of rTMS in PD has been proven for high-frequency stimulation of the M1 area, preferably on both sides and with coils with an enlarged stimulation area (round, H-coils).
Focal dystonia (writer's cramp, blepharospasm)
PubMed found 44 publications on the use of rTMS for various forms of dystonia. Most of them involve the use of low-frequency protocols aimed at areas M1, PMC, primary sensory cortex (S1) and cingulate gyrus. However, all publications are difficult to compare and include a small number of patients.
Data on the effectiveness of low-frequency stimulation of the M1 area in patients with writer's cramp are ambiguous and cannot serve as a basis for confirming the effectiveness of this protocol for dystonia, since the studies included heterogeneous groups of patients and the stimulation modes were different [66, 67].
A non-randomized clinical study from 2010 [68] showed a significant improvement in motor functions in patients with writer's cramp after a single session of low-frequency stimulation of the S1 area. Patients with blepharospasm have shown [69] clinical improvement after low-frequency stimulation of the anterior cingulate cortex using a round or H-coil.
Thus, for focal forms of dystonia, low-frequency stimulation of the premotor cortex is a potentially effective protocol, but additional research is needed to clarify the level of evidence.
Pain syndromes
According to statistics, up to ½ of the entire adult population has ever experienced pain lasting more than 3 months, with 10 to 20% of patients suffering from clinically significant pain. Elements of chronic neuropathic pain occur in 6–8% of the adult population [70, 71]. Only in 30-40% of patients does pharmacotherapy achieve a sufficient analgesic effect (reduction in pain severity by more than 50% on a visual analogue scale - VAS) [72].
4.1.
rTMS in the treatment of chronic neuropathic pain.
There are 68 publications in PubMed, including 19 placebo-controlled studies, on the treatment of chronic neuropathic pain.
It has been demonstrated [73–79] that there is no significant analgesic effect with low-frequency stimulation of the primary motor cortex of the hemisphere opposite to the localization of pain. Low-frequency rTMS was ineffective in the treatment of chronic neuropathic pain (Evidence Level B).
Since 2001, 20 studies have been conducted to evaluate the effectiveness of high-frequency rTMS. Three studies (50 patients) showed that high-frequency rTMS was ineffective when stimulating the M1 area [77, 78, 80]. However, these studies used a round coil, which does not provide local effects on the stimulated area [81]. In the remaining studies, high-frequency rTMS was effective compared with placebo. However, in some studies only one session of rTMS was carried out, and the analgesic effect was assessed immediately after stimulation [73–75, 79, 82–86]. However, a more important result is evidence of the long-term analgesic effect of several successive sessions of rTMS for chronic neuropathic pain of various etiologies [87, 88] and phantom pain [89].
Several systematic reviews and meta-analyses have been published [75, 90–94] examining the effects of rTMS on chronic pain. They confirm the ineffectiveness of low-frequency rTMS and the effectiveness of high-frequency rTMS (pain reduction by more than 30% in 46-62% of patients and by more than 50% in 29% of patients), and note the possibility of obtaining a moderate long-term effect using a series of rTMS sessions. According to a meta-analysis by A. Leung et al. [92], both when assessed in general and when divided into groups depending on the etiology of the pain syndrome, a significant decrease in pain syndrome was noted in patients receiving rTMS compared to placebo. At the same time, the greatest analgesic effect was observed in patients with trigeminal neuralgia (decrease in VAS by 28.8%), somewhat less - in patients with central post-stroke pain syndrome (by 16.7%), spinal cord injury (by 14.7% ), damage to the spinal nerve root (by 10.0%) and peripheral nerve (by 1.5%).
The use of intermittent θ-burst (iTBS), which also increases neuronal excitability, has not been shown to be effective, except for one study in which high-frequency rTMS was preceded by θ-burst stimulation. This combined protocol was more effective compared to the isolated use of high-frequency stimulation [95].
Pilot data have also been published in Russia [96, 97], showing the effectiveness of high-frequency stimulation of the M1 zone of the contralateral pain localization of the hemisphere in the treatment of central post-stroke pain syndrome.
Thus, high-frequency rTMS of the primary motor cortex (M1) of the contralateral pain hemisphere can be recommended as an effective treatment method (Evidence Level A).
4.2.
Migraine.
There are few studies on the use of rTMS in the treatment of migraine [98–106]. A blind, randomized, placebo-controlled study of the effectiveness of rTMS in the M1 area of the left hemisphere in the treatment of migraine [105] showed a significant reduction in the frequency of migraine attacks, pain intensity, and the degree of disability of patients. Clinical improvement was associated with an increase in plasma β-endorphin levels.
R. Lipton et al. [106] showed the effectiveness of transcranial magnetic stimulation of the occipital lobes with single stimuli for the relief of a migraine attack accompanied by a visual aura. This quickly found application in clinical practice, with the development of a portable device that was approved for clinical use by the US Food and Drug Administration in 2014.
4.3.
Complex regional pain syndrome (CRPS) type 1.
CRPS combines sensory, motor and autonomic-trophic disorders, which were previously described as “reflex sympathetic dystrophy” and “causalgia”. CRPS type 1 usually develops after microtrauma or prolonged immobilization of a limb (splint, plaster, etc.). The pain syndrome of CRPS is neuropathic pain. In this regard, rTMS can be considered as a potentially effective method of pain relief in CRPS type 1.
Two randomized, placebo-controlled studies of rTMS in the M1 region were conducted [107, 108], which showed a significant reduction in pain immediately after the session, but the authors noted a large variability in the duration of this effect. Given this, high-frequency M1 rTMS may be recommended as a possibly effective treatment for CRPS type 1 (Evidence Level C).
4.4.
Fibromyalgia.
The effectiveness of rTMS in two areas was studied in patients with fibromyalgia: area M1 and DLPFC. In 2006, an open-label study was conducted [109], which showed the effectiveness of low-frequency rTMS of the right DLPFC in 4 patients. However, a similar study design [110] 3 years later found negative results, possibly due to the small number of stimuli per session. In a study by E. Short et al. [111] demonstrated a significant reduction in pain after 10 sessions of high-frequency stimulation of the left DLPFC in 20 patients compared to the placebo group.
A double-blind, randomized, placebo-controlled study of the effectiveness of high-frequency rTMS of the M1 area (2000 stimuli/session) [112] showed a significant reduction in pain and improvement in quality of life, which persisted for 1 month. Subsequently, it was proposed [113] to use “maintenance” sessions of rTMS in order to increase the duration of the long-term analgesic effect. Thus, there is evidence of the positive effects of rTMS, but the insufficient number of studies that meet the requirements of evidence-based medicine does not yet allow us to recommend any of the non-invasive brain stimulation protocols for the treatment of fibromyalgia.
Epilepsy
As is known, 20% of primary generalized and 60% of focal forms of epilepsy are drug-resistant [114].
PubMed found 102 publications on the use of rTMS in epilepsy, including five placebo-controlled studies. Conducted studies have yielded conflicting results. Of the five studies mentioned above [115–119], only two [117, 119] provided reliable data on a reduction in seizure frequency compared with the placebo group.
A 2011 meta-analysis [120], which included 11 placebo-controlled studies and 164 patients, concluded that there was a significant reduction in seizure frequency with low-frequency stimulation of the epileptic focus in patients with neocortical epilepsies and cortical dysplasias.
The published data, taking into account all the limitations, nevertheless made it possible to assign evidence class C (probably effective) to the low-frequency mode of stimulation of the epileptic focus when it is located in the cortex or in close proximity to the localization of the area of cortical dysplasia.
At the end of this section, recall that one of the principles of epilepsy treatment is continuity. It is known that in the case of drug therapy, irregular use of drugs can cause a worsening of the disease, up to the development of status epilepticus. The main limitation of the use of rTMS is that the duration of the course of stimulation is always limited, and the duration of the effect, as a rule, does not exceed 3 months. Thus, rTMS should be used with caution in drug-resistant epilepsy, and therapy adjustments should be made exclusively in conjunction with an epileptologist.
Tinnitus
Tinnitus (tinnitus) is the subjective sensation of sound of any frequency in the ear or head in the absence of an external sound stimulus. The prevalence of tinnitus among adults is approximately 10–15% [121, 122].
We found 111 articles in PubMed, including 20 placebo-controlled studies (601 patients). A 2010 study [123] performed low-frequency (1 Hz) stimulation of the primary auditory cortex in 42 patients with drug-resistant tinnitus. Both the simulation group and the active stimulation group showed a significant decrease in scores on the Tinnitus questionnaire immediately after rTMS sessions, however, in the simulation group this effect persisted for 2 weeks, while in the active stimulation group a similar effect was recorded for 14 weeks Another study [124] also showed the effectiveness of low-frequency rTMS of the superior temporal cortex in the treatment of tinnitus compared with placebo, and the duration of the effect was even longer - at least 6 months. In a study by E. Khedr et al. [125] used different stimulation protocols (1, 5, 25 Hz) of the left temporoparietal cortex. The treatment was effective regardless of the frequency of stimulation, but it was noted that the longer the duration of the disease, the less pronounced the effect of rTMS.
A 2011 systematic review [126] analyzed five large studies (233 patients). Only one placebo-controlled study showed a significant improvement in the quality of life of patients with tinnitus after low-frequency rTMS of the primary auditory cortex, while in the other two there was no significant difference between the groups. Two studies significantly reduced noise volume, but the total number of patients in these studies was small. Only one study showed a partial benefit of low-frequency stimulation (compared to high-frequency and sham) for up to 4 months.
Thus, low-frequency rTMS of the primary auditory cortex may be used as an alternative treatment for tinnitus (Evidence Level C), but additional research is required.
Spasticity
The generally accepted definition of spasticity was formulated by J. Lanz back in 1980 [127]: “a motor disorder that is part of the upper motor neuron lesion syndrome, characterized by a rate-dependent increase in muscle tone and accompanied by an increase in tendon reflexes as a result of hyperexcitability of stretch receptors.”
PubMed found 16 studies examining the effect of TMS on spasticity [46, 128–142]. Among all studies, only six are double-blind and have a control group [128–133].
7.1.
TMS for the treatment of spasticity due to spinal cord injury.
In 1996, it was first shown [139] that a decrease in the level of spasticity in the legs after high-frequency (25 Hz) stimulation at the level of the Th8 thoracic vertebra in patients with multiple sclerosis (MS). In 2007, similar results were obtained [140] in this category of patients with spasticity after high-frequency (5 Hz) stimulation of the M1 zone of the leg.
Further studies [128, 129] confirmed these results for patients with MS, incomplete spinal cord injury due to trauma, myelitis, and tumor.
In patients with MS, a decrease in spasticity of the stimulated leg was noted [131] when rTMS of the M1 zone was performed both in the iТВS mode and iТВS in combination with physical therapy.
The data obtained indicate the possible effectiveness of high-frequency stimulation of the M1 zone in the presence of a lesion at the level of the spinal cord (class C). However, given the low quality of the studies, additional, larger studies are needed to improve the level of evidence.
Depression
PubMed found 786 publications, including 61 placebo-controlled studies (3682 people).
The first studies of the effectiveness of rTMS in the treatment of depression [143, 144], which began in the 90s, used the vertex as a target for stimulation. However, in 1996, experiments on healthy volunteers [145] showed that stimulation of the prefrontal areas causes changes in mood.
The effect of rTMS on depression can be explained by the fact that stimulation of the prefrontal cortex with high-frequency rTMS can activate regulatory pathways connecting this area with the limbic system, which is responsible for emotional reactions and mood regulation. In 1997, a group of 12 patients showed the effectiveness of rTMS of the left dorsolateral prefrontal cortex compared with placebo [146]. In 2007, the results of a randomized placebo-controlled trial were published [147], which included 301 patients with treatment-resistant depression without supportive pharmacotherapy during stimulation. The effectiveness of long-term (20-30 sessions over 4-6 weeks) high-frequency (10 Hz, 120% of motor threshold 3000 stimuli/session) stimulation of the left DLPFC was shown compared with placebo.
The results were so convincing that a year later the FDA approved the use of this protocol in the treatment of unipolar depressive disorder in adults in the absence or insufficient effectiveness of the use of a single antidepressant at the minimum (or higher) therapeutic dose and duration during a given depressive episode.
Studies were also conducted in Russia [148], which confirmed the high effectiveness of the above protocol. In 2009, a meta-analysis was published [149], which included 30 double-blind, placebo-controlled studies and convincingly demonstrated the effectiveness of high-frequency stimulation of the left DLPFC compared with sham stimulation.
As an alternative to high-frequency rTMS, some researchers [150] proposed the use of low-frequency stimulation of the right DLPFC. However, the results of double-blind, placebo-controlled studies have been conflicting. Some studies have shown the effectiveness of this protocol, while others have not demonstrated significant differences compared to sham stimulation [151–154]. The reason could be the different power of the studies [155]. Meanwhile, the results of a meta-analysis did show [156] a significant decrease in values on classical scales for assessing depressive disorder after a course of low-frequency rTMS of the right DLPFC. In 2013, another meta-analysis was published [157], which showed significant effectiveness of this protocol, comparable to the use of antidepressants and high-frequency rTMS of the left DLPFC.
Based on the studies conducted, a level of evidence was established, A for high-frequency stimulation of the left DLPFC and level B for low-frequency stimulation of the right. Thus, today depression is one of the diseases in the treatment of which rTMS is undoubtedly effective, which is widely used in clinical practice abroad and in our country.
Anxiety disorder
More than 20% of people experience anxiety disorders during their lifetime [158].
Low-frequency stimulation of the right DLPFC has been shown to be effective in generalized anxiety disorder [159]; high-frequency - both left and right DLPFC in post-traumatic anxiety disorder [160]; high-frequency - left DLPFC and low-frequency - SMA zone in obsessive-compulsive disorder [161, 162]. In panic disorder, no significant differences were found compared to the sham stimulation group [163]. However, the quality of the research conducted is not high enough. Additional research is needed to develop recommendations for the use of rTMS in the treatment of anxiety disorders.
Currently, only for post-traumatic anxiety disorder there are recommendations (level C) for the use of high-frequency rTMS of the right DLPFC.
In the table, we summarized the therapeutic protocols of rTMS with proven effectiveness in the treatment and rehabilitation of diseases of the nervous system, as well as those that still require clarification. To date, the effectiveness of rTMS in the treatment of depression and neuropathic pain has been clearly established (level of evidence A); rTMS appears to be effective in neurorehabilitation for reducing motor deficits during stroke recovery (Evidence Level B). For diseases such as PD, tinnitus, CRPS type 1, epilepsy, spinal spasticity, and neuropathy, the effect of rTMS is virtually certain (Level of Evidence: C). The presented data allow doctors to recommend the use of rTMS in these conditions. Larger studies are needed to determine the place of rTMS in the treatment of conditions such as post-stroke speech disorders, various types of dystonia, migraine, and fibromyalgia.
Basic therapeutic TMS protocols recommended for use in clinical practice Note. Effect: A - definite, B - probable, C - possible.
Note that to prevent complications of rTMS, careful adherence to safety rules is required (more details can be found in the relevant recommendations [6] and on the website www.brain-stim.ru).
Prospects
In recent years, new generation technologies have emerged in the field of non-invasive brain stimulation—navigated TMS systems. Their main feature is the ability to localize the stimulation point on the MRI of a particular person and, with an accuracy of 2 mm, reproduce the same stimulation site every day during the entire course of treatment, which significantly increases the effectiveness of therapy and allows individual selection of protocols for stimulation based on the characteristics of the functional and anatomical brain structure and characteristics of the pathological process [164]. The use of navigation TMS seems to be the most promising in relation to the personalization of rehabilitation and treatment programs using non-drug methods of influence and control of neuroplasticity processes. Navigated TMS is described in detail in our review [165].
This publication was supported by RFBR grants No. 13−04−01139-A and No. 15−04−08686-A.
Transcranial magnetic stimulation: contraindications to its implementation
The method is not possible if the patient is suspected of having a cerebral aneurysm, has a pacemaker, or is pregnant. When diagnosing epilepsy, the method should be used with extreme caution, since transcranial brain stimulation can trigger the development of an attack.
Medicine does not stand still; scientific research is carried out every day, thanks to which new effective methods for treating many diseases emerge.
The Yusupov Hospital is equipped with modern medical equipment that allows the latest proven diagnostic and treatment methods to be applied in practice.
The hospital staff includes leading Russian doctors who are ready 24 hours a day, 7 days a week to provide patients with high-quality medical care that meets European standards. You can make an appointment at the hospital by phone.
Indications for transcranial electrical stimulation
- Treatment for alcoholism.
- Fighting drug addiction. By the way, while addiction to alcohol can be to some extent dealt with using medication (Disulfiram, Esperal, Aquilong, etc.), drug addiction until recently was treated exclusively by psychotherapy with drug support with antidepressants and sedatives. Thanks to TES of the brain, results can be achieved much faster and relapses can be avoided in the future.
- Relief of withdrawal symptoms. In this case, transcranial current stimulation can be used in parallel with a course of drug detoxification therapy.
- “Maintaining” metabolism, the functioning of all internal organs and systems against the background of complete abstinence from drugs and alcohol.
- Stimulation of metabolic processes to cleanse tissues of residual products of the breakdown of ethyl alcohol and psychoactive substances.