Definition
Benign paroxysmal positional vertigo (BPPV) occurs in repeated episodes, often lasting less than one minute. Attacks are triggered by changes in head position: turning, throwing back, as well as changes in body position, including lying down, even in sleep. Between attacks, autonomic disturbances (nausea, rarely vomiting, fluctuations in blood pressure, sweating) and imbalance may persist, so patients may describe constant dizziness.
Over time, the severity of attacks usually decreases. The word “benign” means that the disease goes away on its own, without treatment, without causing lasting harm to the patient.
BPPV is the most common type of dizziness. Attacks most often develop in older women. However, the disease can occur at any age.
Attacks of BPPV, in most cases, are associated with separation, destruction or increase in size of the otoliths.
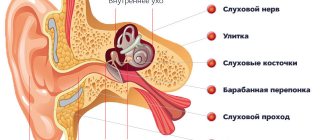
Otoliths (otoconia) are layered pebbles consisting primarily of calcium carbonate crystals, like mother of pearl or nacre. They are immersed in a jelly-like layer that envelops the hairs of sensitive cells on the surface of the macula (macula) of the spherical and eleptic sacs of the vestibular analyzer. The otoliths, the jelly-like layer and the hairs of sensory cells form the otolithic membrane.
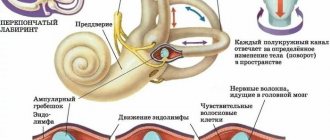
The elliptic sac (uterus) connects to three semicircular tubules (SCC), located in three perpendicular planes: lateral, anterior and posterior. In their extensions at the junction with the uterus, there is also a sensitive area - the ampullar ridge, covered with a structure similar to the otolithic membrane - the cupula. Normally, the cupula separates the RCC and the utricle. It does not contain otoliths. The cupula provides the perception of angular accelerations of the head, responding to changes in pressure in the ampulla arising due to the inertia of the endolymph (the fluid that fills the RCC and the sacs of the vestibular analyzer).
Detached otoliths or fragments thereof may enter the ampullae of the RCC and irritate the cupular areas. This more common variant of BPPV is called canalithiasis.
Thanks to the balance between the formation and resorption of the layers that make up the otoliths, their renewal is ensured, as well as the resorption of detached otoliths. When the balance is disturbed, one of the otoliths becomes large (2-4 times larger than neighboring cells); the large mass leads to greater displacement compared to neighboring fixed otoliths, which is a source of irritation of the vestibular system. This variant of BPPV is called dome lithiasis; it is characterized by a longer course (several months) and lack of effect from vestibular maneuvers.
Asymmetrical signal input to the brain during unilateral stimulation of the vestibular apparatus disrupts the illusion of balance created by the interaction of the vestibular, visual and proprioceptive systems (receiving signals from muscles and ligaments, assessing the position of limb segments). There is a feeling of dizziness.
Sensitive cells of the vestibular analyzer send a signal of maximum intensity to the brain during the first second of stimulation, then the signal strength decreases exponentially, which underlies the short duration of BPPV symptoms.
The most common lesion is the posterior SCC (90%), less often the lateral one (8%), the remaining cases are caused by damage to the anterior SCC and combined damage to several tubules. Classic cases of BPPV due to posterior RCC involvement are idiopathic in 35% of cases, with previous traumatic brain injury (sometimes minor) and whiplash in the neck occurring in 15% of patients.
In other cases, BPPV is caused by other disorders: most often Meniere's disease (30%), vestibular neuronitis, surgical interventions on the organ of hearing, paranasal sinuses, herpetic lesions of the ear ganglion and circulatory disorders of the structures of the inner ear. Population studies have revealed a direct relationship between the likelihood of developing BPPV and age, female gender, migraine, giant cell arteritis, risk factors for cardiovascular complications - arterial hypertension and dyslipidemia, as well as a history of stroke, which confirms the importance of vascular causes in some cases.
Lindsay-Hemenway syndrome has been identified - acute dizziness, followed by the development of BPPV attacks and a decrease or complete disappearance of nystagmus in the caloric test due to circulatory disorders in the anterior vestibular artery system.
The diagnosis of BPPV is made based on the assessment of nystagmus during special maneuvers - techniques that cause angular accelerations of the patient's head.
Damage to the posterior semicircular tubule
The Dix-Hallpike test is the “gold standard” for diagnosing BPPV caused by posterior SCC pathology:
- The patient sits straight along the couch, with his head turned 45˚ towards the labyrinth that is being examined.
- The patient is placed in a lying position, while the head rotation is maintained, the head is thrown back at an angle of 30˚ relative to the axis of the body, and hangs over the edge of the couch.
- Watch eye movements. Nystagmus and dizziness occur with a delay of several seconds and last less than 1 minute. Nystagmus has a typical trajectory: first, a tonic phase occurs, during which the eyeball is moved upward, away from the underlying ear, a rotatory component is noted, then clonic eye movements toward the floor occur. the underlying ear.
- After the nystagmus stops, the patient is returned to a sitting position and the eye movements are observed again; the nystagmus may reappear, but in the opposite direction.
When the test is repeated with turning the head in the same direction, the intensity and duration of the nystagmus decrease each time.
The procedure is repeated with the head turned in the opposite direction.
The affected side is determined by which side positional nystagmus and dizziness occur.
Symptoms of dizziness
Patients usually complain of dizziness
when lying down, when turning in bed or when throwing back the head. For this reason, dizziness is worse in the morning. The attack usually passes quickly and rarely lasts more than a minute. However, after an attack, patients often experience random dizziness, weakness, or a feeling of unsteadiness for several hours or even days.
Sometimes severe dizziness
occurs at night, during sleep, causing the patient to wake up.
Dizziness
may be accompanied by nausea and vomiting. The disease has a benign course: periods of exacerbation, when attacks are repeated daily, followed by spontaneous remission, which can last several years.
Damage to the lateral semicircular tubule
A lesion of the lateral RCC is detected with the patient lying down by turning the head in the plane of the canal from right to left and vice versa (roll test). Horizontal nystagmus occurs, with a clonic component directed downward, mainly when the affected ear is turned downward; if the healthy ear is located below, nystagmus also occurs, the clonic component of which is directed downward, but less pronounced.
In a quarter of patients, canalolithiasis in the lateral RCC is combined with canaloliasis in the posterior RCC. In contrast to downward-directed nystagmus, the clonic component of evoked nystagmus is directed toward the overlying ear. This form is combined with the location of otoliths in the anterior part of the lateral ACC or the otolith fixed to the cupula, while with freely moving otoliths, nystagmus occurs directed towards the underlying ear.
Test results may be influenced by cervical spinal canal stenosis, radiculopathy of the cervical segments of the spinal cord, severe kyphosis, restrictions of movement in the cervical spine: rheumatoid arthritis, ankylosing spondylitis, Paget's disease, spinal cord injury, morbid obesity, Down syndrome. In this case, it is possible to use a Barany swivel chair.
If the test results are negative, a preliminary diagnosis of BPPV is made based on complaints of positional vertigo and is confirmed by successful performance of vestibular maneuvers.
If examination reveals a nystagmus that differs from that described above, as well as other neurological symptoms, it is necessary to exclude other lesions of the nervous system.
A number of types of dizziness and nystagmus appear only when the position of the head in space changes - they are positional.
Nystagmus and rotational vertigo can cause both central (for example, associated with damage to the brain stem or cerebellum) and peripheral (canalolithiasis, vestibular neuronitis, damage to the ear ganglion, perilymphatic fistula) lesions of the vestibular analyzer, as well as combined damage to central and peripheral structures - meningitis, intoxication.
Dizziness can be caused by circulatory disorders: thrombosis of the vestibular arteries, migraine, orthostatic hypotension, paroxysmal heart rhythm disturbances.
The relevance of the differential diagnosis of these causes is due to the fact that the central forms require special intervention.
The most commonly ordered test is an MRI of the brain. In some cases, diagnosis may require an orthostatic test, blood pressure and ECG monitoring, duplex scanning of the brachiocephalic arteries/transcranial Doppler sonography, radiography of the cervical spine, and an ophthalmological examination.
Positional maneuvers are also used to treat the patient. Treatment is carried out with the participation of a doctor and takes into account the location of the otolith according to the diagnostic maneuver.
Damage to the posterior semicircular tubule
Epley maneuver
The most studied is the Epley maneuver. It is used for pathologies of posterior and lateral SCC:
- The patient sits straight along the couch, with his head turned 45˚ towards the labyrinth that is being examined.
- The patient is placed in a lying position, while the head rotation is maintained, the head is tilted back slightly, hanging over the edge of the couch.
- After 20 seconds, the head turns to the healthy side by 90˚
- After 20 seconds, the head is turned in the same direction by 90˚ along with the patient's body, so that the face is facing down.
- After 20 seconds, the patient returns to a sitting position.
- The Simon maneuver is also used to treat posterior RCC lesions:
- In a sitting position, turn the head 45˚ towards the “healthy” ear, for example the right one
- The patient is quickly placed on his left side (head face up), an attack of dizziness occurs with rotatory nystagmus to the left, the position is maintained for 3 minutes. During this time, the otoliths descend to the lowest part of the RCC.
- Quickly turn the patient onto his right side (head face down). Maintain the position for 3 minutes.
- The patient is slowly returned to the starting position.
The fixed otolith resolves within a few weeks. The same amount of time is required for attacks of dizziness to disappear during the natural course of the disease.
According to research by Casani A.R. et al. (2011) the average duration of dizziness with damage to the posterior ACC was 39 days, with damage to the lateral ACC - 16 days.
Manipulations are often accompanied by a sharp temporary increase in the symptoms of the disease: dizziness, nausea, vegetative symptoms.
After the maneuver, the patient must be monitored after 3 days and 1 month, which will allow the maneuver to be repeated if it is ineffective or to promptly begin a search for other causes of dizziness if new symptoms appear.
Relapses occur relatively rarely (3.8 - 29% of cases).
Brandt-Daroff gymnastics
If the maneuvers performed by the doctor are ineffective, patients with damage to the posterior RCC are recommended to perform Brandt-Daroff gymnastics on their own:
- In the morning, after sleep, sit on the bed with your back straight (Position 1)
- Then you need to lie on your left (right) side with your head turned up at 45° (to maintain the correct angle, it is convenient to imagine a person standing next to you at a distance of 1.5 meters and keep your gaze on his face) (Position 2)
- Hold this position for 30 seconds or until the dizziness disappears
- Return to the starting position sitting on the bed
- Then you need to lie on the other side with your head turned up 45° (Position 2)
- Stay in this position for 30 seconds
- Return to the starting position sitting on the bed (Position 1)
Repeat the described exercise 5 times.
If dizziness does not occur during the exercise, it is advisable to perform it only the next morning. If dizziness occurs at least once in any position, then you need to perform the exercises at least two more times: in the afternoon and in the evening.
Treatment of BPPV
BPPV often goes away on its own before seeing a doctor. About 20-28% of patients with BPPV experience spontaneous resolution of symptoms within 1 month.
Therapeutic tactics involve using a certain sequence of head turns (repositioning maneuvers), during which the otoliths move from the affected canal back to the vestibule of the labyrinth.
If repositioning maneuvers are insufficiently effective, the patient may be additionally recommended to perform the necessary set of exercises at home.
Surgical treatment is used only when maneuvers are ineffective, when BPPV disables the patient.
According to various studies, the risk of BPPV recurrence is 15% during the first year and 37-50% over the next 5 years.
How is BPPV treated at the Rassvet clinic?
Since BPPV is a mechanical disease, its treatment is based solely on repositioning maneuvers. For severe nausea and vomiting, antiemetics may be prescribed.
We do not prescribe vascular therapy, homeopathic remedies or other medications and treatments (acupuncture, osteopathy) with unproven effectiveness to patients with BPPV.
Specific prevention of the disease has not yet been developed. The relationship between BPPV and vitamin D deficiency is currently being actively studied.
Author:
Chekaldina Elena Vladimirovna otorhinolaryngologist, Ph.D.
Exercises for lesions of the lateral ACC
Vannucchi extended position method
Lying on your side with the affected ear facing up for 12 hours,
Barbecue method
The “barbecue” method - turning the patient 360˚ - the patient in a lying position is successively turned towards the healthy ear by 90˚ until he takes the starting position.
Lampert and Tiel-Wilck method (in the video above - a maneuver for damage to the right ear)
The patient's head is rotated 270˚ from the affected ear to the healthy one.
Special studies have shown the sufficient effectiveness of exercises performed by patients. There were no differences in the effectiveness of the maneuver in specialized clinics and in primary care settings.
Drug treatment
There are no drugs that have a direct effect on canal/cupolothiasis.
Drug treatment is advisable only for frequent attacks or during maneuvers.
Drugs are used that reduce the excitability of the vestibular system, both selectively and through a general sedative effect. The first include drugs with a vestibulolytic effect - blockers of H1 and H3 histamine receptors, cinnarizine, atarax, first generation antihistamines - diphenhydramine, pipolfen.
Evidence has been obtained in favor of reducing the intensity of dizziness when performing the Epley maneuver simultaneously with taking betahistine 24 mg x 2 times a day for a week.
Sedatives, most commonly benzodiazepine tranquilizers (diazepam), are used in hospital settings for the symptomatic treatment of severe recurrent attacks.
Treatment
Conservative therapy
The goal is to eliminate or minimize discomfort, correct disorders that provoke the occurrence of symptoms. Treatment tactics are determined depending on the cause and mechanism of development of severe dizziness:
- Pathologies of the inner ear
. Taking into account the clinical situation, diuretics, antihistamines and vasodilators, anticholinergics, antipsychotics, vitamins B and C, iodine, bromine and calcium preparations are prescribed. For BPPV, training of the vestibular apparatus is indicated. Patients are taught special techniques (Ellie, Simonta) to change the position of the otoliths and eliminate unpleasant manifestations. - Arrhythmias
. Complete atrioventricular block is relieved with M-cholinergic receptor blockers. In the interictal period, the underlying disease is treated. NSAIDs, antibacterial, antiviral and antianginal agents, antiplatelet agents, and glucocorticoids can be used. - TIA
. Antiplatelet agents and indirect anticoagulants are indicated. Hemodilution is performed with dextran, glucose solution, and saline solutions. Stabilize blood pressure with antihypertensive medications. To improve cerebral circulation, cinnarizine and vinpocetine are prescribed. Neurometabolic therapy is carried out. - Temporal lobe epilepsy
. To reduce the frequency of attacks and achieve a state of remission, monotherapy with carbamazepine, barbiturates or valproate is performed at the initial stage. If monotherapy is ineffective, they switch to the simultaneous use of several drugs. - Panic attacks
. Combinations of medicinal and non-medicinal methods are recommended. Patients are referred for psychotherapy and taught breathing control. As part of drug therapy, long courses of tricyclic and tetracyclic antidepressants are indicated. To reduce the severity of side effects in the first weeks of use, antidepressants are combined with benzodiazepines.
Physiotherapeutic techniques are sometimes used: electrosleep, oxygen therapy, massage, circular shower, microwave therapy. For diseases of the labyrinth during the period of remission, medicinal electrophoresis, darsonvalization, ultraviolet irradiation, pine and sea baths are effective.
Surgery
The surgical option is chosen taking into account the cause of severe dizziness:
- Diseases of the inner ear
: tympanotomy with closure of the perilymphatic fistula, reduction of pressure in the endolymphatic space by fenestration of the semicircular canal, perforation of the base of the stapes, drainage, laser destruction of the labyrinth. - Epilepsy
: temporal resection, sometimes amygdalotomy, selective hippocampotomy or focal resection. - Arrhythmias
: installation of a single-chamber or dual-chamber permanent pacemaker.