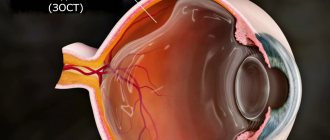
Retinal angiopathy develops against the background of organic and functional disorders of the fundus vessels. They lead to circulatory failure and subsequent degeneration of retinal tissue. Most often, angiopathy is a secondary pathology that develops against the background of other ophthalmological or general systemic diseases.
Causes of angiopathy
The following diseases can lead to disruption of the vascular system of the eye:
- hypertension or hypotension;
- atherosclerosis;
- diabetes mellitus and other endocrine disorders;
- eye injuries;
- autoimmune diseases;
- genetic predisposition.
In most cases, disorders of the vascular system affect the entire body, and angiopathy is combined with other diseases. Only angiopathy of traumatic origin can be local in nature.
The developing pathology causes serious functional and trophic disorders of the tissues and structures of the eye:
- dystonia of the vascular wall;
- vascular spasms;
- formation of atherosclerotic plaques;
- thrombosis of veins and capillaries.
Angiopathy always carries the risk of ischemic changes in the retina. Dysfunction of the circulatory system leads to slow metabolism, accumulation of metabolic products in tissues and hypoxia. Over time, this causes degeneration and functional failure of the light-sensitive cells of the eye and, as a consequence, loss of visual acuity.
Causes of angiopathy
There is a huge list of reasons leading to the development of angiopathy in both eyes. Here are just a few of them:
- diabetes;
- smoking;
- blood diseases;
- osteochondrosis of the cervical spine;
- arterial or intracranial hypertension;
- diseases of the nervous system;
- hypotension or hypertension;
- autoimmune diseases;
- injuries;
- heredity;
- elderly age.
All changes impair the nutrition of the retina, resulting in oxygen starvation.
Types of retinal angiopathy
The classification of angiopathy is based on etiology. There are 5 types of angiopathy:
Hypertensive. General vascular disorders in hypertension affect the functioning of the veins and capillaries of the fundus. The retina that feeds from them does not receive the necessary substances in full and accumulates metabolic products. This causes tissue degeneration, functional failure of light-sensitive cells, and then irreversible organic changes. Angiopathy caused by vascular hypertonicity is further complicated by atherosclerotic changes in the lumen of blood vessels.
Hypotonic. Constantly low pressure in the vascular system is also not beneficial, since low tone causes slower blood flow. The consequence of this is sluggish metabolism, nutritional deficiency and general functional weakness of both the eye muscles and light-sensitive elements.
Diabetic. Elevated blood glucose levels have a toxic effect on the walls of blood vessels. Their elasticity and permeability are impaired. Diabetes is often accompanied by atherosclerosis, which causes the formation of plaques that narrow the lumen of blood vessels, which also impairs trophism.
Traumatic. Impaired blood supply to the fundus can be caused by mechanical damage. Especially often, angiopathy develops after traumatic brain injury and as a result of a violation of the integrity of the upper parts of the spine.
Youthful. Angiopathy that occurs before the age of 30 is considered “youthful.”
The reasons for such early development of pathology, as a rule, are chronic, sluggish infections (toxoplasmosis, tuberculosis and others). Over time, the disease leads to vasculitis - inflammatory changes in the vascular system. The consequence of this is insufficient blood supply and retinal dystrophy.
What is diabetic angiopathy: features of the disease
In simple terms, angiopathy in diabetes mellitus occurs due to the inability of blood vessels to pass blood in the same volume as it was before the onset of diabetes. Problems with sugar impair their elasticity, after which blockage develops. As a result, blood circulation in the legs deteriorates so much that motor function suffers:
- Every movement leads to painful sensations.
- The feet become numb, making it difficult for a person to walk.
- Ulcerative lesions form.
Ultimately, the tissues of the lower extremities die, necrosis develops, and hence the need for amputation arises. But even this is where the deterioration of the condition due to angiopathy does not end. Blood circulation in the body is a holistic and unified process. So gradually the disorders affect the eyes, kidneys, and heart.
Symptoms of angiopathy
Developing angiopathy may not manifest itself for a long time. This complicates diagnosis in the early stages. Most often, the disease is detected by complications that have already arisen, which give clear symptoms. Only with further research does it become clear that the disorders are secondary, and the underlying cause was the existing angiopathy.
Characteristic symptoms in the presence of angiopathy may be:
- episodic blurring of the visual field;
- headache;
- unpleasant and painful sensations in the eye area;
- loss of visual acuity;
- narrowing of the field of view, loss of peripheral vision areas.
These symptoms in any combination are a serious reason for immediately contacting an ophthalmologist. Even if the cause is not angiopathy, such disorders indicate existing organic disorders or developing pathological processes.
Causes
Diabetic angiopathy is a complication of diabetes mellitus. It manifests itself as vascular damage leading to ischemia of the lower extremities. In its morphological essence, the cause of vascular damage is atherosclerosis. Even young people with diabetes are susceptible to diabetic angiopathy, while symptoms of atherosclerosis are more often noted in older patients. Vascular lesions are multisegmental in nature and rapidly progress. The approach to the treatment of both diseases is also different: drug treatment of atherosclerosis involves taking thrombolytic drugs, but with angiopathy of the lower extremities they help little.
In patients with diabetes mellitus, atherosclerosis of the arteries of the extremities develops much faster. Often its progression is recognized at the stage of complete blockage, i.e. vascular occlusion. This is due to the fact that the initial stages of many diabetes diseases are asymptomatic. Diabetic angiopathy affects small arterial vessels that nourish working cells. Obstruction of small and medium-sized arteries is fraught with tissue death.
Diagnostics
Even completely healthy people are recommended to have an annual preventative visit to an ophthalmologist. If you have risk factors, you should visit your doctor twice a year. This is especially important for identifying angiopathy and other eye diseases that do not have obvious symptoms in the early stages. Many of them have a favorable prognosis only with timely treatment.
The basis for diagnosing angiopathy is examination of the fundus. At the same time, even minor disorders are quickly and painlessly identified, threatening serious complications in case of untimely treatment.
Our ophthalmological center carries out a full range of diagnostic measures aimed at early diagnosis of angiopathy. After examining the fundus, experienced doctors, if necessary, conduct a more thorough examination using modern equipment. To clarify the diagnosis, the following may be prescribed:
- duplex study of brachiocephalic vessels;
- Ultrasound of the eyeballs;
- other hardware and instrumental methods for studying the vascular system of the eye.
How to cure retinal angiopathy as quickly as possible?
We offer an innovative method of color pulse therapy, the discovery of which was awarded the Nobel Prize.
The answer is obvious: in order for the visual system to work correctly, it is necessary to debug the normal functioning of the brain centers responsible for its regulation. This is exactly the problem that the innovative Neurodoctor device solves.
The device is based on the pulse therapy method. This treatment method is considered modern medicine, one of the most progressive and highly effective. Pulse therapy affects certain centers of the brain and activates certain areas of the visual system, eliminating malfunctions in their functioning.
How it works?
Neurodoctor affects the control centers of the brain.
The brain begins to produce dozens of neurohormones and form “corrective” nerve impulses.
Neurohormones are many times more effective than the most powerful drugs in quickly curing the disease. Nerve impulses eliminate pathological processes at the cellular level and correct the functioning of other organs and systems of the body.
LEARN MORE ABOUT THE METHOD
Treatment of angiopathy
The first task in the treatment of angiopathy is to identify and eliminate the negative factors that served as the background for the development of the disease. As a rule, these are chronic diseases. It is necessary to monitor blood pressure and prevent hypertensive crises. Diabetics must maintain optimal blood sugar levels. These measures are ensured by appropriate treatment regimens prescribed by specialized specialists. The ophthalmologist monitors how the treatment affects the blood vessels of the eyes, and also prescribes treatment aimed at eliminating hypoxia, normalizing the blood supply to the optic nerve head, and strengthening the walls of the blood vessels of the eye. Vitamins, antioxidants, neuroprotectors and mineral complexes can also provide good support to tissues experiencing dystrophy.
Specialists of the Moscow Ophthalmological Center will offer an individual treatment regimen, which may include drugs in the form of:
- tablets;
- injections;
- parabalbar injections into the eye area;
- intravenous drips.
Additionally, hardware treatment programs, physiotherapeutic procedures and massage are prescribed.
Surgical care can be aimed mainly at eliminating complications that have already developed. Most often, laser surgery is used to treat and prevent retinal detachment caused by angiopathy.
Angiopathy - Types
Depending on the diameter of the capillaries affected by the pathological process, the following types of angiopathy are distinguished:
- Macroangiopathy – develops with atherosclerotic vascular damage. Has a severe course. Macroangiopathies usually develop in the vessels of the heart and lower extremities.
- Microangiopathy means damage to small vessels by a pathological process, developing as a result of necrosis, thrombosis, hyalinosis, fibrinoid swelling. Microangiopathies include damage to the vessels of the retina of the eyeball, as well as damage to the capillaries of the kidneys.
The most common diabetic angiopathy occurs in patients with diabetes mellitus. Vascular lesions can have different localizations. Most often affected:
- Renal vessels (diabetic nephropathy);
- Retinal vessels (diabetic retinopathy);
- Vessels of the lower extremities.
Hypertensive angiopathy is also distinguished. This disease develops during the progression of hypertension and is most clearly manifested in the fundus. In the opposite condition (hypotension), hypotonic retinal angiopathy develops.
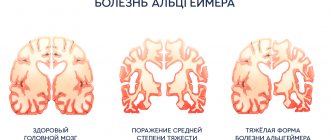
Morel's dysoric angiopathy develops in Alzheimer's disease and senile dementia. This disease is characterized by a combination of amyloidosis of the walls of arteries and arterioles, and the formation of senile plaques. There are two forms of the disease: drusen and congophilic.
Mostly young men develop Ila disease or proliferating retinitis. This disease is characterized by the development of cataracts, multiple hemorrhages in the retina and vitreous body. As juvenile angiopathy progresses, glaucoma appears and the retina of the eyeball becomes detached.
What are the causes of the disease?
Most angiopathy is associated with the development of diabetes mellitus. The pathological process aggravates the course of the underlying disease.
The causes of retinal angiopathy can be both diabetes and blood diseases, hypertension, trauma, smoking, pregnancy, autoimmune diseases, and intoxication.
Cerebral amyloid (CAA) is a consequence of senile dementia or Alzheimer's disease.
Hypertension causes increased blood pressure.
Striatal angiopathy of newborns is the result of lining of the brain vessels with calcium formations
Treatment
In ophthalmological practice, conservative treatment of angiopathy is predominantly used. The main measure to restore microcirculation and blood supply to the organs of vision was and remains the elimination of the underlying disease, against the background of which changes in the vessels of the fundus occurred:
- in the diabetic form, patients are prescribed drugs to stabilize blood glucose, insulin, and are also recommended to follow a low-carbohydrate diet;
- in case of hypertensive form, medications are prescribed to lower blood pressure and strengthen blood vessels;
- for angiopathy caused by inflammatory processes in blood vessels, a complex of drugs with anti-inflammatory, regenerative, and antithrombotic effects is prescribed.
Timely initiation of therapy for the underlying pathology leads to the leveling of factors provoking angiopathy and restoration of blood supply to the retina.
To improve the condition and functionality of the fundus of the eye, the ophthalmologist may prescribe additional medications:
- microcirculation stimulants - “Piracetam”, “Vazonit” and their analogues;
- agents that strengthen the walls of blood vessels and reduce their permeability - Parmidin, preparations with ginkgo biloba;
- drugs that prevent blockage of blood vessels by blood clots - Pentoxifylline, aspirin, Ticlopidine and their analogues;
- vitamin complexes containing substances of group B, antioxidants (vitamins A, C, E);
- local products with vitamins, lutein, anthocyanins - “Taufon”, “Anthocyan Forte”, “Emoxipin” and their analogues.
To improve the patency of blood vessels in the head area, drugs to lower cholesterol levels (Atorvastatin or Pravastatin) are prescribed. These medications are especially important for patients with hypertensive angiopathy.
Physiotherapeutic procedures are used to improve retinal nutrition, enhance microcirculation and strengthen blood vessels. If the problem is changes in the eye vessels, magnetic therapy and laser treatment are used. When the disease is provoked by “clamping” of blood vessels and nerves in the cervical or thoracic spine, electrophoresis and acupuncture are used.
A special diet will also help support the retina. The patient's diet should become less caloric. Sources of solid animal fats, salt, and light carbohydrates should be excluded from it. You also need to reduce the amount of spices, especially hot ones, with a strongly pronounced piquant taste. Remove all types of alcohol from the menu, as alcoholic beverages negatively affect the condition of blood vessels and provoke thrombosis.
To maintain the retina, it is necessary to enrich the diet with foods rich in vitamins and microelements that are good for the eyes: carrots, pumpkin, garlic, red fish, sweet colored peppers, berries and fruits colored blue or purple. They contain anthocyanins - substances that strengthen the walls of blood vessels and improve the trophism of light-sensitive tissues of the eyes. Additionally, you can use special fortified complexes for vision. Children are prescribed physiotherapy with the Sidorenko Glasses device.
Special physical exercises help keep blood vessels in good shape, strengthen the heart and improve blood supply to the eyes. The type and intensity of training depends on the underlying disease, general health and the degree of changes in the retina. The doctor may recommend daily restorative exercises, eye exercises, yoga, and swimming. Long, measured walks in the fresh air will certainly be useful.
Angiopathy: so different, so dangerous
What is meant by diagnosis
Angiopathy is a pathological condition of blood vessels in which the tone or structure of the vascular wall changes.
It occurs in various diseases, including as a dangerous complication. There are the following main types:
- Diabetic
- Amyloid cerebral
- Retinal angiopathy
Less common are hypertensive, hypotonic, traumatic, striatal (newborns). Each has its own characteristics in diagnosis, course, causes and therapy.
The disease affects both small blood vessels (then we are talking about microangiopathy) and large ones. Angiopathy of the arteries usually develops in the lower extremities, heart, brain and is severe. Macroangiopathy is usually caused by diabetes and atherosclerosis.